  |
A 25-year-old female presents for a contact lens fitting. She was specifically interested in pursuing orthokeratology, having previously had a consultation for LASIK, but was nervous about potential side effects. This patient had never worn contact lenses and her main goal was freedom from spectacle wear.
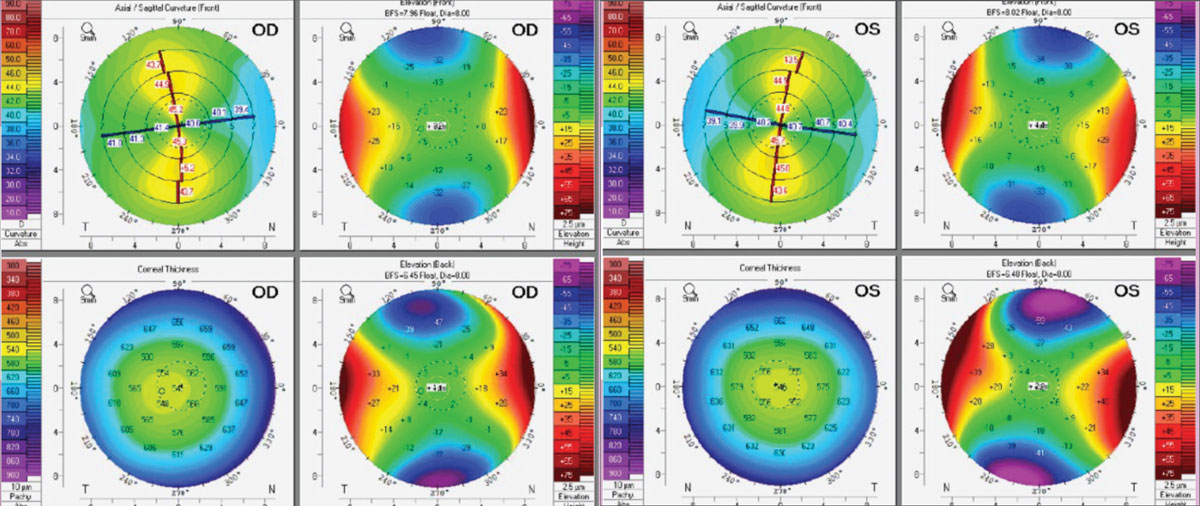
The patient presented with visual acuities of 20/20 OD and OS in her current spectacles. Her manifest refraction was -1.25 -4.75x180 OD and -0.75 -4.25x175 OS. Scheimpflug tomography (Pentacam, Oculus) showed high regular astigmatism in both eyes with corneal astigmatism measuring 4.10D OD and 4.70D OS. On slit lamp examination, there were findings consistent with dry eye, including inferior scleral show, lagophthalmos and inferior superficial punctate keratitis. The conjunctiva was white and quiet, indicating that the exposure effect was localized to the cornea.
Considerations
Here, we highlight our thought process and consider how we would proceed:
Dr. Pfeifer: My first thought when seeing this patient’s refraction was how difficult frame selection must have been. Due to the potential cosmetic concerns of a thicker lens edge in the vertical direction as well as a limited field-of-view, it is reasonable to think this patient will appreciate better vision in contact lenses, even if she is seeing 20/20 in glasses. Topography showed relatively symmetric, yet elevated corneal astigmatism with no apparent thinning or abnormal elevations or depressions, so corneal disease is likely not present at this time.
It is easy to jump to soft lenses for a young, healthy patient who is seeing well in glasses. However, the lenses available to correct her level of astigmatism are limited and the steps between powers don’t allow a great deal of customization. This leads to the option of custom soft lenses, offering a much greater customization level. Custom soft lenses, though, rely heavily on how the lens conforms to the shape of the cornea, which may not provide the best optics for this patient. Scleral lenses could also be a great option, as they are highly customizable. In addition, their stability ensures good vision, as a well-fitting lens should not move or rotate on blink. The downside with scleral lenses is added maintenance, insertion and removal technique, and a reduction in oxygen that reaches the cornea.
