  |
Scleral lenses offer significant visual and ocular health improvements to our patients, especially those with corneal or ocular surface disease. This article will focus on the scleral lens landing zone, specifically problems with tissue compression.
Causes and Effects
Tissue compression is the result of a misaligned scleral lens landing zone or a landing zone that is not wide enough to evenly spread the force the lens exerts on the conjunctiva. Both excessively steep and flat lenses are capable of creating these issues.
There are a variety of short-term effects of a misaligned scleral lens, including discomfort, arcuate staining, vascular compression (blanching/impingement) and rebound injection after lens removal. If scleral lens misalignment persists over the long term, the previously mentioned effects can be exacerbated and conjunctival hypertrophy development is possible.
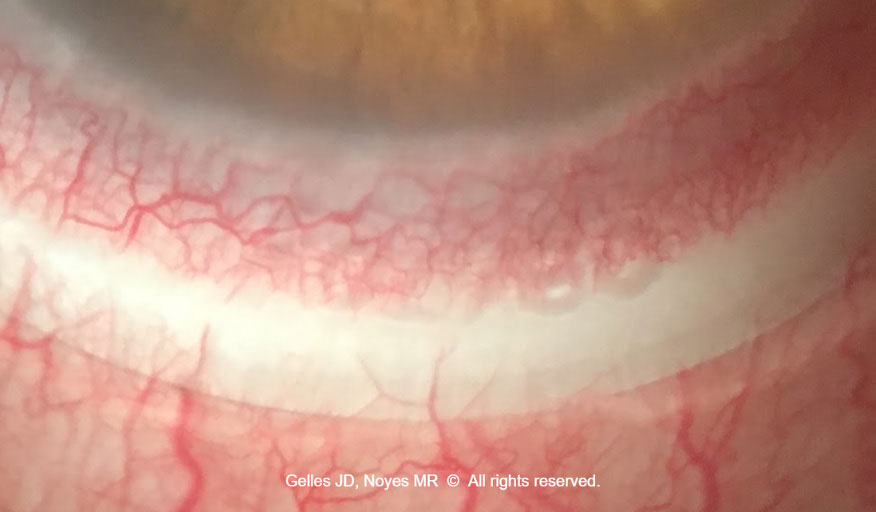 |
| This scleral lens landing zone displays severe (fine and large vessel impingement) conjunctival compression. The left edge of the lens is too flat (note the 0.5mm band of compression located 0.5mm from the lens edge), and the right edge is too steep (note the compression starts at the edge and extends 1mm inward). To improve this landing zone fitting relationship, steepen the left side and flatten the right side by using a toric periphery. Click image to enlarge. |
Identification
Accurately identifying the region of vessel compression will aid in troubleshooting. Additionally, detailed documentation of this information will help in communicating with laboratory consultants to make lens modifications.
Techniques can be repeated for lens-on and lens-off evaluation, such as with diffuse white light, direct beam and cobalt blue (with and without vital dyes, with and without holding the lids) to observe findings such as pooling, injection, staining, compression and shadows.
First, note the position of the scleral lens markers, typically indicated by dots or dashes on the lens surface, by noting the axis they fall on (horizontal dashes are located at 0° and 180° and dots are located at 270°, for example).
Document the vessel compression in relation to the following:
- lens edge (e.g., “at the lens edge extending 1mm inward” or “2mm in from the lens edge and 1mm wide”)
- severity of vessel compression (e.g., “fine vessels are blanched” or “fine and large vessels are fully impinged”)
- location of compression by axis (e.g., “compression is located from 0° to 90°”)
- periodicity of compression (e.g., “even compression 360° around,” “compressed in two areas 180° apart,” “compressed in a single area” or “compressed focally over a conjunctival obstacle”)
- conjunctival tissue movement (e.g., “the conjunctiva is free moving under the landing zone edge” or “the conjunctiva does not move at the landing zone edge with digital movement through the eyelid”)
Using direct white light illumination at a 45° angle to evaluate across the lens (beam on the nasal side to evaluate the temporal landing zone), note the appearance of the lens edge (e.g., “a shadow is cast from the lens edge indicating the edge is lifted” or “no shadow is cast from the lens edge and conjunctival heaping is present indicating the edge is too steep”).
Application of vital dye, either sodium fluorescein or lissamine green, will also aid in identification. With the lens on, note whether there are any locations of dye pooling vs. freely flowing under the landing zone edge and if there are adjacent signs of conjunctival folding/staining/heaping. After lens removal, note any rebound injection (both severity and pattern) and if a conjunctival impression ring is present (if so, indicate its severity, depth, width, location and periodicity). Repeat the use of vital dye to assess conjunctival staining. All findings should corroborate the issues with the initial lens fit.
