 |
When properly fit, corneal gas permeable (GP) multifocal lenses can provide a clear, comfortable and healthy contact lens option. Fortunately, these lenses are generally simple to fit and follow the same basic fitting strategies as other GPs. An ideal fit consists of a centered lens, a slightly steep central and mid-peripheral fluorescein pattern, approximately 1mm of edge lift and 1mm to 2mm of movement. This case highlights the importance of a properly fit lens in achieving visual success and demonstrates the impact that poorly fit corneal GP lenses can have on the anterior corneal surface.
The Case
A 59-year-old female presented for a contact lens fitting. She had been wearing corneal GP lenses for more than 30 years. During the past five, she had moved from distance vision to multifocal lenses. During this period, she struggled to achieve the near vision she needed to be functional in her occupation as an accountant. Also, the distance vision she was able to achieve with her glasses was not clear on the days she had worn her lenses. She presented to our office for a second opinion, as she had grown frustrated with her current lenses.
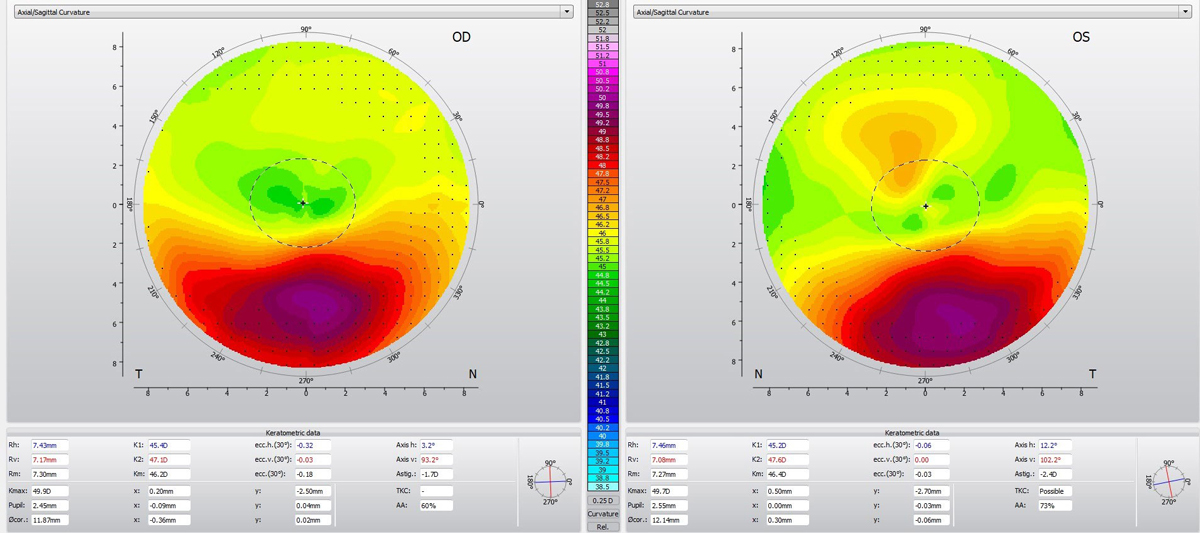 |
| Fig. 1. The patient’s eyes had a large degree of asymmetry between the superior and inferior cornea with significant inferior steepening. Click image to enlarge. |
Diagnostic Testing
Entering distance visual acuity (DVA) with her current lenses was 20/30 OD, 20/30 OS and 20/30 OU. Near visual acuity (NVA) was 20/50 OU. The fit assessment in both eyes showed a superiorly decentered lens, a flat central fitting relationship and high edge lift. The lens was essentially immobile, requiring manual manipulation to create any movement. Parameters of the patient’s habitual lenses were unavailable, though the overall diameter (OAD) was measured at 9.3mm OD and OS.
Upon removal of the patient’s lenses, I performed topography. Both eyes demonstrated a large degree of asymmetry between the superior and inferior cornea with significant inferior steepening (Figure 1).
