  |
A 56-year-old man presented with a history of keratoconus OS>OD. He had a history of corneal crosslinking OU and has been wearing corneal RGP lenses for approximately 10 years, reporting discomfort OU.
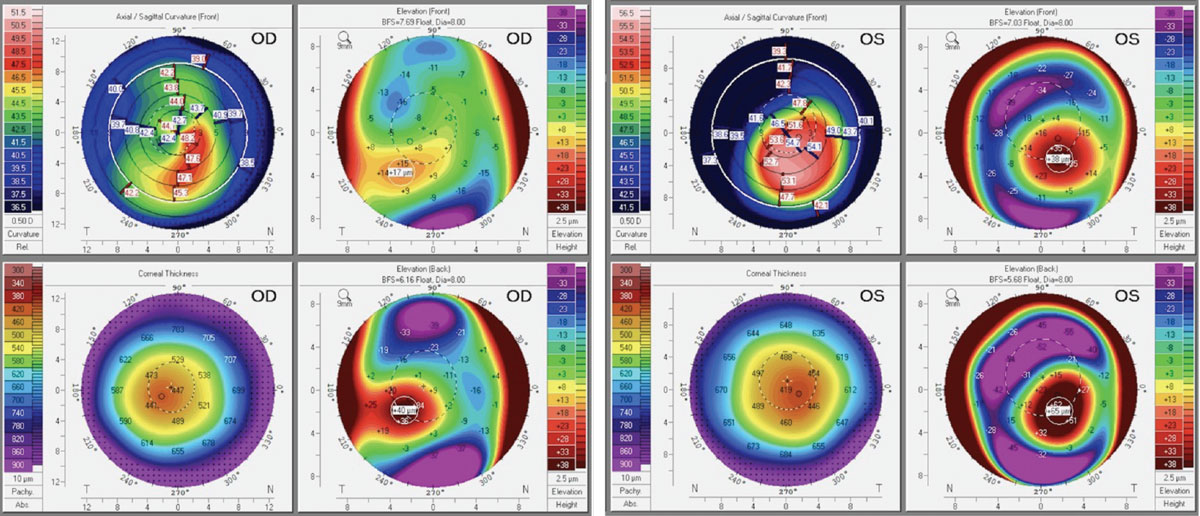
His entering acuity with habitual RGP lens wear was 20/30 OD and 20/25 OS. On manifest refraction, he was best-corrected to 20/40 and 20/50 with a prescription of pl-4.00x090 in the right eye and -0.50-5.50x110 in the left. Scheimpflug tomography (Pentacam Wave AXL, Oculus) showed an IS ratio of 4.00D in the right eye, 12.00D in the left eye and a maximum keratometry reading of 48.50D and 55.60D in the right and left eyes, respectively.
On slit-lamp evaluation, there was no significant corneal haze or scars present. His bulbar conjunctivas were white and quiet with small focal nasal and temporal pingueculae on each eye.
 |
|
Fig. 1. Corneal tomography of the patient’s right and left eyes. Click image to enlarge. |
 |
|
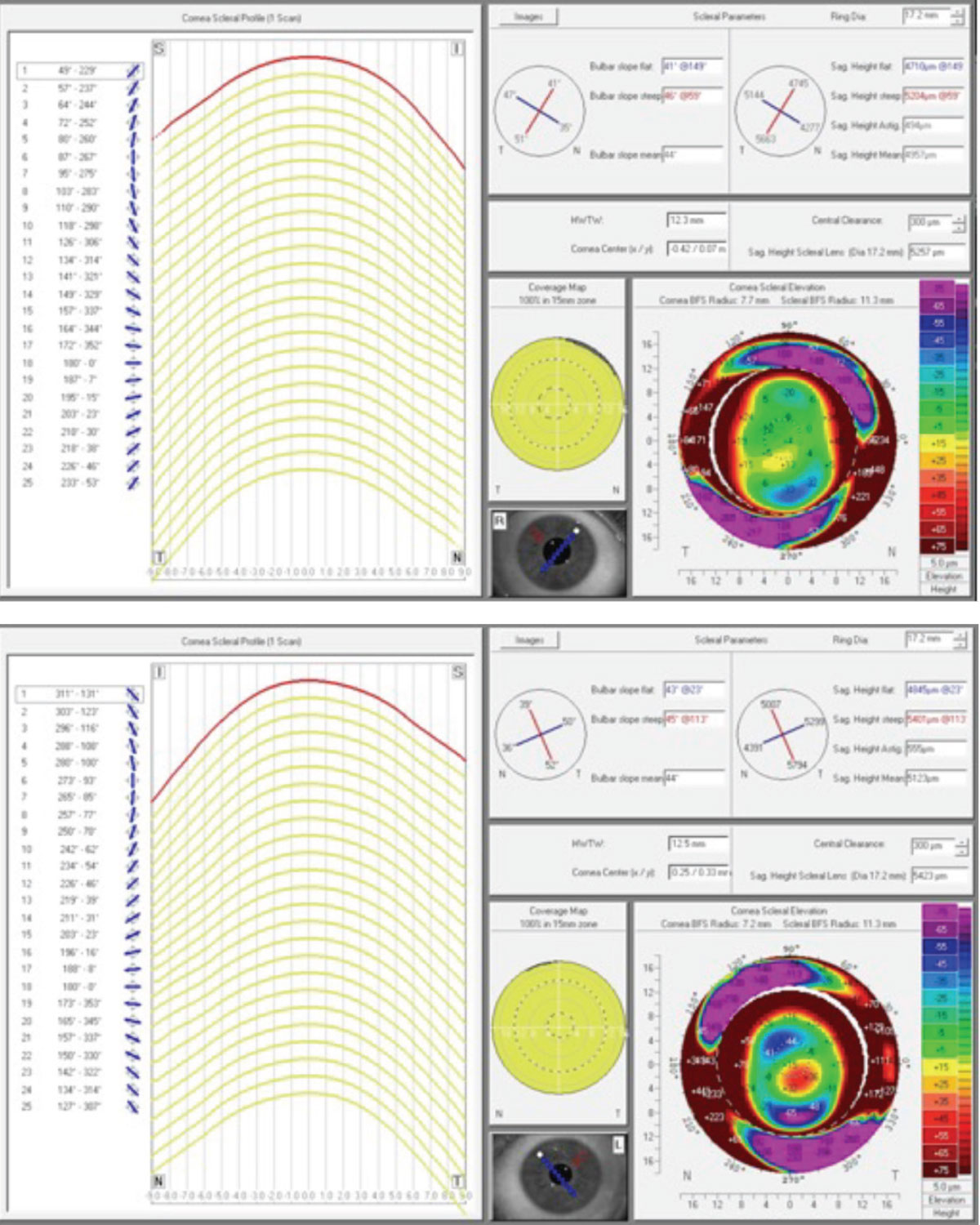
Fig. 2. Corneoscleral profilometry of the right (top) and left (bottom) eyes. Click image to enlarge. |
Considerations
Here, we highlight our thought processes and consider how we would proceed:
Dr. Su: This patient has a history of wearing corneal RGPs and reporting poor comfort with them. Looking at his tomography maps, it may be possible to refit the right eye with the same lens modality to improve the comfort. Refitting the left eye with another RGP may be more difficult, since the keratoconus is more severe and the IS ratio may cause the RGP to rock on the eye, making it less stable. If the patient is comfortable with switching lens types for both eyes, I would refit with a scleral, as this would likely improve comfort. As for the pingueculae, a scleral that lands on the elevation may also cause discomfort and irritation.
Another option would be to avoid the pinguecula altogether—this could be achieved by making the lens smaller. I usually don’t like to start with this selection, though, as a smaller lens may put more pressure around the conjunctiva and subsequently cause irritation. Comparatively, the use of a larger lens provides the ability to better spread out pressure over a greater surface area. There are also options to microvault and notch, but depending on the ocular shape and