Scleral lenses (SLs) are lifesavers! However, some SL wearers, even those with 20/20 vision, report quality of vision still falling short. The most common complaints are bothersome ghosting, smearing, halo and glare. On examination, there are no media opacities, such as cataracts, that could explain the reduction in vision quality. Despite the practitioner’s best efforts, the vision quality can’t be further improved with a traditional SL (tSL). So what’s the reason for the poor visual quality, and is there anything that can be done to improve it further? These patients may be struggling with residual higher order aberrations (HOAs); you can help improve their vision and quality of life, even those with 20/20 vision, by using wavefront-guided scleral lenses (wfgSLs).1
Background
Rigid contact lenses have long been the mainstay to improve vision caused by irregular corneal astigmatism. As we all know, this type of astigmatism induces HOAs. A rigid contact lens can mask the anterior surface of the irregular corneal astigmatism to reduce HOAs and improve vision. In many conditions, like keratoconus, the posterior cornea is often irregular as well. When the anterior cornea is masked by the rigid lens, the internal aberrations from the posterior cornea can come through; these are residual HOAs.2 Other factors can be the source of residual HOAs as well, such as the rigid lens itself, fluctuations in pupil diameter, tear film, accommodative status, crystalline lens shape and age.
Wavefront aberrometry can help in cases such as these, as it is an objective method of measuring aberrations of the eye. It works by projecting infrared light into the eye, then measuring the reflected light’s deviation from a plane of focus. Wavefront aberrometry is highly sensitive but not specific. Additional combination instruments, such as an aberrometer combined with a topographer, are needed to determine the structure of the eye that is abnormal. Because of its function, wavefront aberrometry is useful for understanding patients’ visual complaints. One advantage that wavefront aberrometry presents is the possibility for data to be presented in various forms, including wavefront maps, tables and bar graphs.
One of the most beneficial data displays is the point spread function (PSF), simulating how a patient would see a perfect white point on a black background. Aberrations are measured in microns and defined by a pupil diameter. The three primary HOAs associated with reduced vision quality are coma, trefoil and spherical aberrations. When combined, they blend together, leading to a patient’s complex visual complaints. When a contact lens is worn, the lens becomes part of the optical system of the eye that is being measured and residual aberrations are what is left over once a lens is fit.
 |
|
Fig. 1. Comparison of a PSF from two different patients: one with a normal cornea (left) and the other with keratoconus (right). Using these PSF simulations can be a great way to communicate to patients and show them that you understand the visual issues they are experiencing. This can be very validating and aid in building trust and rapport with patients. Click image to enlarge. |
WfgSLs can reduce these residual aberrations. The process of creating a wfgSL starts with a typical SL design process. After an ideal SL fit is achieved, a duplicate SL with fiducials (a dot matrix on the front of the lens) is worn by the patient. From there, wavefront aberrometry is used to capture the residual HOA data, the position of the lens and the location of the line of sight. Using this data, a wavefront-guided optical profile is created. WfgSLs work by the principle of destructive interference, similar to noise-canceling headphones, to reduce HOAs. The patient’s vision is evaluated by capturing an aberrometry measurement at the follow-up.
Now, let’s get to some practical pearls learned over the course of a few years and spanning several hundred eyes at the Cornea and Laser Eye Institute. Many of these tips have been presented as manuscripts, posters or abstracts from our clinic, but others are simply from clinical experience. All of these should help you deepen your understanding of the nuances of aberrometry, HOAs and wfgSLs.
1. Don’t Forget: Words Matter
Setting expectations is vital to success. It is important to educate the patient that this wfgSL will not entirely eliminate HOAs. They can expect an improvement in visual quality, but not perfect vision. Generally, irregular corneal astigmatism patients at our facility experience an average 50% HOA reduction and one line or more improvement in visual acuity using the Ovitz system.3 This is similar to the published data.4-6 It is paramount to iterate to patients, especially those who are already 20/20, that they may or may not gain lines of acuity but should experience an improvement in visual quality. That said, we have seen up to five lines of visual acuity gain in our clinic. We have also seen normal cornea patients go from a best-corrected visual acuity of 20/20 to 20/10.
