  |
A 42-year-old male presents for contact lens fitting secondary to post-refractive surgery corneal ectasia OU. He has a history of LASIK OU, after which he developed ectasia OU. More recently, he underwent corneal crosslinking (CXL) on his right eye only, as stromal scarring and significant thinning was noted in the left eye. He presents wearing his habitual rigid gas permeable (RGP) contact lenses and reports his left lens never feels stable on his eye; thus, his goals are to have the best vision possible and to improve lens comfort.
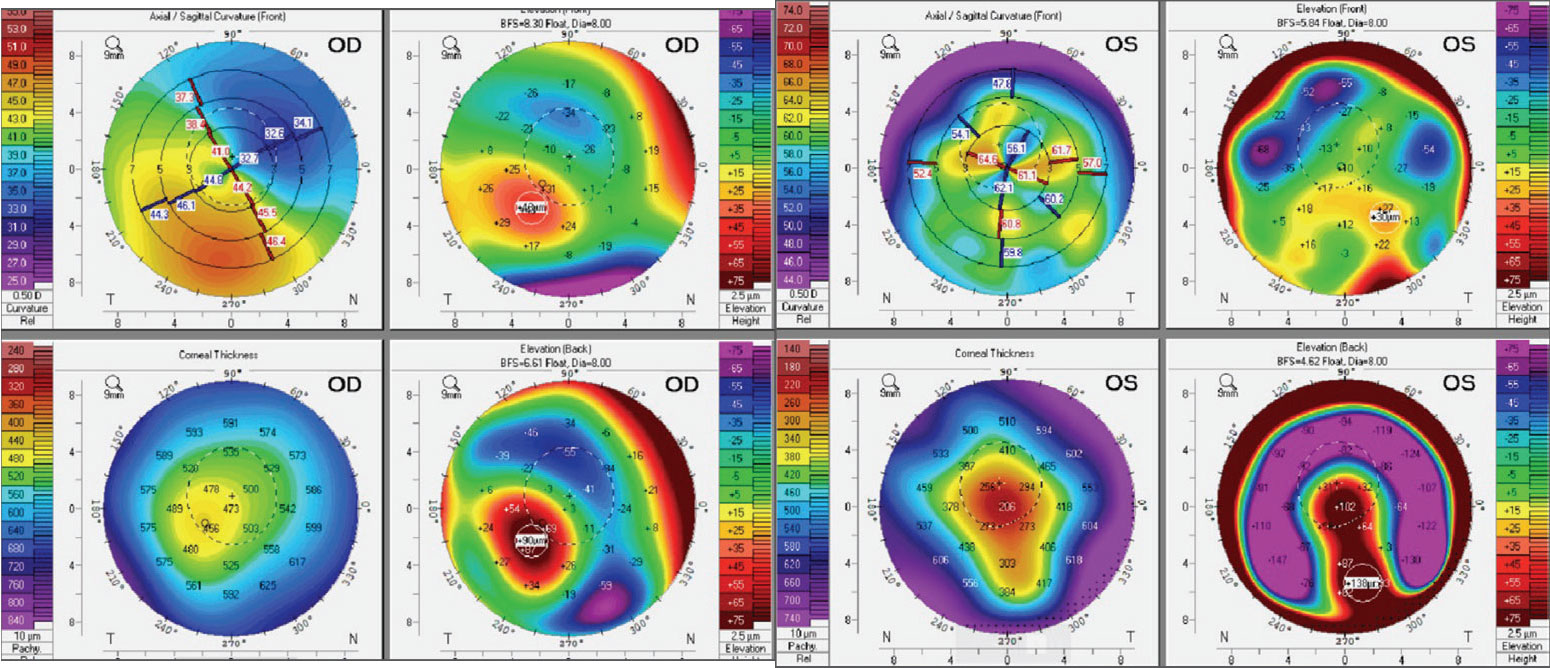
Manifest refraction is -3.50 -5.00x035 OD and -4.50 -4.50x045 OS with visual acuities (VA) of 20/25 OD and 20/400 OS. The slit lamp revealed epithelial irregularity over the corneal scarring OS, 1+ superficial punctate keratopathy inferior OU and 1+ three and nine o’clock corneal and conjunctival staining worse OS. The right lens shows a lid attachment fit with movement of 1.0mm and good centration. However, the left lens shows an interpalpebral fit with harsh touch over the apex with paracentral clearance and excessive edge lift inferior. Best-corrected VA (BCVA) in GPs are 20/20 OD and 20/30 OS. Scheimpflug tomography (Pentacam, Oculus) showed asymmetric irregular astigmatism, with the left eye having steeper Ks along with thinner pachymetry values than the right eye.
 |
|
Corneal tomography of the patient’s right eye (left) and left eye (right). Click image to enlarge. |
Considerations
Here, we highlight our thought process and consider how we would proceed:
Dr. Pfeifer: When deciding what lens modality to fit for any patient, but especially for those with asymmetric corneas, I like to rely on the front elevation. This patient has relatively similar front elevation differences in each eye, but the pattern of peaks and valleys is much more irregular OS than OD; this irregularity can make the movement and centration of a corneal GP less predictable, which can lead to comfort issues. Because of this, I’m inclined to switch the left eye into something that can avoid this irregularity, like a scleral lens. But what about the right eye?
There are three options for how to manage this patient going forward: leave the patient in a corneal GP OD while changing to a scleral lens OS, switch both right and left lenses to sclerals or try something completely different. For simplicity, I would discuss the first two options with the patient initially to gauge their opinion.
