 |
Scleral lenses are a popular tool to manage the symptoms of patients with severe dry eye. This modality, however, only masks a patient’s symptoms, so the root cause of dry eye must still be treated. In turn, optimizing the surface of the eye improves the likelihood of success with scleral lens wear. It’s a win-win scenario.
The Case
A 78-year-old female with severe light sensitivity and blurred vision from ocular rosacea was referred for a scleral lens fitting. She wore glasses and was very hesitant to try contact lenses. Scleral lenses were a last-ditch effort to improve her severe symptoms.
The patient had been treated for ocular surface disease for many years. She had cataract surgery OU in 2015. Her ocular history was also positive for glaucoma, for which she was taking Combigan (brimonidine/timolol, Allergan) BID and latanoprost QD.
Her dry eye regimen for both eyes included lid cleansing with tea tree oil wash and hypochlorous acid spray twice daily, Retaine MGD preservative-free eye drops (Ocusoft) four to six times a day, warm compresses with a heat mask and omega-3 supplementation daily and Restasis (cyclosporine, Allergan) twice a day. She had just discontinued her course of doxycycline 50mg BID after six weeks because the drug upset her stomach and didn’t improve her symptoms. She found symptom relief with Lotemax gel (loteprednol etabonate, Bausch + Lomb) but has not been using it because she responds to steroids and has glaucoma. She underwent LipiFlow (Johnson & Johnson Vision) a year ago, which provided minimal relief for a short period of time.
Visual acuities (VAs) were 20/40 OD and 20/30- OS, pinholed to 20/20 OU. Her pupils were round and reactive to light, with no relative afferent pupillary defects. Extraocular movements were full OU.
The slit lamp exam revealed a thickened lid margin with telangiectasia OU, significant biofilm and debris on the lid margin along with cylindrical collarettes and 2+ diffuse punctate epithelial erosions OU as well as a deep and quiet anterior chamber OU (Figure 1). Posterior chamber intraocular lenses were noted in both eyes. Light pressure on the meibomian glands produced very little turbid expression. Non-contact tear break-up time was instant OD and three seconds OS. The patient’s intraocular pressure was 11mm Hg OU. Her keratometry readings were 45.00/46.00@045 OD and 44.00/44.50@150 OS. Undilated posterior segment evaluation revealed thin neuroretinal rims of 0.7mm OD and 0.5mm OS with a clear macula.
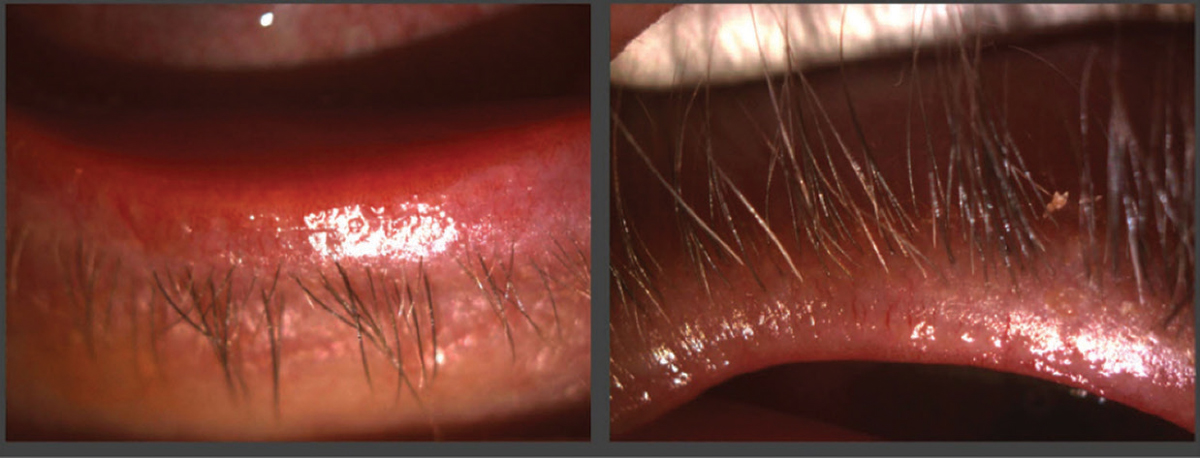 |
| Fig. 1. The patient had significant telangiectasia and blepharitis. Click image to enlarge. |
Diagnostic Fitting
The patient found immediate relief from the burning sensation in her eyes with scleral lens wear. She was fit with SynergEyes VS scleral lenses OU with a base curve (BC)/vault of 8.4/3500 OU, a diameter of 16.0mm OU, powers of +1.75 OD and +3.25 OS and a haptic of 34/40 OU. Her VA was 20/20 OU with the diagnostic lens over-refraction. Hydra-PEG was added to the lenses to improve the lubricity of the front surface.
She was instructed to continue her regimen of tea tree oil wash, hypochlorous acid spray, warm compresses, omega-3 vitamins and Restasis. BlephEx treatment was performed in-office with tea tree oil on both eyes to address Demodex. The patient was referred for intense pulsed laser (IPL) treatment to manage surface inflammation and for dietary advice to formulate a low inflammatory plan while avoiding foods that could trigger her symptoms. She did not respond well to IPL, as the procedure was painful for her, her skin was sensitive for 24 hours and she started to bruise.
Dispensing
The patient returned two weeks later. The fit was optimal, at 200µm of central clearance with limbal-to-limbal clearance. The haptic aligned with the conjunctiva with no blanching. Her VAs were 20/20 OD and 20/20 OS. She was trained to insert and remove her lenses and use Clear Care (hydrogen peroxide, Alcon) at night to minimize the preservatives to the ocular surface and non-preserved saline to fill.