2. There is a Method to the Madness
Maximizing pupil size is crucial when capturing aberrometry. There are two methods to do so: either pharmacologically dilated or physiologically dilated, each with their pros and cons. Only the pharmacologic method, though, has been primarily reported on in the literature.4-6 The optic zone of the wavefront-guided optics is only as large as the maximum pupil diameter that was achieved during the aberrometry. When the wavefront-guided optic zone isn’t large enough, the adjustment from the wavefront-guided optics patch to the standard optical carrier will encroach into the pupil and be an additional source of aberration.
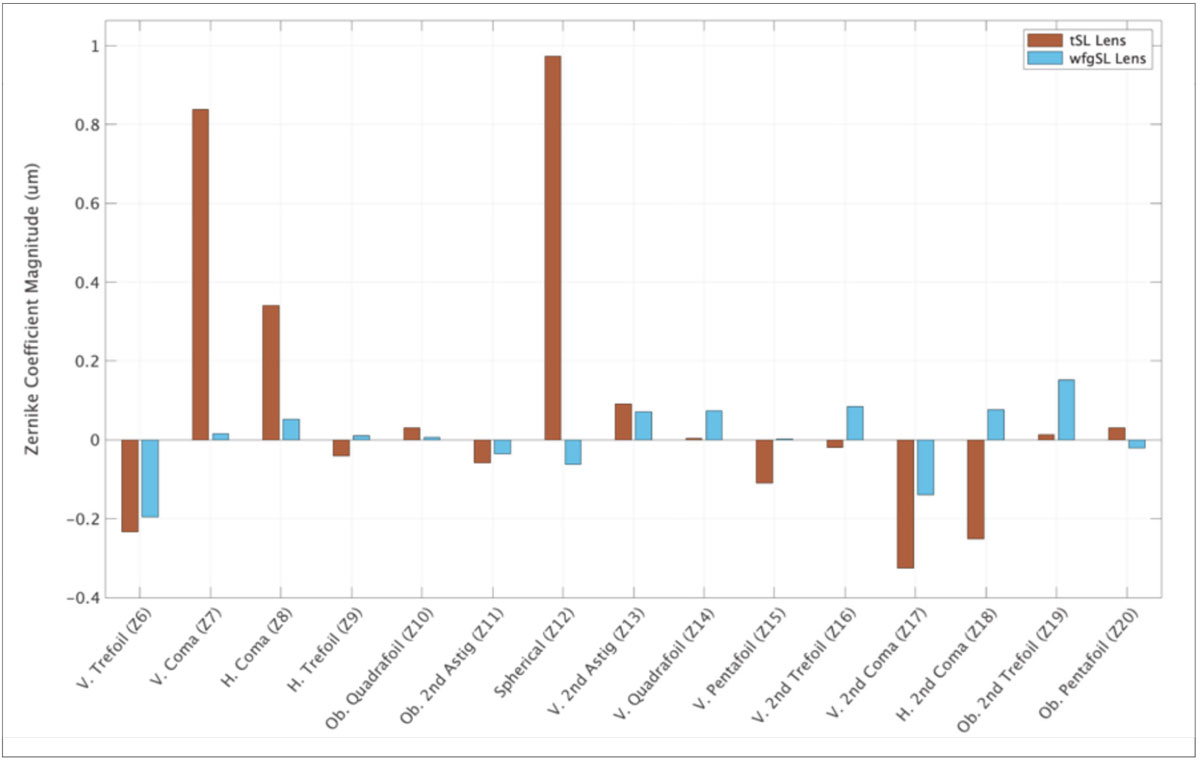 |
|
Fig. 2. Bar plot comparing magnitude of individual Zernike coefficients in a keratoconus patient wearing a tSL vs. a wfgSL. All major aberration showed significant reduction with the wfgSL. Higher order root mean square (HORMS) decreased from 1.43µm to 0.41µm. All data is reported at a 7.8mm pupil diameter. Click image to enlarge. |
If your wavefront aberrometer is located in a testing room that has ambient room illumination, pharmacologic dilation is necessary to ensure you capture HOA data through a maximum pupil diameter, as patients will likely encounter darker environments. However, if your aberrometer is located in a room without windows and lighting can be shut off completely, the patient can naturally dilate. In this situation, it is unlikely the patient will experience a darker environment. Which is better? We don’t currently know, but our results with the undilated method mirror the published pharmacologically dilated results.