size of the lesion, this may take a few lens iterations. Looking at his ocular shape from the profilometry scans, he has a lot of scleral toricity which can make the fit more complex, even in the absence of the pingueculae. To save chair time and increase first-fit success, there are newer methods like impression-based scleral lens designs and scan-based designs using scleral profilometry—if available, I would start here.
Dr. Pfeifer: Given this patient’s history of successful RGP wear, my initial inclination would be an attempt to improve the fit of his RGPs to reduce his symptoms of discomfort. Though his keratoconus is more severe in the left eye, the anterior elevation differences in both the right and left eyes are below 350µm, thus predicting some degree of success in RGPs. Reducing the lens diameter, steepening the edges to reduce excessive movement or even just incorporation of a coating are all options that may dramatically improve his symptoms. Pingueculae can be a difficult bump in the road when fitting lenses, but a corneal RGP lens would perform well by avoiding these elevations altogether.
Conversely, a scleral lens may indicate compression over these areas that can often lead to discomfort. If the lens edge is flattened to avoid this compression, you run the risk of tear exchange around the edge of the pinguecula, which could not only lead to discomfort, but also post lens fogging. However, if the patient is unable to tolerate RGP wear, scleral lenses are still a viable option to pursue. In this case, my ideal lens would be a smaller diameter to avoid the elevations entirely. A larger-diameter lens incorporating a vault, notch or lift also has potential to be considered, taking the pressure off of the lesions. The downside of choosing a larger diameter is that it may require some troubleshooting to correctly orient the lens modification and vault the pinguecula.
There is also the option of an impression-based or a profilometry-based scleral lens. These more advanced options offer a higher degree of customization to accommodate these lesions; they would also account for the irregularity of this patient’s scleral toricity to improve overall lens fit. Ultimately, the patient’s motivation to either improve his current lens modality or try a new one will help guide how to proceed.