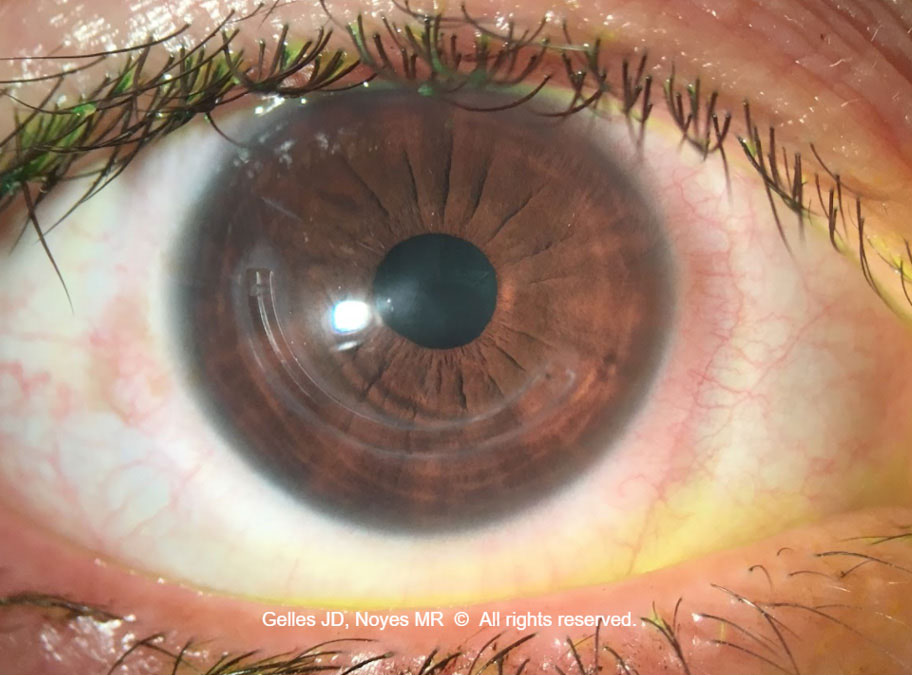 |
| Note the deep conjunctival impression on the nasal side of the scleral lens post-removal, with corresponding grade two nasal conjunctival rebound hyperemia. On the temporal side, the conjunctival impression and rebound injection signs are less impressive and the hyperemia is more focal. To improve the landing zone alignment, incorporate a quadrant-specific landing zone flattening the nasal quadrant more than the temporal, increase the landing zone width to spread the lens pressure more evenly and consider adding a focal peripheral elevation to the temporal side at the location of the hyperemia. Click image to enlarge. |
Problem-solving
If the scleral lens fitting relationship shows compressed vessels at the lens edge, the landing zone is too steep. This can be resolved by flattening the edge (i.e., reducing the angle at which the landing zone contacts the globe). If the compressed vessels are not at the lens edge but rather located inward from the edge, the landing zone is too flat and can be fixed by steepening the edge (i.e., increasing the angle of the landing zone).
If the area of compression is relatively even 360° around the landing zone, flattening or steepening the entire landing zone will help. If the compression has a pattern, such as equal compression at 0° and 180°, use a toric haptic. If the compression is unequal or located at a single quadrant, then a quadrant-specific design can be used.
If there is focal compression due to pathology, such as pressing against a pinguecula, incorporating a peripheral edge elevation can help vault this pathology. In mild cases, a simple increase or decrease in lens diameter can overlay a very shallow pinguecula or avoid contact altogether. In some cases, notching a lens (focal removal of lens material) can be effective; however, this can be accompanied by adjacent tissue desiccation. Of course, the use of topography-guided or impression-based scleral lens designs may also aid in these situations. If there is deep circumferential conjunctival compression with rebound hyperemia on lens removal, consider increasing the landing zone width to distribute the lens force more evenly.
Additionally, note where the deepest point is located (inward from where the lens edge indicates an excessively flat landing zone and directly at the lens edge indicates a steep landing zone).
If the lens fitting relationship is left too steep for a longer period of time, noted by development of conjunctival hypertrophy, it is wise to prescribe a topical steroid and discontinue lens wear until improvement is observed. Once improved, refit the patient paying special attention to correcting lens alignment in the affected area. Keep the following in mind: a large-diameter lens to overlay the affected tissue or a small-diameter lens to avoid it.
Tips & Takeaways
|
Conclusion
Keen observation, documentation and communication are key to successful scleral lens landing zone troubleshooting for conjunctival compression. Remember, laboratory consultants are not wizards; they can’t magically make you a perfect lens based on poor descriptions. Use these tips for the best results all around.