3. Relationships are Paramount
The success of wfgSLs is predicated on the lenses staying in the same position—this makes the fitting relationship paramount. A tSL can have a little bit of movement and still be successful, but for wfgSLs, slight change in position can cause reduced vision.7 To stabilize the lens, using a non-spherical haptic, whether it be toric, quadrant-specific or free-form haptics is necessary.8,9 Our experience has shown all these haptic options can work well to stabilize the lens.
4. A Material World
There are questions that arise about the effect of lens coatings, such as Tangible Hydra-PEG. The effect of lens cleaning also comes with these concerns. Luckily, the literature has a publication for each, and the good news is there seems to be no ill effect from coatings or cleaning, at least when simulated over the course of one year.10,11
5. Allow Adequate Time for the Process
Good things take time and expense, and wfgSLs are no exception. Patients must understand that the process is longer than prescribing a tSL and is considered a premium option. As such, they will have an increased cost associated with them. In our office, we find the process adds approximately two to three additional lenses (one being the alignment lens) and associated visits to finalize.
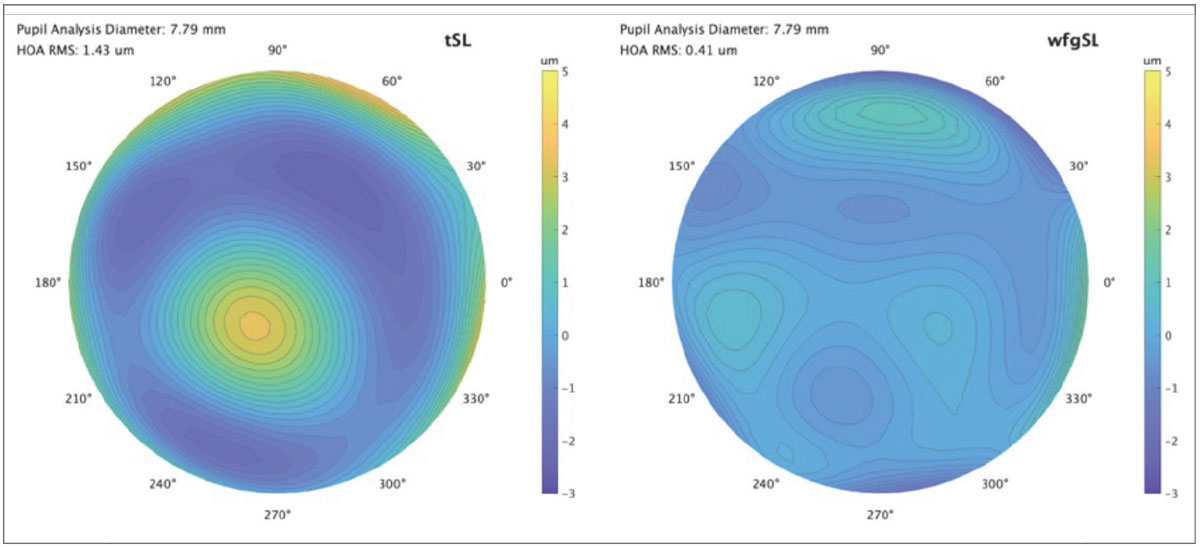 |
|
Fig. 3. Comparison of wavefront maps of the patient from Fig. 2. wearing the tSL vs. wfgSL. Click image to enlarge. |
6. Get Used to It
Neural adaptation is an important aspect of wearing wfgSLs. If you dispense the wfgSL in your office, be sure to educate the patient that there will likely be an adaptation period; this may occur over the course of several weeks. Our clinic saw a minority percentage of patients gain an additional line after a four-week period of wfgSL wear.12
7. Please Mind the Overrefraction
For patients that take large astigmatic overrefractions, if these do not improve the vision as much as expected, do not incorporate them. Instead, create a wfgSL first, then overrefract. In my clinic, I have not yet seen a patient that actually needs a high astigmatic overrefraction after having their HOA reduced with a wfgSL.
