 |
A few recent cases have reminded me of Occam’s razor—the idea that the simplest explanation is usually the correct one (also known as the “law of parsimony”). The first patient presented with a sudden-onset painful eye and the second presented with sudden-onset blurry vision in both eyes. Can you guess the culprit in each case?
Is It a Foreign Body?
 |
|
Curvilinear pattern highlighted by sodium fluorescein dye. It is overlying an area of existing corneal scarring from keratoconus. Click image to enlarge. |
A 25-year-old male presented to our Urgent Care service complaining of a sudden-onset painful right eye since applying his habitual GP lens. He noted associated light sensitivity, redness and tearing with pain rated a seven out of 10. After removing the lens, the pain improved to a four out of 10. He thinks he may have scratched his eye.
The patient has a history of keratoconus OU with associated scarring OS>OD. He only wears a GP lens OD, which improves vision to 20/25. He does not wear a lens OS, and vision is 20/500. He was using a GP multipurpose solution to clean the lens and rinsed it with water before application. A penetrating keratoplasty had been recently recommended for the OS, but the patient is deferring the procedure due to work obligations.
He was wearing a ComfortKone (Metro Optics) design with parameters OD 5.40/8.5/-22.50/A24. One of our ocular disease residents was concerned about a curvilinear pattern of staining on the cornea that looked like a foreign body. However, no foreign body was visible in white light. The upper lid and lower lid were everted with no foreign body present. The resident had already irrigated the eye with no improvement in symptoms.
After consulting with the resident, the main concern was the corneal staining pattern. They had several lofty ideas of what may have caused the staining, including threads in the eye, an eye injury or even Acanthamoeba because of the water use. After a few open-ended questions, I asked the resident if the patient had brought the lens in question and asked they retrieve it.
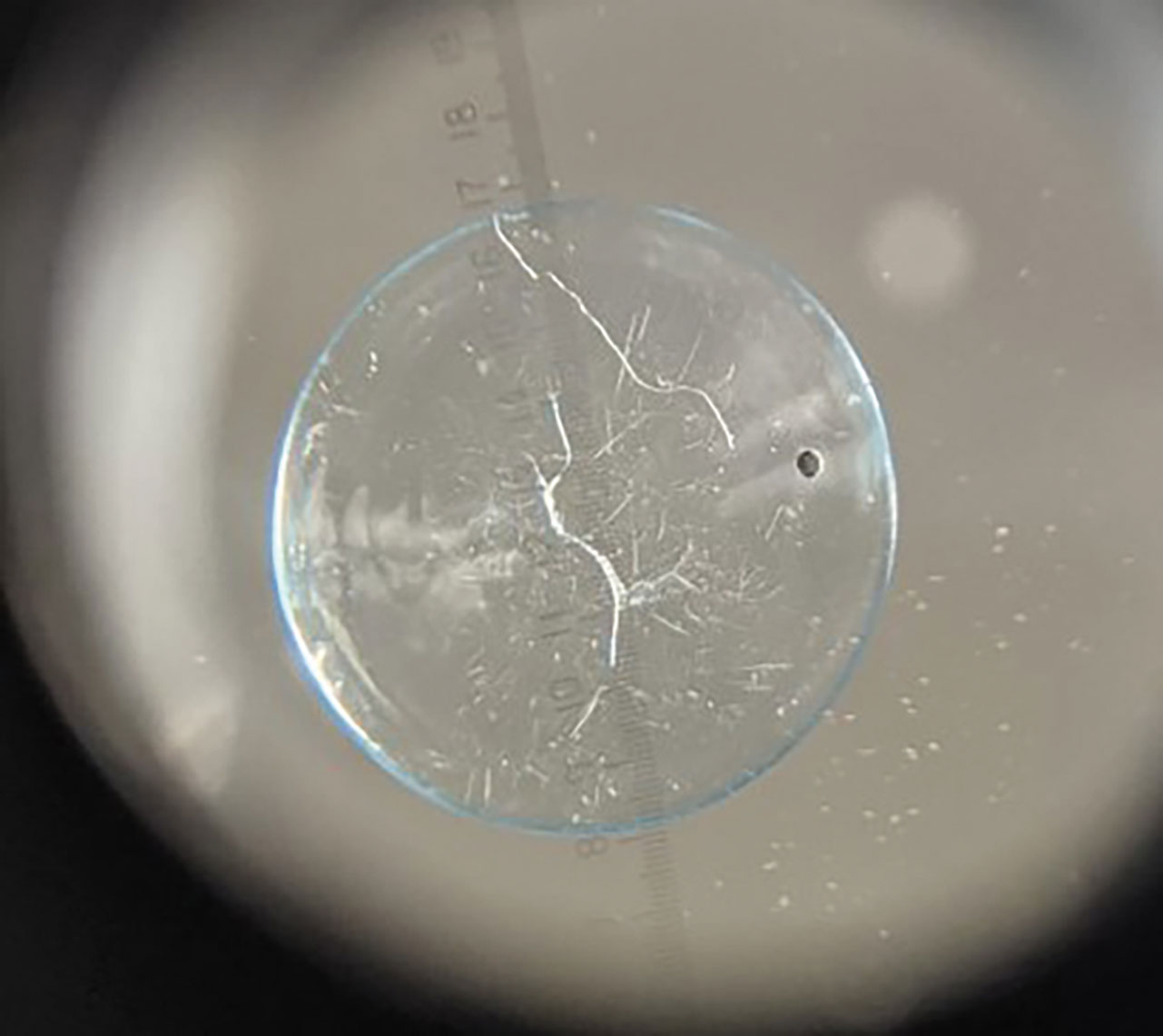
I carefully removed the lens from the case and placed it on our 7x magnifier. Sure enough, there were several cracks through the lens, one of which matched—almost exactly—the staining pattern present. Problem solved!
A cracked or damaged GP lens is obviously undesirable and not suitable for wear. Clinicians should remind patients to inspect their lenses for damage each day before application. This means visually inspecting the lens on the finger for any cracks, edge chips or foreign material. Once the overall integrity of the lens is confirmed, it can be conditioned and applied to the eye. Any cracks or damage can cause eyelid or corneal irritation or injury.
