|
A 33-year-old Hispanic male presented for a first-time contact lens fitting OU complaining of blurry, fluctuating vision and glare at night with his habitual glasses from three years prior. He noted a recent diagnosis of keratoconus and was subsequently referred to our contact lens service. We confirmed the diagnosis and discussed the option for corneal crosslinking (CXL) prior to a contact lens fit. The patient declined CXL due to cost, but was interested in seeing better, especially when driving at night.
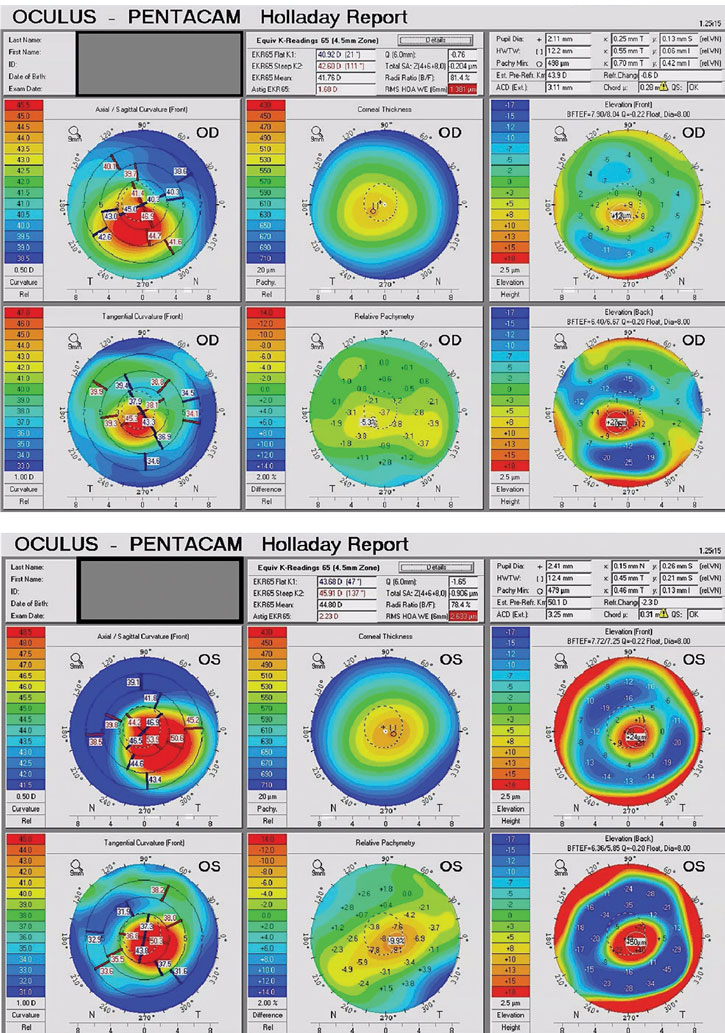
Entering vision was OD 20/40 and OS 20/50 in spectacles. All other entrance testing was within normal limits. The patient’s Pentacam (Oculus) maps showed simulated keratometry readings of OD: 42.5/44.2@110 and OS: 46.9/48.7@129 (Figure 1). While the keratometry may appear normal OD, the ectasia was confirmed by assessing the abnormal Kmax, abnormal back surface elevation, reduced pachymetry values and elevated BAD-D value in each eye.
The manifest refraction was OD: +0.25 -1.00x090 and OS: -1.25 -2.50x150 with a distance BCVA of OD 20/30 and OS 20/40. Near VA reached 20/30 in each eye with the same refraction.
Assessment
 |
|
Fig. 1. Pentacam tomography maps for the patient in this case. Click image to enlarge. |
From the topography or tomography maps, I like to evaluate the tangential map and elevation map to determine a starting lens. From this patient’s elevation map, we could assess the likelihood of success with a corneal lens (vs. the need for a scleral lens design) and predict to some degree what the sodium fluorescein pattern of the corneal lens will look like (Figure 1). If the sagittal height difference on the elevation map (height map) at an 8mm chord is <200µm, there is a good chance the patient can be fit in a corneal lens. If the sagittal height difference on the elevation map at an 8mm chord is >400µm, there is little chance we will be successful (and we might as well start with a different lens design). This patient fits neatly into the first category, and I was reasonably confident we would be successful in a RoseK2 design. It is important to keep in mind that all corneal lenses are limited by this sagittal height differential.