Slit-lamp exam of the cornea was relatively unremarkable with an intact epithelium and a clear stroma. There was no evidence of ectasia.
I then conducted refraction. Her habitual glasses yielded -7.75 -0.25x033 with a DVA of 20/80 and an NVA of 20/50 OD and -8.75 with a DVA of 20/50 OS and an add of +2.25D OU. Her manifest refraction was -5.25 -0.50x140 with a DVA of 20/25 and an NVA of 20/25 OD and -7.50 -0.25x050 with a DVA of 20/25 OS and an add of +2.00D OU.
Based on the fit assessment and topography, I identified corneal molding (i.e., corneal reshaping as a result of the interaction between the cornea and contact lens). The superior decentration and flat fit of the patient’s habitual lenses had resulted in superior flattening and inferior steepening of the anterior corneal surface. This was further suggested by the patient’s complaint of spectacle blur, a potential result of flat-fitting corneal GP lenses. In comparing the manifest refraction after lens removal to the patient’s habitual glasses, there was clearly a hyperopic refractive shift created by the central corneal pressure exerted by her habitual lenses.
I reviewed this with the patient and advised a refit. Although I would have preferred she discontinue lens wear for one to two weeks before a refit, the patient noted she was unable to function in her current glasses. As such, I performed an initial fitting with the expectation that additional alterations would be required based on the expected changes in her corneal shape following the discontinuation of her current lenses. Her glasses Rx would be finalized following the contact lens refit.
Initial Fitting
I used a spherical corneal GP lens to perform a diagnostic fitting and a larger-diameter corneal lens to better center the lens. We trialed lenses until achieving a uniformly aligned fit OU.
Consistent with the patient’s corneal topography, the lenses tended to decenter inferiorly, centering over the steepest portion of the cornea. I accepted this outcome because of her current corneal shape and assumed the decentration would correct itself as the cornea returned to a more symmetrical pattern.
The diagnostic lenses that displayed the best fitting relationship were -3.00D/46.50D/10.00mm OAD/0.12mm axial edge lift (AEL) with an over-refraction of -4.00D and a DVA of 20/20 OD and -3.00D/46.50D/10.00mm OAD/0.12mm AEL with an over-refraction of -5.50D and a DVA of 20/20 OS.
While the central relationship was adequate, the lenses displayed excess edge lift. I compensated for this by decreasing the AEL to 0.08mm in both eyes. I selected a center-distance aspheric multifocal design and calculated the add by using lens design guidelines and adding 0.25D to the spectacle add.
I ordered the following lenses: -6.75D/+2.25D add/ 46.50D/ 10.00mm OAD/0.08mm AEL OD and -8.25D/+2.25D add/46.50D/ 10.00mm OAD/0.08mm AEL OS.
Lens Dispensing
At this visit, the lenses showed a fairly uniform alignment pattern, were minimally decentered inferiorly and an improved edge lift compared with the diagnostic lenses. The patient’s distance and near vision was 20/30 OU. I dispensed the lenses and asked the patient to return in one week.