This leaves us with what I believe to be the best option for this patient, which are bitoric GPs. With her level of corneal astigmatism, a spherical GP would only rock along the patient’s steep meridian, leading to potential discomfort and poor vision. Conversely, a bitoric GP will align with the patient’s cornea and provide excellent vision. It is worth noting that because the patient’s right eye has less corneal astigmatism than accepted during refraction, a back toric lens with a spherical front surface may suffice. Of course, one important factor in fitting a new wearer into any corneal GP is the education that the lenses may take a little getting used to, like a new watch or a new pair of shoes would.
Dr. Su: In this case, we have an array of options at our disposal—custom soft lenses, corneal GPs, hybrids and sclerals. Custom soft lenses offer a versatile solution for most astigmatic cases with various base curves, diameters and central thicknesses. In many cases, a custom soft lens with increased central thickness may effectively mask some level of corneal astigmatism. As the central thickness increases, there is a corresponding reduction in draping, leading to a more heightened masking effect; I would want to start here. These lenses use stabilized toric haptics on the front surface to provide optimal vision correction, but in a case with 4D of cylinder, I may be more cautious of potential fluctuations caused by lens rotation.
Rigid lenses, such as corneal GPs, scleral and hybrid lenses, all rely on the tear layer to correct astigmatism which can be more forgiving for visual fluctuations on movement. When considering hybrids for over 4D of cylinder, however, concerns can arise with lens flexure. Making a toric back surface design is more appropriate to align with the corneal shape, so a bitoric corneal GP lens can be an excellent start, too. Sclerals can work as well, but in this case of a normal cornea free from pathology, handling and maintenance may not necessarily be worth it with the other great options.
Regardless of the chosen lens, it’s essential to address dry eye concerns proactively since contact lens wear can exacerbate existing dryness. Implementing dry eye treatment alongside the lens fitting can enhance overall patient comfort and satisfaction.
 |
|
Corneal tomography of the patient’s right (left) and left eyes (right). Click image to enlarge. |
Dr. Noyes: It can be easy to first jump to the suspicion of corneal ectasia when seeing patients with high astigmatism; corneal topography or tomography can be vital to ensure a correct diagnosis. This tomography reading does not imply corneal ectasia (e.g., regular astigmatic pattern, no posterior surface ectasia), just moderate to high astigmatic values. Because the patient is correctable to 20/20 in spectacle correction, my first reaction would be to try a toric soft contact lens. If vision isn’t adequate from there, I would consider moving into specialty lenses. Having said that, a scleral may be the best choice for this patient in particular, pending the level of dryness. Remember, the patient was also diagnosed with lagophthalmos and dry eye.
Dr. Gelles: High astigmatism can be a challenge. The first step, in this case, is to get topography to ensure the astigmatism isn’t corneal disease-related. Just based on the refraction, which is similar in each eye, the rule astigmatism and correctability to 20/20 make it unlikely, but at 4D of cyl, you have to check. The tomography shows no signs of corneal disease, pachs are thick, no abnormal elevations are present, and the astigmatism is symmetric. It’s just good ol’ symmetric with the rule corneal astigmatism, which mostly matches the refractive cylinder, so we know it’s normal and nearly all corneal.
There are a ton of options, but only a couple good ones. These days it’s easy to find high astigmatism soft lenses due to the vast custom soft lens options. However, lens drape and lens stability will challenge success; the optics will be very sensitive to any rotational movement.
