 |
Over time, clinicians have realized that corneal diameter, not corneal curvature, is the most influential factor of a patient’s sagittal depth.1 The average horizontal visible iris diameter (HVID) is 11.6mm to 12.0mm, but only 50% of patients fall within this range.2 This means that the other half of the patient population is wearing contact lenses that do not fit well and are either too large or too small for a patient’s eye.
This is where custom soft contact lenses can save the day by providing smaller or larger diameter fits depending on patient needs. These lenses can be a challenge to fit, and clinicians often have to start by making an educated guess about initial lens parameters. But practice makes perfect, and, with each custom lens you fit, you will be able to more accurately gauge what your patient needs. The following case discusses a patient who, despite having megalocornea—a condition in which the corneal diameter is larger than average—is motivated to try contact lenses.
The Case
A 42-year-old male presented with a history of advanced congenital glaucoma. He recently had a Descemet’s stripping endothelial keratoplasty (DSEK) in his right eye due to a failing endothelium. In an attempt to improve his peripheral vision, he was interested in trying contact lenses. When he was a young adult, he wore rigid gas permeable lenses (RGPs) but stopped due to discomfort issues and his inability to adapt to the lenses.
He was using Alphagan P (brimonidine tartrate, Allergan) OU BID as well as Systane eye drops (polyethylene glycol and propylene glycol, Alcon) as needed. He was not taking any oral medications. His health history was unremarkable.
He wore glasses with a prescription of -2.75+1.75x133 OD and -2.50+1.50x030 OS. His presenting visual acuities (VAs) were 20/25 OD and 20/40 OS.
A slit lamp exam revealed clear lids, lashes and conjunctiva and deep and quiet anterior chambers OU. The right cornea revealed a DSEK, but it was otherwise clear. The left cornea was also clear. The iris was normal, and the lenses exhibited trace nuclear sclerosis OU. An undilated posterior segment evaluation revealed a cup-to-disc ratio of 0.9 OU, with everything else falling within normal limits. The patient’s intraocular pressures were 19mm Hg OD and 20mm Hg OS. Topographical imaging showed simulated keratometry (K) readings of 41.81/40.03@125 OD and 41.83/40.24@035 OS and large HVIDs of 14.4mm OD and 14.8mm OS (Figure 1).
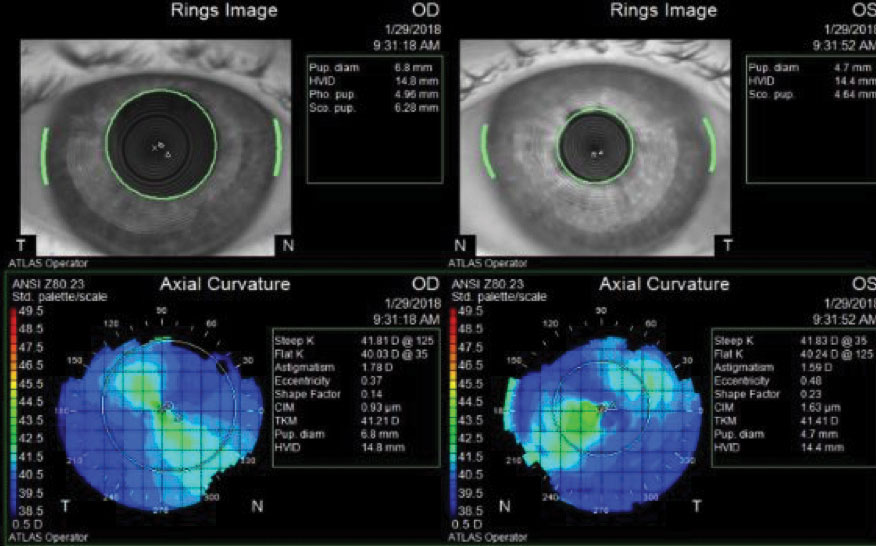 |
| Fig. 1. Imaging reveals this patient’s HVIDs fall outside the normal range, at 14.4mm OD and 14.8mm OS, suggesting the need for custom contact lenses. Click image to enlarge. |
Contact Lens Evaluation
Manifest refraction revealed:
- 2.75+1.75x125 (VA of 20/25) OD
- -3.25+1.75x045 (VA of 20/30-) OS
After I discussed contact lens options with the patient, he was interested in pursuing soft lenses due to his previous experience with RGPs. As an avid mountain biker, he was looking for a lens with better stability.