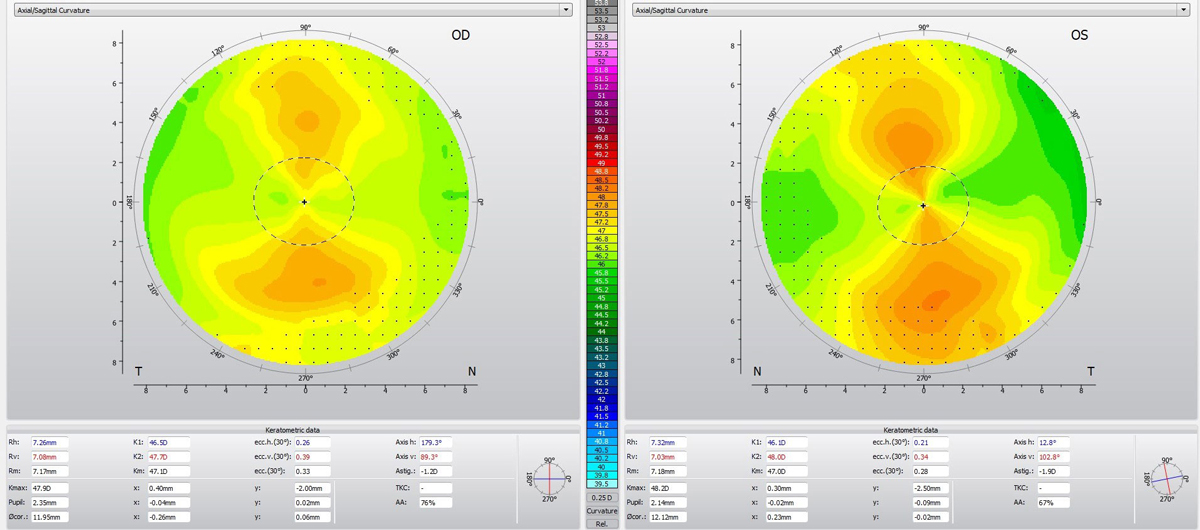 |
| Fig. 2. A regular, with-the-rule corneal astigmatism pattern was visible in both eyes. Click image to enlarge. |
Follow-up
The entering distance vision was 20/30 OU and near vision was 20/20 OU. She reported improved vision compared with her habitual lenses at near but said her distance vision was not as clear as she would like. She noted good comfort with the lenses and no difficulty removing them.
The lens fit had significantly changed since dispensing. The lens centration had gone from inferior OU to well-centered OD and mildly superiorly decentered OS. The fluorescein pattern now displayed a with-the-rule astigmatism pattern with alignment along the horizontal meridian and mild clearance along the vertical meridian.
The right eye had adequate edge lift 360° around the lens, while the left eye showed excess superior and inferior edge lift. I presumed this high vertical edge lift was causing the mild superior decentration in the left eye. The fit was optimal in the right eye. I used a toric edge design in the left eye to steepen the vertical meridian’s edge and improve centration.
A -0.50 OU distance over-refraction improved distance acuity to 20/20 while preserving near acuity of 20/20. I ordered new lenses with these parameters: -7.25D/+2.25D add/46.50D/10.00mm OAD/0.08mm AEL OD and -8.75D/+2.25D add/46.50D/10.00mm OAD/0.08mm AEL OS. These lenses yielded a distance and near visual acuity of 20/20 OU. As expected, the new left lens was centered and displayed a more uniform edge lift pattern with the toric peripheral curves.
The patient returned two weeks later and reported excellent distance and near vision. Her distance and near visual acuity was still 20/20 OU. The fit remained unchanged with centered lenses, a with-the-rule central fitting relationship, uniform edge lift and 1mm of movement. After removing the lenses, I performed topography. Both eyes displayed a regular, with-the-rule corneal astigmatism pattern (Figure 2). I finalized the contact lens Rx.
I then repeated manifest refraction. As anticipated, the results were significantly different with the refit. The new manifest correlated well with the changes in topography. It measured -8.25 -1.25x180 with a DVA of 20/20 and an NVA of 20/20 OD and -9.00 -2.25x015 with a DVA of 20/20 OS and an add of +2.00D OU.
I issued a new glasses prescription. The patient has since reported an easier transition from contact lenses to glasses upon lens removal.
Discussion
I needed to correct two issues when refitting this patient. First and foremost, I was tasked with improving distance and near vision in contact lenses. Secondarily, I had to address her spectacle blur. Both issues were the result of poor-fitting habitual lenses. The flat-fitting original lenses were decentered superiorly, placing the patient’s visual axis within the mid-periphery of the lens and resulting in subpar visual performance at both distance and near. The fit was also causing the corneal molding responsible for the spectacle blur.
To improve centration, we pursued a larger lens design and a central alignment fit. The patient was able to achieve clear distance and near vision while easily transitioning from contact lenses to glasses.


