 |
With myopia management becoming a newly recognized standard of care (per the 2021 World Council of Optometry Resolution), orthokeratology (ortho-K) is becoming more mainstream in eyecare practices worldwide.1 While used in myopia management for children, ortho-K can also be useful for correcting standard ametropia in adults seeking an alternative to spectacles, daily wear contact lenses and/or refractive surgery. If the adult patient is presbyopic, further consideration should be given to whether correction will be for distance vision (with use of reading glasses for near as needed), near-only (with use of supplemental glasses for distance) or monovision (correcting one eye for distance and one for near with the ortho-K lenses, with the possibility of needing glasses for intermediate vision and/or driving).
 |
|
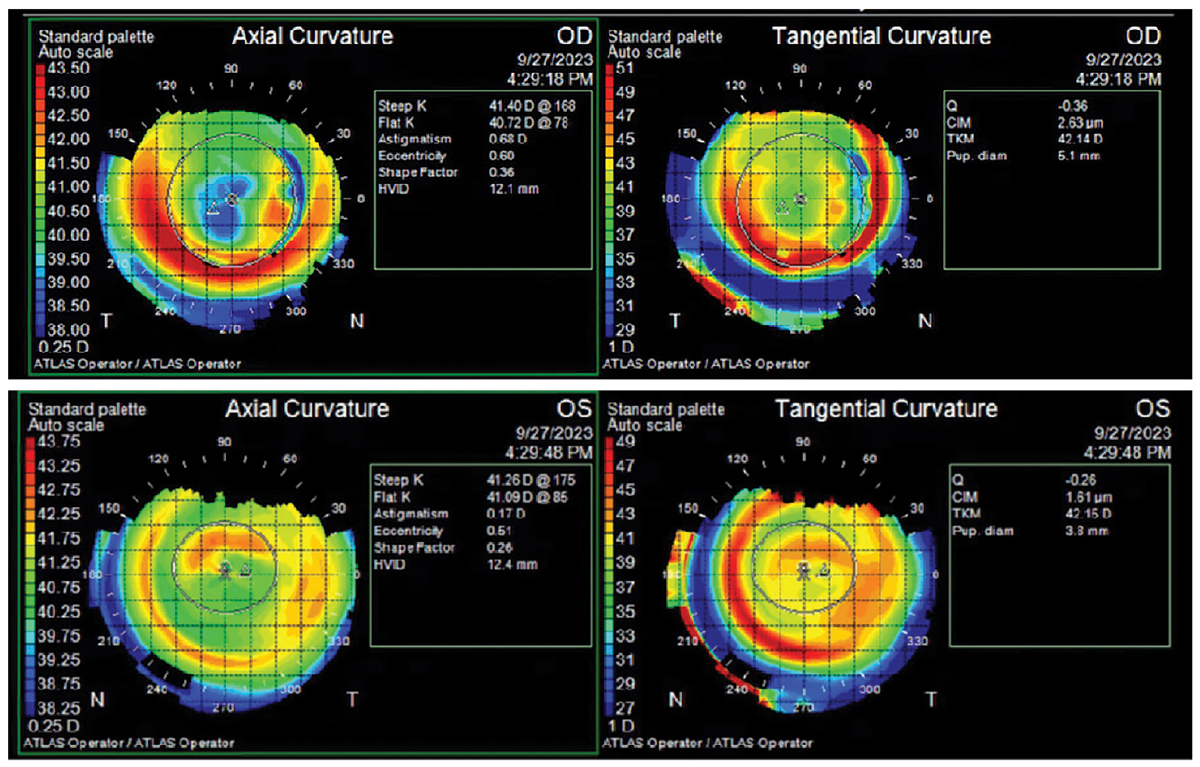
Topography (Humphrey Atlas) maps of entering ortho-K lens result showing a less distinct treatment zone OS (the near eye) on the tangential map (right). Click image to enlarge. |
Monovision ortho-K is highly customizable and can be adjusted to give the patient more “span” (or difference) between the two eyes as needed. Best practice for monovision ortho-K fitting involves determination of the myopic patient’s best manifest refraction, near add at the preferred working distance and dominant eye. From there, lenses can be ordered empirically or fit diagnostically from a fitting set. For the distance eye, the fit does not change from the typical procedure used in pediatrics, with a base curve flatter than the cornea at a level equivalent to the amount of spherical myopic refractive error plus a compression factor or “Jessen factor,” which is added correction to account for natural regression toward myopia that occurs after lens removal and over the course of the day.2,3 For near, the targeted correction is reduced by the amount of the patient’s add power so that the near vision is maintained at the near point.