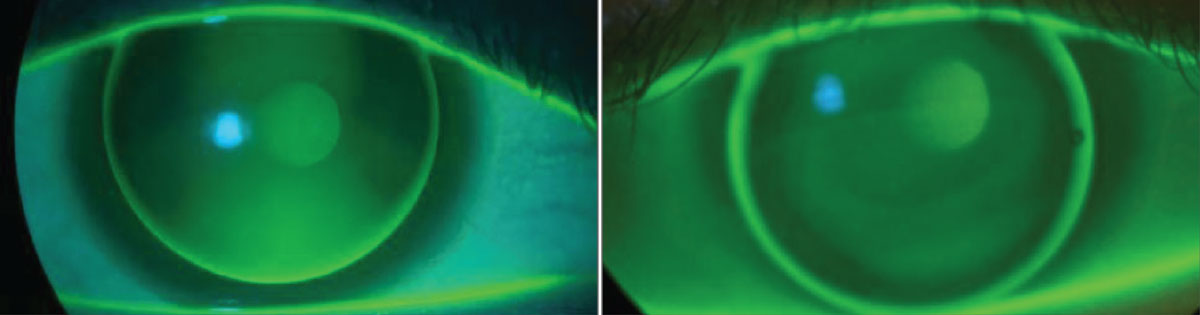
GP lenses are an ideal first choice, but let’s discuss hybrid lenses first. We know GPs can be very successful at masking corneal cylinder, and the center of a hybrid can provide just that, but the advantage of a hybrid is all in the bonded soft skirt to provide improved centration and reduced edge awareness over its corneal GP counterpart. In this case, the limbal-to-limbal astigmatism may be too much to be successful with a hybrid, potentially leading to three-nine staining due to rubbing on the nasal and temporal cornea, but you may be pleasantly surprised. If only a GP existed that could align to that cornea… bitoric to the rescue!
This would be my first choice. The toric back surface will provide corneal alignment and lens stability. I prefer a large intralimbal diameter for increased stability and minimized lid interaction. Another consideration could be a scleral lens. Though much less used for simple refractive error patients with high cyl, it can certainly be successful in this modality. As Dr. Noyes pointed out, the dryness is a consideration, and these can work wonders for dry eye patients. I typically wouldn’t start here, as there are simpler options, plus dryness is not a primary complaint and likely can be effectively managed with ointment.
I’m going with a bitoric GP on this one. It’s a classic combo: the optometric equivalent of peanut butter and jelly, milk and cookies, or coffee and doughnuts.
Discussion
Patients with a high level of corneal astigmatism can be challenging to fit with contact lenses despite the wide array of options. Contact lens correction relies on stability, and the high cyl power in the lenses can deteriorate vision if they rotate or displace. Due to the corneal alignment demonstrated by well-fitting bitoric GPs, they will stay relatively stable on blink and provide good vision. It is important to assess rotation and movement and adjust the lens, such as increasing diameter or modifying the edges to ensure stability. The wide range of fitting parameters available allow ODs to design bitoric lenses that can fit a wide presentation of corneal astigmatism.
Corneal topography can be very helpful in fitting high corneal astigmatism. Not only is it useful in ensuring there is no corneal pathology, but it can predict how a corneal GP will likely fit on the eye. It is also important to continue to perform topography scans over time to monitor for changes that may affect vision or lens fit.
Results
This patient has higher than average corneal astigmatism in both eyes. After educating her on the options, she was fit empirically using K readings and manifest refraction in bitoric RGP lenses OU (Visions Bi-Toric, X-Cel). Though the patient was able to achieve 20/20 OD and OS, the initial lenses displayed movement of 1.5mm, leading to the patient reporting ghosting of images. The diameter of both lenses was increased from 9.6mm to 10.0mm to help with stability; the ghosting was eliminated.
 |
|
Patient fit in a spherical RGP (left). Note three o’clock to nine o’clock bearing and excessive vertical clearance vs. in a bitoric RGP (right) with symmetric alignment. Click image to enlarge. |
Using a more spherical lens with this patient would have caused bearing on the nasal and temporal cornea with greater vertical movement. Use of a more toric lens increases corneal alignment and improves lens stability. When choosing a lens, it is important to consider whether the eye possesses apical astigmatism or limbus-to-limbus astigmatism. Apical astigmatism predicts greater success with spherical peripheral curves, while limbus to limbus astigmatism will likely require toric peripheral curves. With a bit of vault, a spherical base curve can be used, but with a greater amount of corneal astigmatism, a toric base curve will perform best by increasing corneal alignment and improving lens stability.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