8. A Double-Edged Sword
Residual HOAs are often thought of as only negatively affecting vision; however, they can also help presbyopes by creating multifocality. HOAs, specifically spherical aberrations, increase depth of focus. For our presbyopic patients, correcting their residual HOAs will improve their visual quality, but it will come at the expense of reduced intermittent and near vision. In patients wanting best clarity of vision at all distances, HOA correction and a pair of reading glasses will do. For those looking to reduce spectacle use, wavefront-guided lenses can still be used in a monovision set-up.
9. Line ‘Em Up
Many shortcomings of multifocal contact lenses are due to an inability to align the optics to the line of sight. As wavefront-guided optics are inherently placed on the line of sight, accounting for lens rotation and centration, this technology can place multifocal optics exactly in the center of the line of sight. The tech makes it easy to put multifocal optics right where they are needed. This is the lowest hanging fruit of this technology, creating visual axis aligned multifocals.13
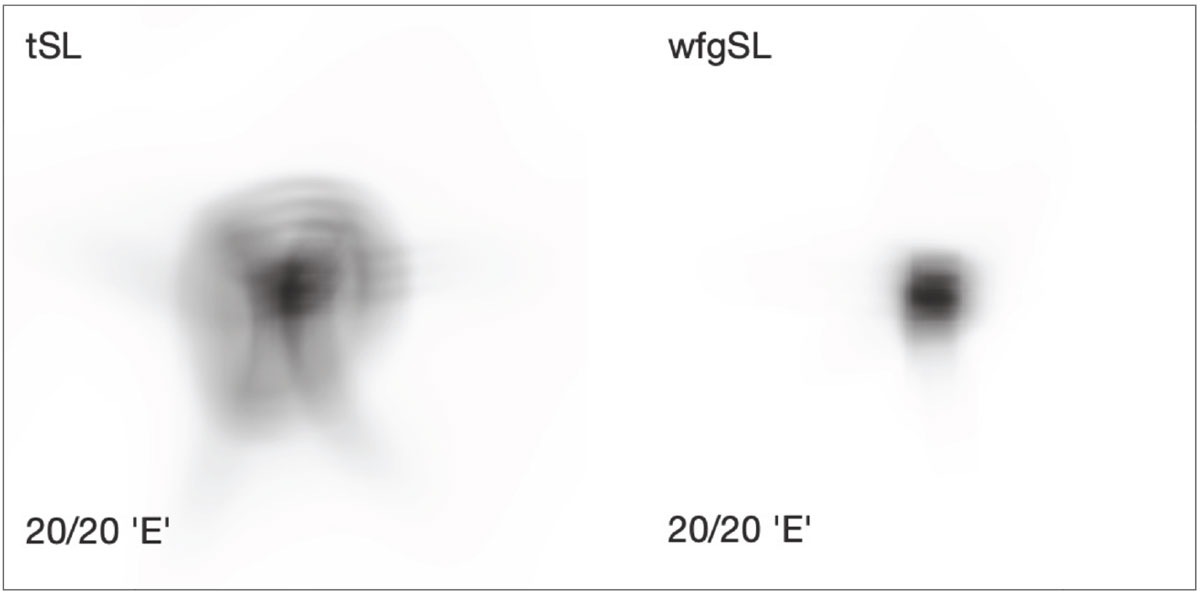 |
|
Fig. 4. Comparison of how the same patient would see an ‘E’ on the 20/20 line on a traditional Snellen eye chart. The patient gained one line of visual acuity wearing the wfgSL compared to the tSL. This is simulated using wavefront aberrometry data using a 7.8mm pupil diameter. Click image to enlarge. |
10. Induce What’s Desired
Wavefront-guided optics are primarily used to reduce residual HOAs, subsequently improving visual quality, but they can also be used to induce select aberrations. For example, unwanted HOAs can be eliminated, but with the possibility to add back in the right amount of spherical aberration to create an extended depth of focus (EDOF) and an exceptional multifocal option for patients—especially those with irregular corneal astigmatism. This option is a wavefront-guided EDOF SL. We have observed cases in our clinic where the tSL has more HOA and worse visual performance than the wavefront-guided EDOF SL.14