Keep in mind, the patient may complain (even if the fit is as you intend) of loss of intermediate vision; this is consistent with the use of monovision. You can choose to adjust the base curve to compensate for this, but you may alter the patient’s near visual acuity (VA) in the process. We recommend allowing distance VA to stabilize for two weeks. Then, perform an in-office over-refraction using the monocular in a binocular field approach, with loose lenses at the preferred working distance in order to determine the best add power for the non-dominant eye.
 |
|
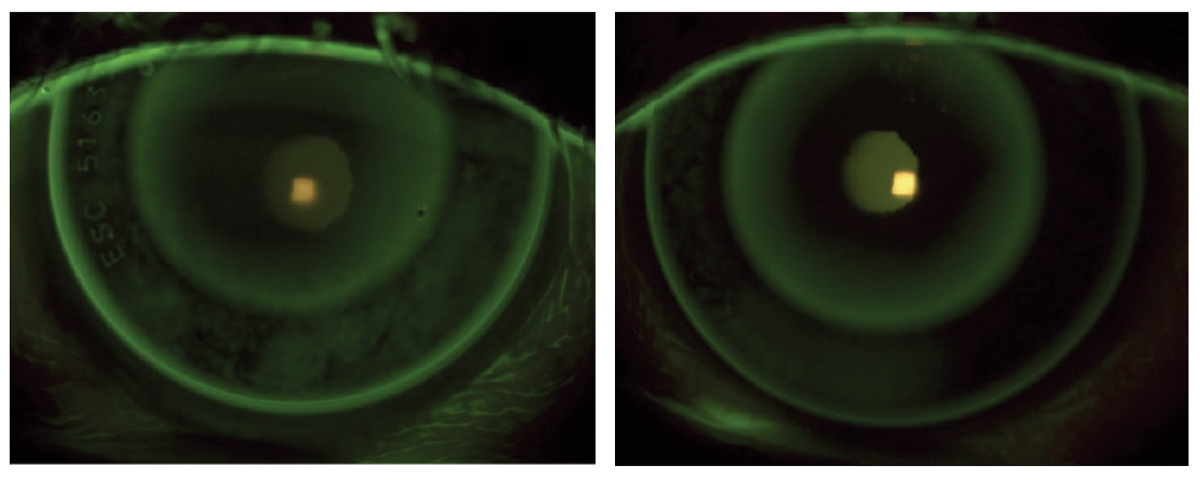
Entering lens fit in each eye (right eye distance, left eye near) showing a fairly similar bull’s-eye pattern in each eye. Click image to enlarge. |
Patient Case
A 57-year-old African American female was fit with monovision ortho-K lenses at an outside office approximately 10 years prior. Her pre-fit refraction was OD -3.75 -1.50 x 085 and OS -4.25 -1.50 x 085. She had been a patient at our practice for many years with several lens adjustments made throughout, including a full refit into distance-only lenses in 2020 with readjustment of the near add following. She reported being generally happy with both distance and near vision since that time but still used +1.25 readers for “very small” print. Her main struggle was with intermediate VA and her goal was to be less reliant on reading glasses. Of note, one solution here could have been to have the patient use dissimilar adds or combining the lenses in two pairs of readers.
