  |
A 49-year-old female presented to the clinic with a history of keratoconus OD>OS. The patient had worn standard soft multifocal lenses in the past but discontinued them due to vision fluctuation and dryness. Her goal was spectacle freedom, and any glasses were unacceptable.
On initial presentation, uncorrected visual acuity was 20/70 OD and 20/40 OS, best-corrected to 20/20 at distance and near in each eye with a manifest refraction of +2.00 -3.75x085 OD and +1.75 -3.25x100 with a +1.00 add OS. Scheimpflug tomography (Pentacam Wave AXL, Oculus) showed an inferior-to-superior ratio of less than 5.00D in each eye and maximum keratometry readings of 48.00D and 46.90D in the right and left eyes, respectively. On slit lamp evaluation, there was no significant corneal haze, scars or thinning in either eye. The conjunctiva was white and quiet without any considerable surface elevations.
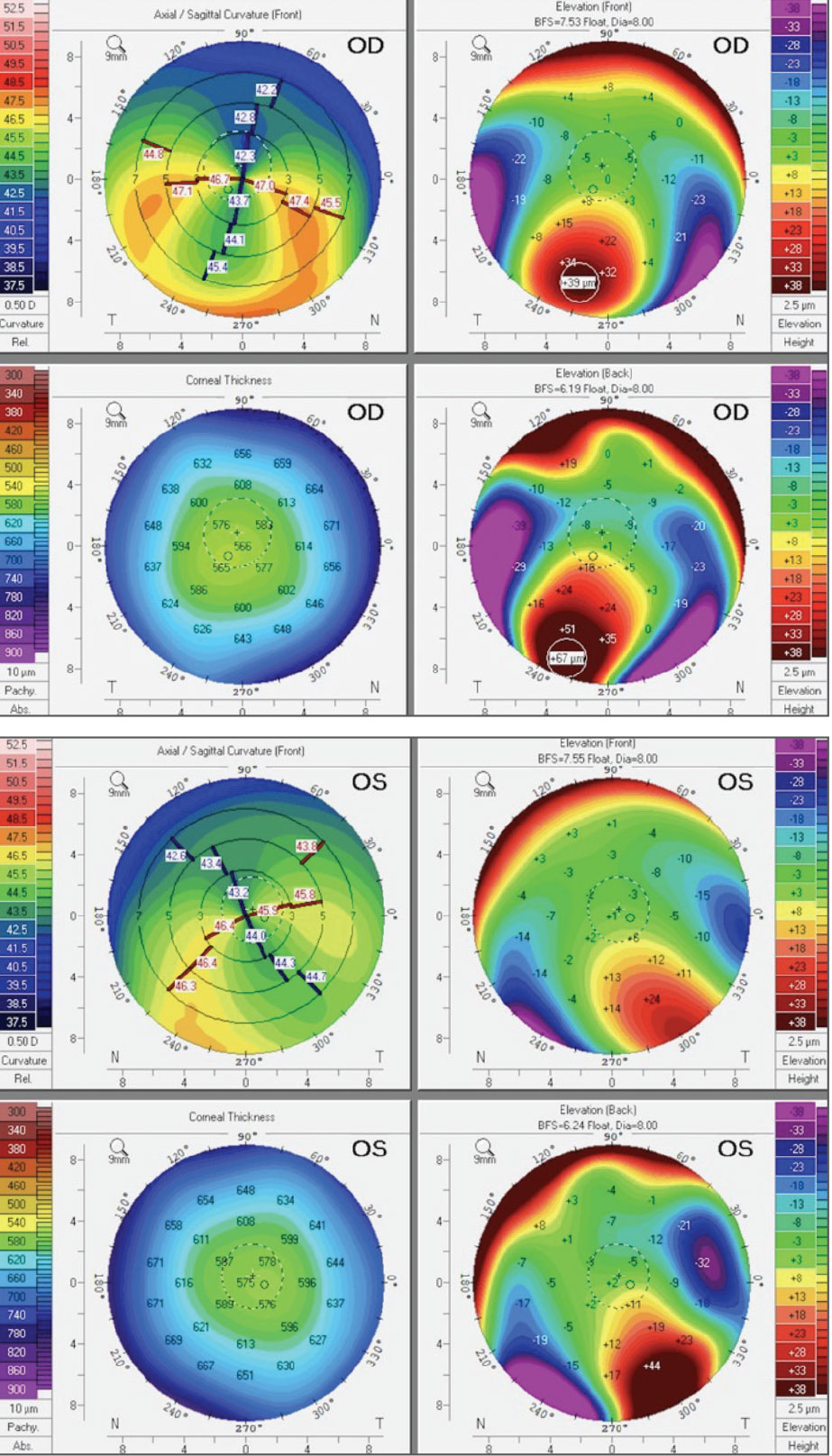 |
Corneal tomography of the patient’s right (top) and left eyes (bottom). Click image to enlarge. |
Considerations
Here, we highlight our thought processes and consider how each of us would proceed:
Dr. Su: In this case, the patient has a pellucid-like pattern, with a minimal inferior-to-superior ratio, correctable to 20/20 with manifest refraction. These patients are generally very successful with soft contact lenses. Unlike standardized soft lenses, custom soft lenses can be a great option as they are not limited to the constraints of the average cornea. Fit parameter customization and lens thickness manipulation that mask corneal irregularities can provide better comfort, lens stability and visual acuity. Furthermore, some custom soft contact lenses can add customized multifocal optics, which have the advantage of customized near-zone diameters for small-pupil patients or in circumstances where standard designs and optics underperform.