If a lens is damaged on the eye or during wear, the patient will usually notice a sudden change in vision. They may have been able to remove only part of the lens fragments. Should this occur, obtain a sufficient case history to piece together the situation at the time of lens loss, but also then instill sodium fluorescein to aid in locating any remaining lens fragments. Upper and lower lid eversion and careful evaluation are crucial. Irrigation may also help clear any additional foreign debris from the fornices.
This patient’s corneal abrasion was treated, a new lens was reordered and lens aftercare procedures were reviewed, with stress on avoiding contact with tap water moving forward.
 |
|
A cracked lens (seen here, concave side down on a 7x magnifier) caused the corneal staining pattern with the previous image. Click image to enlarge. |
Is It Supposed to Be "Left Blue?"
A patient with keratoconus called the emergency line to report sudden onset blurry vision OU after applying a new pair of duplicate lenses they had recently picked up from the office. To try and fix the problem, he removed the lenses, cleaned them and re-applied but to no avail.
He tried putting in his old lenses and reported clear vision. He inquired as to whether his lenses can be exchanged with the lab or if he should come in for a follow-up visit.
We arranged to see the patient and he denied any issues with lens comfort. He had worn the lenses about four hours on this day and felt like vision was now worse OS. The lenses ordered were a spherical GP lens (Art Optical) design with parameters OD: 8.25/9.2/-2.50/Optimum Extra/green and OS: 8.25/9.2/-1.75/Optimum Extra/blue. The patient had seen 20/20 out of these lenses in each eye at his most recent annual evaluation, at which time the prescription was duplicated.
One of our students worked up the patient and found entering vision of OD 20/25+2 and OS 20/40 with an over-refraction of OD -0.25 and OS +1.00 which improved VA to 20/20 OD and 20/20-3 OS. The student evaluated the lenses on-eye, noting an appropriate fit. After the patient removed the lenses, the student astutely noticed the lens on the right side of the case appeared blue and the lens on the left side of the case appeared green, suggesting the lenses were switched.
Indeed, the simplest explanation strikes again! We reviewed how the over-refraction result and improvement in vision seen confirms that the lenses were swapped. We proceeded to switch the lenses back, and our (somewhat embarrassed) patient returned home none the worse for wear.
When troubleshooting patient complaints, look for the horses—not the zebras. The fix may be relatively simple on our end, providing major relief to our patients at a time of great concern and worry on their end.