11. Am I Making Myself Clear?
Clear media is important, but not vital. A corneal scar or other media opacity can cause a patient to experience symptoms of smearing, ghosting or glare. Though our experience shows these patients exhibit less improvement with wfgSLs than those with clear media, improvements can still be achieved, so don’t entirely rule out these patients. In our practice, a wfgSL will be attempted for a patient with a corneal scar before performing a corneal transplant. For cataracts, though, since the procedure is commonly and successfully performed, we will readily operate on those who are ready. That said, these lenses have worked well on those with intraocular lenses and after penetrating keratoplasty.15
12. Rapid Changes
One factor that can be difficult to correct with wfgSL is rapid optical changes, such as the echelettes on a diffractive intraocular lens, intracorneal ring segments that are inside the pupil or SL optic zone edge bisecting the pupil. All of these are difficult for a wfgSL to correct, and in several patients, these implants need to be removed or exchanged. Despite this, not all intracorneal ring segments are the same—outside of the US, there are a variety of brands and models with different optic zone sizes available, ranging from 4mm to 7mm. In the US, the brand-name intracorneal ring segments, Intacs (Addition Technology Inc.), are typically used and have a larger optic zone of approximately 7mm. Our experience with patients with Intacs is that wfgSL correction can be achieved with similar results to those without.16
 |
|
Fig. 5. Comparison of the PSF of the same patient wearing the tSL (left) and wfgSL (right). This is simulated using wavefront aberrometry data using a 7.8mm pupil diameter. Click image to enlarge. |
13. To Customize or to Optimize?
WfgSL vs. eccentricity: what’s the difference and when do you use them? WfgSLs are fully customized to the individual’s HOA optical profile to correct each individual HOA. Eccentricity differs by not being customized to the individual’s profile, but instead is there to optimize spherical aberration only by changing the lens’ peripheral optical focus. If a lens with eccentricity control was perfectly centered on the visual axis, eccentricity would only alter the amount of spherical aberrations present. Do keep in mind, they can still be useful in reducing HOAs, but in our experience, to a much lesser degree.17 Our clinic uses eccentricity when the lens is not rotationally stable, as eccentricity is rotationally symmetric, so there is no impact from a lens that rotates out of position. We use this simple principle: Stable lens? Use wavefront-guided optics. Unstable lens rotation? Use eccentricity.
Takeaways
Technology such as wavefront-guided optics and elevation-specific lens design are currently creating more sophisticated lens shapes that may offer superior stability, especially when coupling them with customized optics. We are in a new era of specialty contact lenses, and device-driven technologies such as wfgSLs may serve to better the lives of the patients we care for.