The monovision in this case was OD distance (the dominant eye) and OS near. The patient could achieve fairly good uncorrected distance VA in each eye with her habitual lenses worn at night. The Emerald Ortho-K lenses (Euclid Vision Corporation) gave entering uncorrected VA of 20/25 OU at distance and 20/30 OU at nearby late afternoon. The refraction was OD PL and OS -0.75DS with a +2.00 add.
 |
|
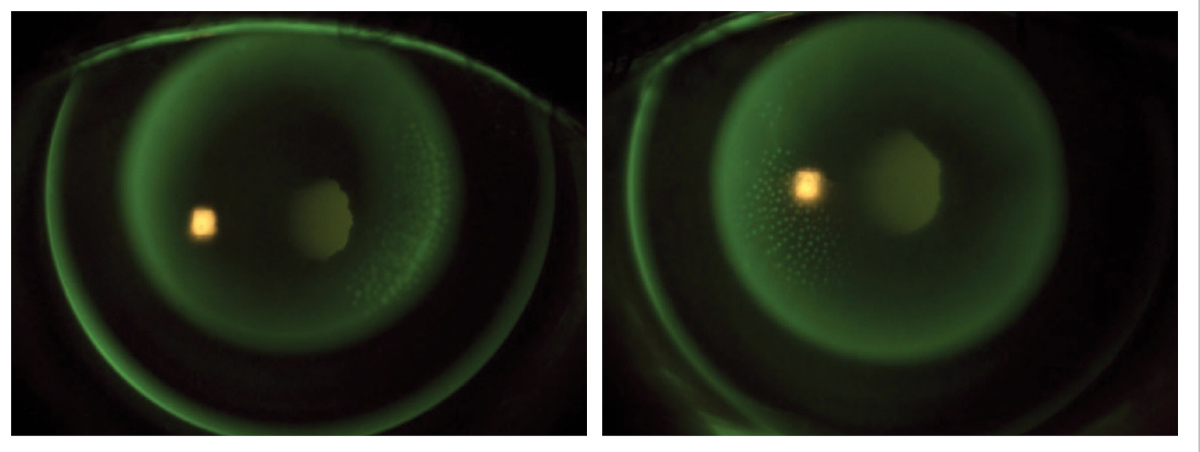
Final lens fit in each eye (right eye distance, left eye near). Dimple veiling is visible in the reverse curve nasally in each eye. The OS treatment zone is less distinct as this is the near eye. Click image to enlarge. |
The lens parameters were OD +0.75DS/8.85 BC/10.60 diameter and OS +0.75DS/8.54 BC/10.60 diameter (cc 20/20-2 OD, OS). The refraction over-lens was +0.50DS OD and -1.00DS OS. The overall lens fit showed a bull’s-eye pattern in each eye, and the topographies showed a centered treatment zone (though less distinct OS). (For reference, the initial BC OS was 9.0 to achieve true distance VA OS and was steepened to 8.54 to give the monovision OS near correction).
With the help of laboratory consultation, we worked to further increase the difference in correction between the two eyes since the entering distance VA was fairly similar and the patient complained of lack of intermediate VA. The goal was to achieve a “truer” monovision resulting in reduced distance VA OS in order to improve intermediate and near VA OU.
The new lens parameters were OD +0.75DS/8.85BC/10.60 diameter and OS +0.75DS/8.28 BC/10.60 diameter. With the new lenses worn for one night, daytime uncorrected distance VA remained 20/20 OD and was reduced (as anticipated) to 20/30 OS. At near, VA was 20/40 OD and 20/25+ OS. The refraction over-lens was +1.00DS OD and -1.50DS OS. The overall lens fit showed a bullseye pattern in each eye, with slight central pooling OS, as expected due to the steepened base curve adjustment.
