  |
A 33-year-old male presented to the clinic with a history of keratoconus, forme-fruste in the right eye and moderate in the left, made even more challenging by his career as a pilot. The left eye was treated with corneal crosslinking about one year ago. The patient had a history of soft lens intolerance in the left eye, which was currently corrected with a scleral lens. He reported discomfort and rebound redness with his habitual scleral lens. Notably, he reported that despite scleral lens wear, visual quality of the left eye was poor compared with the right. His goal was to have similar visual quality in both eyes.
On initial presentation, uncorrected visual acuity was 20/20 OD and 20/40 OS. Visual acuity with his habitual scleral lens on the left eye was 20/20. Best-corrected visual acuity (BCVA) was 20/20 in each eye, with a manifest refraction of +0.25-0.50x090 OD and +0.25-4.25x120 OS.
Scheimpflug tomography (Pentacam Wave AXL, Oculus) showed maximum keratometry readings of 41.9D and 48.2D and IS ratios of 1.5D and 10.5D in the right and left eyes, respectively. On the slit lamp exam, large nasal pingueculas were documented on each eye. With the current scleral lens, there was significant impingement on the pinguecula during lens wear, and upon removal, there was a deep lens impression and grade three injection of the conjunctiva at the pinguecula.
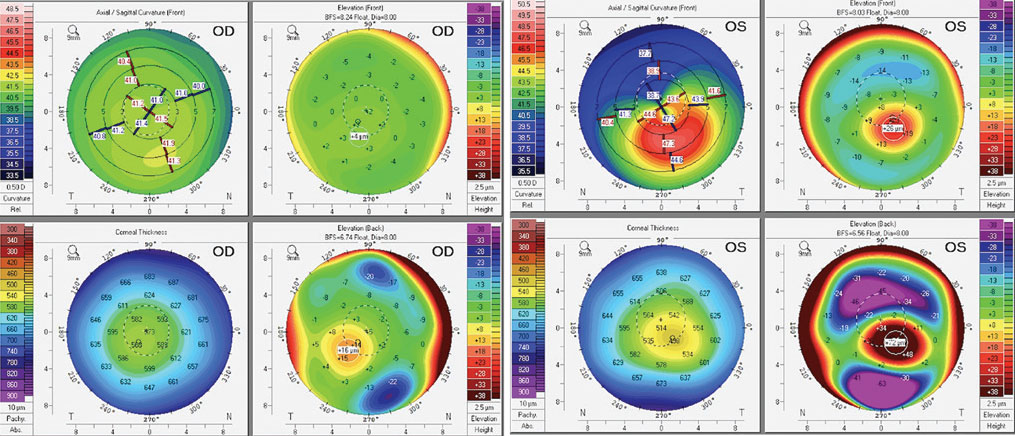 |
| Corneal tomography of the patient’s right and left eyes. Click image to enlarge. |
Considerations
Here, we highlight our thought processes and consider how each of us would proceed in this situation:
Dr. Su. Aviation has strict visual requirements since pilots must navigate difficult and dynamic conditions. Crisp vision is a must. Although this patient can achieve 20/20 vision with glasses, it is not surprising that the amount of irregular astigmatism from the left eye would result in glare, halos and ghosting images. These visual disturbances could have dangerous consequences, especially while flying.
A modality such as a rigid gas permeable (RGP), hybrid or scleral lens could provide the optics needed for crisp vision. However, consideration needs to be taken for the patient’s lifestyle and occupation. Since he is sometimes required to fly for long periods in a dry environment, an RGP or hybrid lens may not give him comfort or visual stability compared with a scleral lens. In this case, a scleral may be the right choice to help him achieve his goals.
Additionally, the patient reported residual glare and streaking of images from his habitual scleral lens, most likely due to the residual higher-order aberrations (HOAs). With wavefront-guided scleral lens technology, we can further reduce the residual glare/flare/halos with HOA-correcting optics incorporated on the front surface of the scleral lens. These high-performance optics would reduce the amount of shadowing, resulting in a similar visual experience in both eyes.
A common challenge to successful scleral lens wear is the presence of a pinguecula. The lens haptic can cause compression and mechanical damage to the tissue, resulting in redness and discomfort. For some patients, reducing the lens diameter to minimize the interaction of the lens edge with the lesion is the simplest option. Nonetheless, this may be more difficult in patients with moderately large pingueculas or those close to the limbus. More complex options include edge notching—removal of lens edge material—to avoid the pinguecula. Careful follow-up is still needed to ensure the conjunctival tissue around the notch does not impinge and desiccate over time. Some scleral lens designs can incorporate a micro elevation to contour the edge over the pinguecula without compression. Custom impression-based or scan-based scleral lenses may provide the best fit and comfort for this patient, as ocular surface data takes into account all the elevations and contours of the cornea and sclera. This can be mirrored and manufactured onto the lens haptic.