By adding 3.0mm to the HVID to calculate the lens diameter (i.e., a 12.0mm HVID requires a 15.0mm lens), the patient would need a 17.4mm lens OD and a 17.8mm lens OS. Adding 1.5mm to each side of the lens helps ensure lens stability.1
The soft lenses customized by our labs max out at 16.0mm. Kontour makes lenses with large diameters but doesn’t produce toric lenses larger than 16.0mm. After discussing options with colleagues, I found I could order toric lenses with large diameters from Visionary Optics.
To design the lenses, I made an educated guess for the base curve (BC), adjusting it due to the increase in arc length associated with the diameter change. For a normal-sized cornea of 11.8mm, a keratometry reading of 40.00/42.00 would require a BC of 8.8. Increasing the arc length would require a steeper lens to compensate for the change in sagittal depth and keep the same cornea fitting relationship. I also rounded up on the diameter to improve the stability of the toric lens.
I chose a steeper BC on the left eye due to its slightly larger corneal diameter. I ordered Methafilcon A soft XP toric lenses with the following parameters:
- 8.4/-1.00-1.75x035/17.5 OD
- 8.1/-1.50-1.75x135/18.0 OS
Contact Lens Dispensing
A week later, I placed the lenses on the patient’s eyes. The right lens covered the cornea, but the scleral coverage was short, and the lens fluted significantly. The left lens also exhibited excessive fluting, although not as severe, but the centration and scleral coverage were both adequate. The left lens was placed on the right eye to assess the fit of a larger diameter and a steeper BC. The lens was centered, had good scleral coverage and showed less severe fluting. An over-refraction was unobtainable because the lenses did not lie flat on the cornea.
I steepened both lenses and ordered a larger right lens in a second set with the following parameters:
- 7.9/-1.00-1.75 x035/18.0 OD
- 7.9/-1.50-1.75 x135/18.0 OS
Redo Contact Lens Dispensing
The second set of lenses was placed on the patient a week later. Both lenses had good centration, coverage and movement with no fluting OU. The patient’s vision was 20/25 OD and 20/30+ OS. His over-refraction was plano OU.
The patient was trained on insertion and removal techniques before he was sent home to try the lenses.
Follow-up
The patient presented a week later reporting good comfort and vision with his new lenses, so his prescription was finalized.
Discussion
When designing custom soft lenses, clinicians should calculate the lens diameters using the HVID + 3.0mm formula and add more wiggle room for toric designs to ensure better stabilization. At minimum, clinicians should plan for a 1.5mm overlap on either side of the cornea, with 0.5mm to 1.0mm of movement on primary gaze. The majority of patients with larger corneal diameters require lenses that are large, steep and deep; whereas, most patients with smaller corneas require small, flat and shallow lenses. In this case, because the patient’s HVIDs were above average, an educated guess with diagnostic lenses was the only way to find the appropriate fitting relationship between the lens and the patient’s cornea.
Also remember to adjust the BC of the lens to steepen larger lenses and flatten smaller lenses. Many topographers can help calculate the sagittal depth of the lens and assist labs in calculating the BC.
Knowing how to properly fit corneas that fall outside of the average HVID of 11.6mm to 12.0mm can add value to your practice and promote patient loyalty. Patients who are not successful with traditional soft lenses and do not have a significant ocular surface disease don’t have to walk away from contact lens wear. They will likely benefit from a custom fit, especially if they have a high astigmatism, an oblique axis astigmatism or a desire for more precise multifocal optics.
|
1. Young G. Ocular sagittal height and soft contact lens fit. Cont Lens Anterior Eye. 1992;15(1):45-9. 2. Caroline PJ, Andre MP. The effect of corneal diameter on soft lens fitting, part 1. Contact Lens Spectrum. www.clspectrum.com/issues/2002/april-2002/contact-lens-case-reports. Published April 1, 2002. Accessed July 27, 2018. |