Slit lamp evaluation revealed a Fleisher ring along with Vogt striae centrally in each eye. There was no central corneal scarring, but thinning was evident and consistent with keratoconus and the patient’s global pachymetry maps on the Pentacam.
 |
|
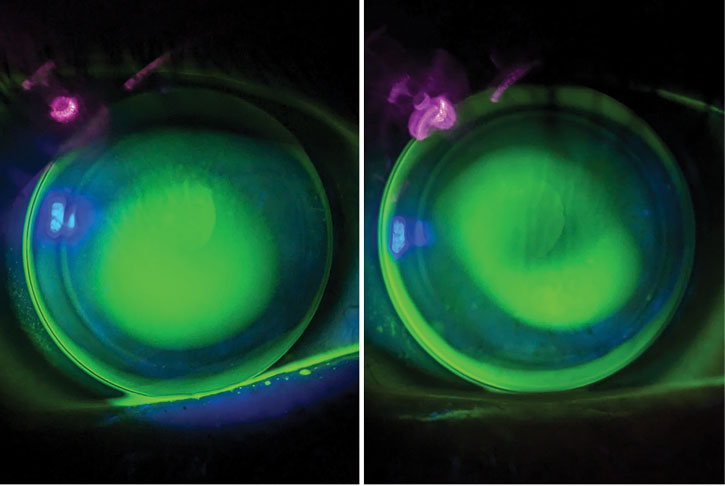
Fig. 2. Final lenses show adequate fit centrally (apical clearance OD, left, feather touch OS, right) with relatively even edges provided by toric peripheral curves. Click image to enlarge. |
Lens Refit
The patient was fit with RoseK2 corneal lenses (Blanchard, CooperVision Specialty Eye Care) OU. I chose this lens because, based on the tomography maps, I was anticipating that he may need a toric peripheral curve to achieve an even landing on the cornea. The RoseK2 lens was designed by Paul Rose of New Zealand. It is an aspheric design and has a customizable landing zone, including both toric and asymmetric corneal technology options. The lens design is typically fit diagnostically, using keratometry readings and a fitting set. Our practice is fortunate to have several fitting sets and diameters to choose from.
I tried the following diagnostic lenses OD: 7.50/9.2/-2.00DS and OS: 7.10/9.0/-2.00DS. With an over-refraction, the BCVA was equivalent to that achieved in spectacles at OD 20/30 and OS 20/40. The fit was steep OS, and I considered adding in a toric periphery but opted to see how the first pair went without it. Despite minimal improvement in Snellen acuity with the lenses, the patient was happy with the quality improvement achieved in diagnostic lenses and was hopeful that would assist him with night driving.
A custom lens order was placed for RoseK2 with parameters OD: 7.50/9.2/-2.00DS/Optimum Extra (Contamac) in green and OS: 7.20/9.0/-3.00DS/Optimum Extra (Contamac) in blue.
Follow-ups
At the follow-up two weeks later, the patient did not wear the lenses to the office, noting he had hardly worn them at all, except the day following his appointment. He described extensive difficulty with lens application due to having shaky hands. The frustration was so much that he gave up and discontinued wear. We used this visit to retrain application and removal procedures, which the patient succeeded at once again. We assessed the fit and decided to proactively place an exchange order in each eye. We saw the patient back in two weeks.
There, we dispensed the new lenses. The patient had not worn the first pair much and once again forgot some of the application and removal procedures. We reviewed them and provided a suction cup remover should he need it. At this visit, we measured a -0.50DS over-refraction in each eye that only subjectively improved vision to add the toric peripheral curves in each eye: OD 0.8mm and OS 1.2mm. We scheduled a one-month follow-up visit and elected to hold off on the reorder for now.
At the follow-up, the patient came in wearing the lenses. He was much happier because of his continued success with application and removal. He felt like the lenses lessened his symptoms of glare and halos at night and overall was happy with his vision. He was well-adapted and did not have any comfort concerns. We confirmed he was following proper cleaning procedures with Clear Care (Alcon). There was now no over-refraction in either eye, with the patient rejecting the -0.50DS over each eye found at the last visit.
At this visit, we did note the presence of peripheral 3-9 staining in each eye; however, the patient was not using any lubricating eye drops. Slit lamp assessment revealed a reduced tear film break-up time of four seconds in each eye. We advised the patient to start instilling contact lens–compatible lubricating eye drops four times daily and we would follow-up in four weeks for further dry eye evaluation and to gauge the level of improvement in 3-9 staining.
Have these important reminders handy while fitting your next patient with GP lenses. First, choose a lens wisely and consider all your options. We often overlook corneal lenses these days, but if the sagittal height dictates, go for it! Second, treat dryness along with GP lens wear (and it would be a great idea to check the patient’s dry eye status before you even being a fit.) Finally, consider holding off making small power changes until the neophyte patient is fully adapted to lens and wear. Chances are that over-refraction will change—and may even disappear—once they are comfortable.