Dr. Gelles. Patients with asymmetric keratoconus can be some of the most challenging, especially when the less affected eye is nearly emmetropic. Adequate uncorrected vision of the emmetropic eye can make monocular contact lens wear a chore. These patients are often hyper-aware of the lens. For monocular wear, I tend to use soft and scleral lenses over other options as they are usually associated with less lens awareness.
Another challenge is visual quality. Even with correction, the more severe eye may still not be on par with the better eye due to residual aberrations. To address visual quality complaints, wavefront-guided optics can provide a solution. These are currently available but only on select scleral lens designs. Research shows a 40% to 60% reduction in HOAs, and our clinical experience mirrors these numbers. Add a large pinguecula and you have a real challenge.
In this case, there is also a mental aspect to consider. The patient is already wearing a scleral lens, which is not meeting his needs. A previously poor experience can make trying the same contact lens modality again challenging. An impression-based scleral lens with wavefront-guided optics may be the best choice in this situation. It’s important to explain the lens differences so there is an understanding that though we will be using another scleral lens, it will be nothing like the current.
Dr. Noyes. Any case where the patient’s subjective vision does not line up with their visual acuity is difficult, especially when they are reading close to 20/20 or better. In this specific situation I’d tell the patient, “You don’t have to wear your scleral lens all the time, but you do have to wear it while you’re flying.” Many of these patients will find it cumbersome to wear a lens when they can complete their daily tasks without them. It’s important to keep the patient’s lifestyle in mind when fitting them in scleral contact lenses. If for some reason vision is not satisfactory with scleral lenses, new advancements such as HOA correction provided by wavefront-guided optics are now an option.
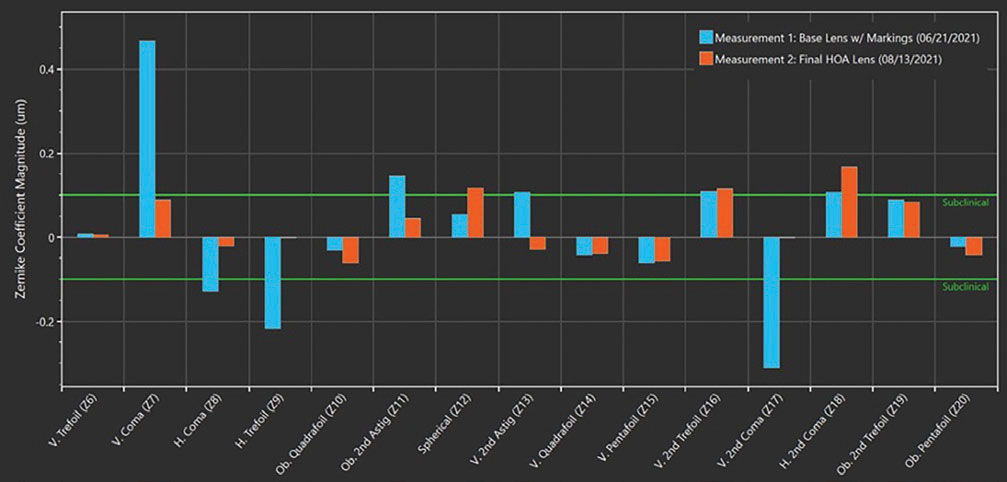 |
| Aberrations of the standard scleral lens (base lens) vs. the wavefront-guided scleral lens (final lens) in the left eye. Click image to enlarge. |
Discussion
Complex ocular geometries and conjunctival elevations, such as pingueculas, can cause trouble with scleral lens wear. Modifying the lens haptic with advanced options to contour over these obstacles will ensure comfortable and healthy lens wear over time. To evaluate the visual potential and quality of the worse eye, a rigid lens over-refraction must be done. If vision improves and residual glare is resolved with an over-refraction, the over-refraction can be incorporated onto the front surface of the scleral lens, and the optics can be finalized. If the glare is not fixed, the problem primarily lies in residual HOAs. Wavefront aberrometry over the scleral lens will quantify the type and amount of residual aberration.
An integrated wavefront aberrometry system now exists, which can measure the amount of residual HOAs and turn them into a wavefront-guided optical profile on the lens. Once manufactured and worn, this will reduce residual aberrations and lead to improved quality of vision. Incorporating new technological advancements such as this and working with the necessary labs can help your patient achieve their desirable clear and comfortable vision in both eyes.
Result
The patient was refit with an ocular impression-based scleral lens (EyePrintPro, EyePrint Prosthetics) on the left eye. Importantly, he was directed to discontinue lens wear for one to two weeks to allow the conjunctival tissue to return to its natural shape. On follow-up, he presented with 20/15 OD and 20/30 OS visual acuity, with a BCVA of 20/20 in the left eye with a spherical-cylindrical over-refraction. HOA-correcting optics were ordered via a wavefront aberrometry system (xWave, Ovitz).
On further follow-up, he presented with 20/15 visual acuity in the right and left eyes. The residual HOA was reduced by 53% after incorporating the HOA-correcting optics onto the front surface of the lens. The patient was delighted to have equal vision in both eyes and significantly improved quality of vision in the left eye during his flights.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