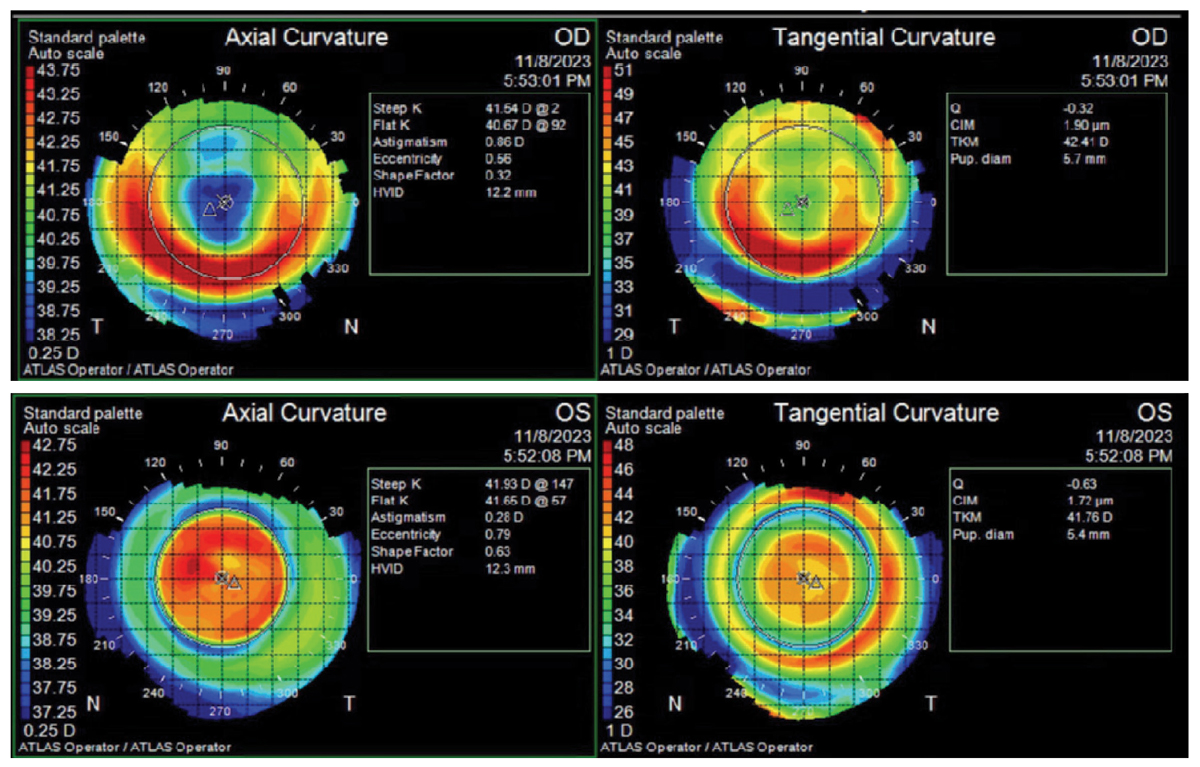
After wearing the new lenses for two weeks, the patient came back with distance uncorrected VA of 20/20 OD and 20/30 OS. At near, the VA was 20/40 OD and 20/25 OS. The O/R was consistent with that at the one-day visit. Topographies reflected a well-centered treatment zone for distance in the right eye, with a centered area of steepening in the left eye. The patient was overall satisfied with the improvement in near and intermediate VA.
 |
|
Topography (Humphrey Atlas) maps of new ortho-K lens result showing central steepening OS (the near eye), which corresponds to improved near acuity in that eye. Click image to enlarge. |
At one-month follow-up, she presented with stable uncorrected VA. Her refraction was OD PL and OS -1.50DS. The main concern was that she was no longer able to use her +1.25D readers for the computer due to asthenopia OS. She was happy with the overall improvement in intermediate vision and felt more freedom from needing the glasses. Loose lens over-refraction was performed at the computer and resulted in +1.50 OD and plano OS. We prescribed this for computer glasses, but the patient could also easily trial it by popping out the OS lens from a pair of readers.
Monovision ortho-K can be a great option for presbyopes who do not want to wear contact lenses during the day. Patient selection is important, as is education that a loss of intermediate vision is possible—especially with increasing add powers. Despite this caution, monovision ortho-K can (mostly) free presbyopic patients from reliance on daytime distance correction and should be a consideration in presbyopes who are resistant to full-time wear of reading glasses
The authors thank Abbey Cantolina at Euclid Vision Corporation for her assistance with this case.
1. World Council of Optometry. Resolution: The Standard of Care For Myopia Management by Optometrists. Accessed January 14, 2024. https://myopia.worldcouncilofoptometry.info/standard-of-care/. 2. Michaud L, Marcotte-Collard R, Simard P, Ouzzani, M. The Contact Lens Evidence-Based Academic Report (CLEAR) Guidelines. Managing Myopia (1st ed.). Dougmar Publishing Group. Accessed January 14, 2024. 3. Chan B, Cho P, Mountford J. The validity of the Jessen formula in overnight orthokeratology: a retrospective study. Ophthalmol Physiol Opt. 2008;28(3):265-8. |