Since this patient has failed standard soft multifocal lenses before, it is likely the fitting relationship between the eye and lens was not ideal, and the lens optics did not align well with the patient’s line of sight. Custom soft lenses with a multifocal design would be a great start since she has a low add power that may allow for easier adaptation. Another option would be continuing with a custom soft option that allows for optimal centration and comfort given her corneal shape irregularity, but with monovision optics for blended vision.
Dr. Noyes: When you have a topography reading that confirms ectasia, it can be easy to slip into the “specialty lens mindset.” Most of us immediately think, “RGPs! Sclerals! Hybrids! Oh my!” but this patient can be corrected to 20/20 with a manifest refraction, meaning glasses and soft lenses are still on the table. It is completely reasonable to start a patient like this with soft lenses, custom soft lenses or even spectacles. Of course, you should monitor the ectasia and corneal changes, but you can always switch to a specialty lens later if needed.
Dr. Gelles: Keep it simple. If the manifest provides 20/20 vision and soft lenses are stable and center well without edge lift or fluting, there should be a simple, ideal option. When we see any irregularity, we often jump to something more customized and rigid; certainly, some eyes will need more complex designs, but try something simple first. Should a soft lens fail, alternatives for this patient can include corneal GP or hybrid lenses. To address the near vision demands, monovision or a multifocal should work well, especially in early presbyopia, as the disparity in monovision or induced spherical aberration in a multifocal is very small.
Also, a highlight of this case, pellucid topography patterns (kissing doves, crab claws, croissants and all the other cute names we like to give them) don’t necessarily mean pellucid marginal degeneration (PMD). The factor that matters most when differentiating PMD from keratoconus is where the thinning is located. If it is next to the limbus, you have PMD.
Another pearl is to evaluate the pupil and the topography relationship and whether the irregularity is over the pupil. In this case, the topography over the pupil is essentially regular astigmatism, which is why the patient corrects so well. Since the pupil is small, it is unlikely that the irregularity, which is so peripheral, will contribute much to the patient’s visual quality.