Follow-up
The patient returned one week later. Her light sensitivity had improved, and the contact lenses provided immense relief. They became cloudy after a few hours of wear, however, so she had to rinse them in the middle of the day to clear the debris. Other than that, she was able to wear her lenses for 14 to 16 hours per day with no issues.
Her VAs were 20/30+ OD and 20/25- OS. On slit lamp examination, both her lens chambers were filled with mucus and tear film debris. Fluorescein showed quick uptake at 12 o’clock and slightly inferior conjunctival chalasis under the lens, indicating excessive limbal clearance in both lenses. No over-refraction was noted after the lenses were rinsed and reinserted. Another set was ordered with a slightly tighter vertical meridian in both eyes.
The haptic lines indicating flat edge were at 3/9 o’clock in each eye. The 12/6 o’clock meridian was steepend. The BC of the lenses was also steepened to lower limbal clearance, and the power was adjusted as a result. She was refit with SynergEyes VS scleral lenses OU with a BC/vault of 8.0/3500 OU, a diameter of 16.0mm OU, powers of -0.25 OD and +1.25 OS and a haptic of 34/42 OU.
Dispensing Redo
The patient returned five weeks later. She had an IPL session one week prior and responded much better to it, with less pain and residual side effects. Her tear film debris had improved, and her face was visibly less red. The lenses showed optimal haptic alignment and no superior seeping with fluorescein. The limbal clearance was 50μm to 75μm. Her VAs were unchanged at 20/20 OD and 20/20 OS.
Second Follow-up
The patient didn’t return for another two months. This time, she had undergone four sessions of IPL and one session of LipiFlow in both eyes and had noticed a big difference in her overall ocular comfort even without contact lenses. Her lid margin was clearer and whiter (Figure 2). She preferred wearing the lenses but was able to go some weekends without them, which was not always the case. Her lenses were finalized.
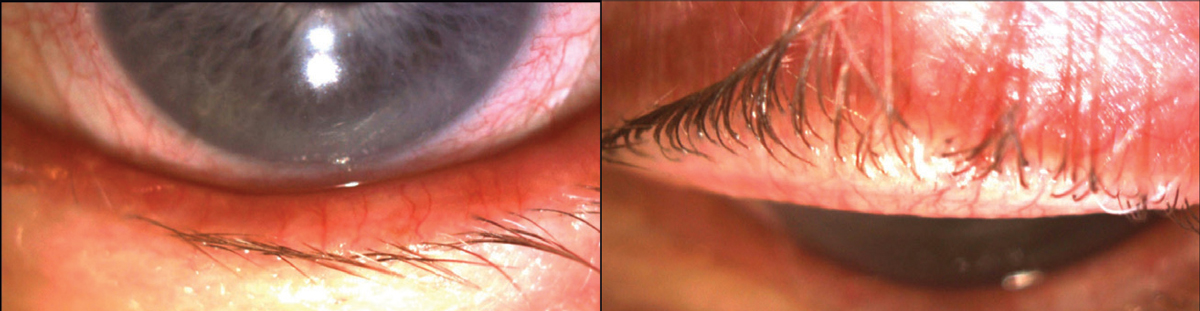 |
| Fig. 2. The patient eventually found success with IPL therapy. Click image to enlarge. |
Discussion
Rosacea is a chronic inflammatory skin condition that primarily affects the face and periocular regions, with 58% to 72% of rosacea patients developing ophthalmic findings.1 These patients typically have inflammatory dry eye with meibomian gland dysfunction (MGD) and Demodex-related blepharitis. MGD presents as abnormal turbid meibomian gland secretion, which causes blocking and/or atrophy of the glands and recurrent hordeolum. Typical slit-lamp examination of the eyelid margins shows telangiectasia and thickening of the lid margin in 50% to 94% of patients.1
The standard of care for these patients includes minimizing inflammation through medication use and treating the lid margin. Sometimes, this isn’t enough. Left untreated, severe cases can lead to peripheral corneal ulceration, corneal scarring and neovascularization.2
Conservative treatment of mild ocular rosacea includes lid cleansing, warm compresses and artificial tears. Patients with ocular rosacea have enhanced sensitivity to common environmental stimuli, such as ultraviolet light, certain foods, extreme weather, stress, exercise, alcohol, caffeine and cosmetics and should avoid these triggers.1 If symptoms are more severe, Restasis and/or oral doxycycline are recommended. LipiFlow has also been shown to improve meibomian gland inspissation. However, in my experience, reducing inflammation before gland expression has been more effective. IPL can limit lid inflammation by targeting blood vessels along the eyelid, inhibiting inflammatory mediators from accessing the meibomian glands. IPL also creates a mild local warming effect to allow better inspissated meibum expression and eliminate bacteria that cause meibomitis.3
Treat the root cause of a patient’s dry eye and reduce inflammation rather than mask their symptoms with a scleral lens. These patients will, in turn, have a higher chance of success with contact lens tolerance.
1. Oge’ LK, Muncie HL, Phillips-Savoy AR. Rosacea: diagnosis and treatment. Am Fam Physician. 2015;92(3):187-96. 2. Layton AM. Pharmacologic treatments for rosacea. Clin Dermatol. 2017;35(2):207-12. 3. Gupta PK, Vora GK, Matossian C, et al. Outcomes of intense pulsed light therapy for treatment of evaporative dry eye disease. Can J Ophthalmol. 2016;51(4):249-53. |