Two different lens modalities means two different cleaning, application and removal methods, so switching one eye only may cause undue stress. However, this patient may look at his history of success with the corneal GP OD and not want to go through the hassle of pursuing a new correction method. He may also notice the difference once he begins wearing the scleral lens in the left eye and starts to notice issues with the GP. This is why it is integral to get to know the patient and discuss their goals and/or concerns with lens wear. Trialing the lenses in-office and ensuring the patient’s awareness of wear and care of the different lenses will lead to greater chances of success in the chosen modality(ies).
Dr. Su: For this patient, the primary objective is to achieve optimal vision and comfort with his lenses. The left eye has had some discomfort with an RGP, and likely the scarring is due to a poor fit, suggesting the potential need for a refit. The front elevation maps indicate greater irregularities in the left eye which may account for this discomfort. A scleral lens, which vaults the cornea entirely, can provide clear optics and comfort.
However, potential challenges can occur if lenses of different modalities are worn in each eye, leading to lens awareness. If the patient is apprehensive, consider fitting the right eye with a scleral lens too. For the devoted long-term RGP wearer reluctant to transition, you can try redesigning the GP. Furthermore, technology has greatly evolved over the years! For eyes with more complex geometries, freeform GP lenses can be designed to better match the eye’s contours, compared with more traditional RGPs. This would ensure better lens stability while providing effective movement and efficient tear exchange.
 |
|
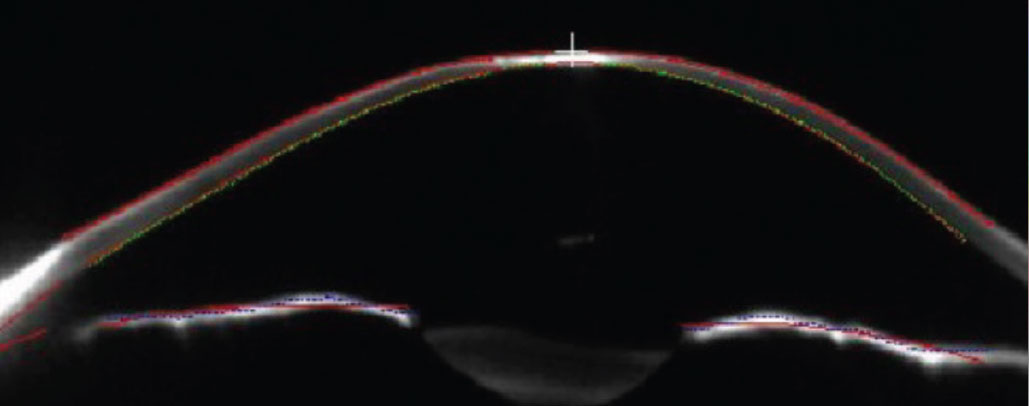
Schiempflug cross-sectional image of the left cornea. Note the central corneal scar. Click image to enlarge. |
Dr. Noyes: For me, this case has a lot of options: GPs, sclerals, hybrids, oh my! I think the biggest takeaway from this is “when is it time to switch from a GP to a scleral?” This patient was initially prescribed bilateral GP lenses but switched to a scleral in the left. In this case, the patient successfully adapted to his GP lens OD, but noted a feeling of instability OS. Especially in complex fits or patients with irregular astigmatism (such as with corneal ectasia), stability is a must; these patients require contact lenses to reach their BCVA. If the lens doesn’t stay on the eye properly, it can have devastating visual consequences on the patient’s day-to-day function. Scleral lenses do offer an advantage over RGPs in terms of corneal stability in these cases, and I think Dr. Pfeifer navigated that in an excellent fashion.
Dr. Gelles: This is the quintessential ectasia case: asymmetric in severity, very correctable with a manifest on the less severe eye. Foremost is the issue of corneal stability; this patient was well managed, having undergone CXL in the right eye, but as the ectasia is too far gone for CXL on the left eye, there is nothing else to be done. A recent publication reviewed long-term stability of corneas treated with CXL as part of an FDA clinical trial. The researchers found over the long-term, eyes with keratoconus seem to be more stable than those with post-refractive corneal ectasia.1 This highlights the importance of educating and continued monitoring of these patients, keeping in mind that treatment with CXL may be repeated in patients showing continued progression.
As for lenses, this patient could succeed with a variety of lens strategies—whether scleral, redesigned GP or hybrid—but the simplest option is a soft piggyback. This can be demonstrated in the office immediately with a diagnostic disposable soft lens. As the more severe eye is not so extreme in shape, this could be an ideal option and not even require a modification to the GP. If unsuccessful, the next choice would be a scleral lens or GP redesign. As noted previously, preference is generally to use the same type of lens in each eye for maintaining similar ocular comfort and lens care.
Discussion
It is important to keep the patient’s goals and comfort in mind when considering contact lenses for individuals with dramatic asymmetry in topography or corneal presentation. When discussing lens options with patients, educate them on the wear and care of different lens modalities. The burden of two separate cleaning regimens or insertion and removal methods may increase the chance of complications. Try to keep it simple, such as the use of hydrogen peroxide-based disinfection, which can be used for both soft and rigid materials. If a different lens modality is selected for each eye, inform the patient not to compare the two eyes. After all, “comparison is the thief of joy.” For some patients, matching modality in both eyes may beget greater success due to similar comfort levels between eyes and the ease of one routine.
Results
While this patient had mild success wearing an RGP lens in the left eye, he was ultimately prescribed a scleral lens. The choice was made due to the presence of apical corneal and patient complaints. After discussing the option of wearing a scleral lens in both eyes, the patient preferred to continue with GP correction in the right eye. He has been successful with the asymmetric lens modality and now has a BCVA of 20/20 OD and 20/25 OS.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.
1. Greenstein SA, Yu AS, Gelles JD, Huang S, Hersh PS. Long-term outcomes after corneal cross-linking for progressive keratoconus and corneal ectasia: a 10-year follow-up of the pivotal study. Eye Contact Lens. 2023;49(10):411-6. |