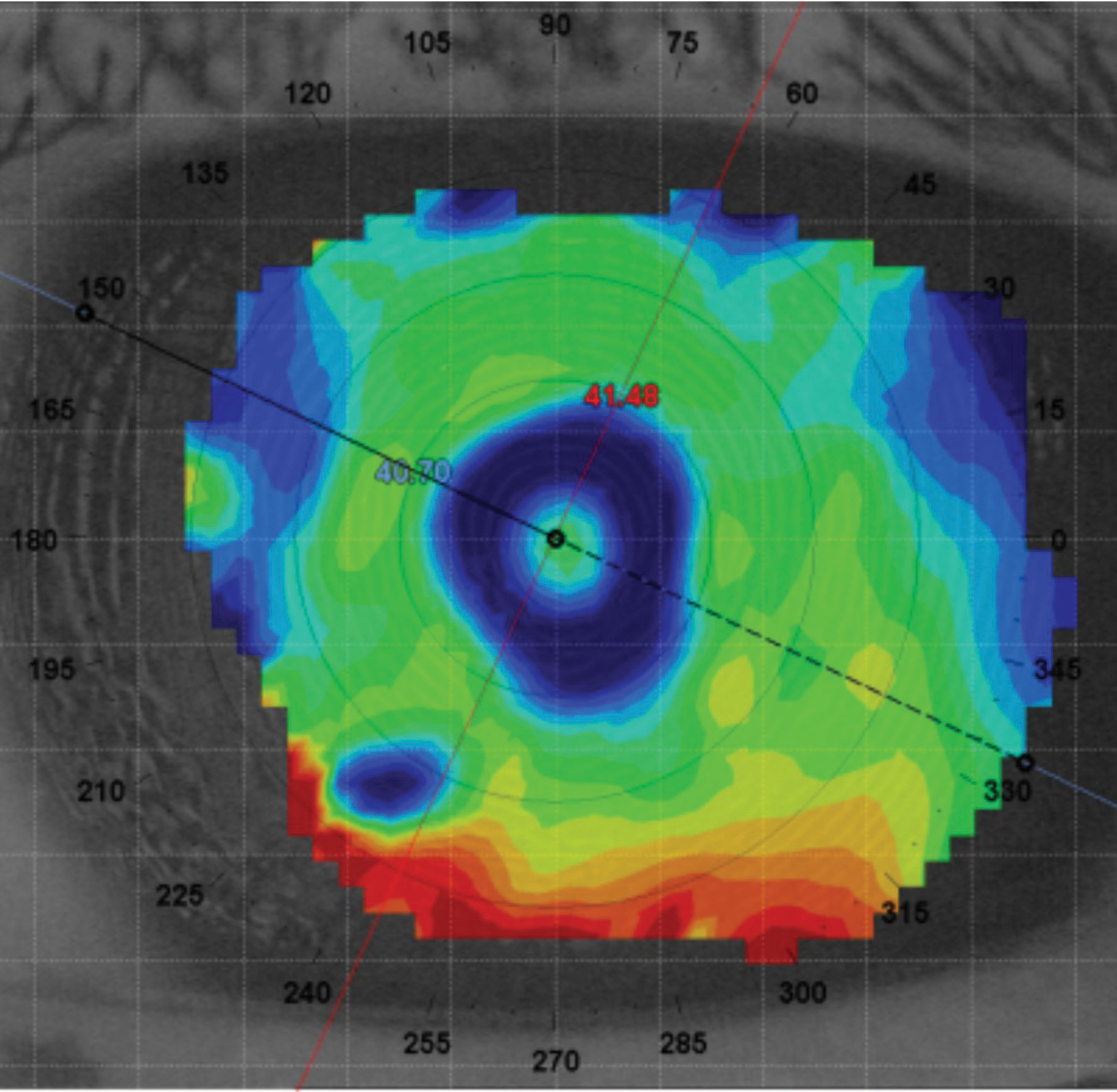 |
Over-lens topography of the left eye showing appropriate alignment with multifocal optics with the line of sight. Tangential map scaled to accentuate the multifocal. Click mage to enlarge. |
Discussion
Most standardized multifocal soft contact lenses have a standard distance and near-zone size. These lenses do not always center perfectly on the eye, which can cause inadequate distance and near vision. With the added difficulty of fitting an irregular cornea, the decentered optics can also induce even more aberrations, further reducing visual quality.
Custom multifocal soft contact lenses can be successful with customized parameters such as diameter (OAD) and base curve (BC) to improve the fitting relationship and customized optics such as distance, intermediate and near power and optic zone size parameters—even optic zone decentration—to align the lens optics with the line of sight. The extensive power profiles and customized fitting parameters allow eyecare practitioners the complete freedom to design a lens with excellent optics at all distances for hard-to-fit presbyopic patients.
Results
The patient was fit with a custom multifocal toric (Revive, Bausch + Lomb) soft lens with the following lens parameters: BC 8.5mm, OAD 14.50mm, power +1.75 -3.75x085 OD; BC 8.5mm, OAD 14.50mm, power +2.00-3.25x100 OS. The add was +1.00 in a near-centered design with a 2.20mm central near-zone diameter. Her best-corrected visual acuities were 20/20 OD, 20/20 OS and 20/15 OU, and she reported clear, comfortable vision at distance, intermediate and near.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