Dr. Gelles: If a scleral lens is the right lens modality for a patient with a pinguecula or another type of elevated obstacle, it will require the use of a focal custom haptic modification, such as a notch, peripheral elevation or channel. Typically, having to create a complex haptic shape takes longer. Using a scan-based scleral lens can be ideal in these cases, as it will get us much closer to an endpoint than the diagnostic lens-based design. But what if we are in a practice that does not have a device capable of capturing corneoscleral profilometry or even one that uses scleral lenses? This case could be handled in a variety of ways.
The first and simplest option to consider in the absence of sclerals is to create a piggyback system. This is achievable by taking a low plus power standard soft lens and placing it on the eye, then placing the patient’s habitual corneal RGP on top of it. This can be trialed in the office, with the benefit of receiving immediate feedback from the patient. Even if this doesn’t turn out to be the final choice, it could still give the patient improved comfort for the time being, as they wait for another lens design to arrive.
The next possible option would be the use of a hybrid lens, which may provide more comfort for the patient by improving lens stability and reducing lid interaction with the lens. Another reason to choose this design is because the soft skirt will contour to the pinguecula—no need for complex haptics.
Generally, if a patient is already struggling in a lens modality, I do not prescribe the same type of lens. However, if a corneal RGP is desired using scan-based software, it can be employed to make a freeform corneal RGP, which may elevate lens performance through improving fit and stability. If I am going to use the same lens modality, I make it a priority to educate the patient that the lens I am creating is designed by an entirely different process than the one they currently use. I don’t want them to feel as if I am repeating options that have previously been tried and failed. Making sure to communicate this builds a higher level of trust and understanding.
This does require a corneal topographer capable of exporting data to lens design software, but I am going to assume that anyone prescribing or designing specialty contact lenses has a corneal topographer.
Discussion
Pingueculae may present difficulties during scleral fittings. Compression of the lens on the lesion(s) can cause a suboptimal fit, leading to discomfort and potential long-term complications. Collaborating with laboratory consultants and using advanced options to customize the lens haptic can ensure that it conforms to these obstacles, guaranteeing comfortable and healthy wear over time.
Results
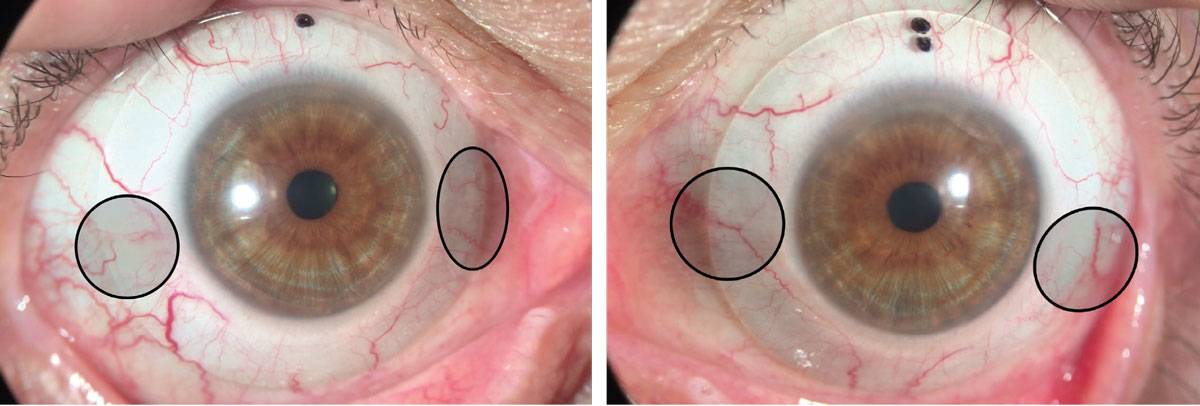
The patient was diagnostically fit with a larger diameter, 19.0mm scleral (BostonSight Scleral), originally without special focal haptic modifications. Later, SmartChannels were added to help relieve pressure on each pinguecula. He was best-corrected to 20/25 OD and 20/20 OS. On follow-up, he reported good vision, but was experiencing fogging of the lenses after only three hours of wear. He also had an impression ring in both eyes with localized redness on the nasal side. Slit lamp findings showed the landing of the scleral lens on the nasal pinguecula with adjacent edge lift. Corneoscleral profilometry scans from the initial visit were reviewed and scan-based scleral lenses (BostonSight Smart360 Scleral, BostonSight, Needham, MA) were ordered for each eye.
At the subsequent follow-up appointment, the patient was able to achieve 20/20 vision OD and OS, reporting no more issues with lens fogging. He also experienced good comfort while wearing the lenses for 10 hours a day.
 |
|
Fig. 3. Final scan-based sclerals. Note the lack of vessel compression over the small nasal and temporal pingueculae. Click image to enlarge. |
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