Adapted from the October 2023 edition of Gas Permeable Lens Institute’s publication, The Advisor, titled “Understanding Wavefront Aberrometry and How to Take Vision from Subpar to Super with Wavefront Guided Scleral Lenses.” Join the GPLI at gpli.info to read the unabridged version and view their library of resources.
| 1. Nguyen LC, Kauffman MJ, Hastings GD, Applegate RA, Marsack JD. Case report: what are we doing for our “20/20 unhappy” scleral lens patients? Optom Vis Sci. 2020;97(9):826-30. 2. Marsack JD, Parker KE, Pesudovs K, Donnelly WJ 3rd, Applegate RA. Uncorrected wavefront error and visual performance during RGP wear in keratoconus. Optom Vis Sci. 2007;84(6):463-70. 3. Su B, Brown N, Wong J, Greenstein SA, Hersh PS, Gelles JD. Visual improvement in wavefront guided scleral lenses in keratoconus: a retrospective review. American Academy of Optometry Annual Meeting. October 2023. 4. Sabesan R, Johns L, Tomashevskaya O, et al. Wavefront-guided scleral lens prosthetic device for keratoconus. Optom Vis Sci. 2013;90(4):314-23. 5. Marsack JD, Ravikumar A, Nguyen C, et al. Wavefront-guided scleral lens correction in keratoconus. Optom Vis Sci. 2014;91(10):1221-30. 6. Hastings GD, Applegate RA, Nguyen LC, et al. Comparison of wavefront-guided and best conventional scleral lenses after habituation in eyes with corneal ectasia. Optom Vis Sci. 2019;96(4):238-47. 7. Rijal S, Hastings GD, Nguyen LC, et al. The impact of misaligned wavefront-guided correction in a scleral lens for the highly aberrated eye. Optom Vis Sci. 2020;97(9):732-40. 8. Ticak A, Marsack JD, Koenig DE, et al. A comparison of three methods to increase scleral contact lens on-eye stability. Eye Contact Lens. 2015;41(6):386-90. 9. Gelles JD, Cheung B, Akilov S, et al. Ocular impression-based scleral lens with wavefront-guided optics for visual improvement in keratoconus. Eye Contact Lens. 2022;48(11):485-8. 10. Hastings GD, Zanayed JZ, Nguyen LC, Applegate RA, Marsack JD. Do polymer coatings change the aberrations of conventional and wavefront-guided scleral lenses? Optom Vis Sci. 2020;97(1):28-35. 11. Wilting SM, Hastings GD, Nguyen LC, et al. Quantifying the optical and physical consequences of daily cleaning on conventional and wavefront-guided scleral lenses. Optom Vis Sci. 2020;97(9):754-60. 12. Chung D, Gelles JD, Greenstein SA, et al. Neural adaptation with wavefront guided scleral lenses for keratoconus. Association for Research in Vision and Ophthalmology Annual Meeting. 2022. 13. Su B, Brown N, Greenstein SA, Hersh PS, Gelles JD. Wavefront guided extended depth of focus scleral lenses in a presbyopic patient. Global Specialty Lens Symposium. January 2024. 14. Gelles JD, Brown N, Guevara A, et al. Scleral lens with novel wavefront guided extended depth of focus optics for visual improvement in a presbyopic patient with keratoconus. Global Specialty Lens Symposium. January 2022. 15. Su B, Brown N, Yu AS, Jaki N, Greenstein SA, Hersh PS, Gelles JD. Visual improvement with wavefront guided scleral lenses after penetrating keratoplasty. Global Specialty Lens Symposium. January 2023. 16. Gelles JD, Chung D, Krisa S, Greenstein SA, Hersh PS. Visual Improvement with wavefront guided scleral lenses for keratoconus after intracorneal ring segment implantation. Global Specialty Lens Symposium. January 2022. 17. Badrinarayanan A, Balakrishnan AC, Dutta R, Kumar RM, Iqbal A. Impact of scleral lens front surface eccentricity on visual acuity, contrast sensitivity, and higher-order aberrations in eyes with keratoconus. Eye Contact Lens. 2023;49(9):374-8. |


