|
When fitting any type of gas permeable (GP) contact lens, issues with dryness and non-wetting can arise. They can often occur if a patient has a poor-quality tear film, improper lid hygiene or lens handling or demonstrates non-compliance with the prescribed care regimen. Lens fit and care system changes along with periodic lens replacement can help address these concerns.
Case One
A 23-year-old Hispanic male with keratoconus presented for a contact lens evaluation wearing ill-fitting, three-year-old GP corneal lenses. He noted occasional dryness with his lenses but found relief with occasional use of artificial tears.
We diagnostically fit and ordered a new pair of aspheric corneal lenses with the addition of a toric peripheral curve system. Toric peripheries are indicated when topography suggests the steeper inferior cornea is inferiorly displaced and causes the lower edge of the lens to lift up and irritate the lower eyelid.1 The patient achieved 20/20 vision OU, but, a few weeks later, he again complained of increased dryness and discomfort OU during the latter half of his daily wear time. The patient did admit he was not rubbing the lenses with the multipurpose GP lens cleaning solution for the recommended length of time at night.
After adding sodium fluorescein, we noted moderate staining on the temporal side of each cornea, closer to the limbus. This type of staining can occur in keratoconic patients who may have dry eye associated with atopic disease and meibomian gland dysfunction. Other causes of 3 o’clock and 9 o’clock staining are a thick edge profile or a high axial edge clearance.1 We observed minimal edge clearance in the horizontal meridian of the lens, as opposed to high clearance (Figure 1).
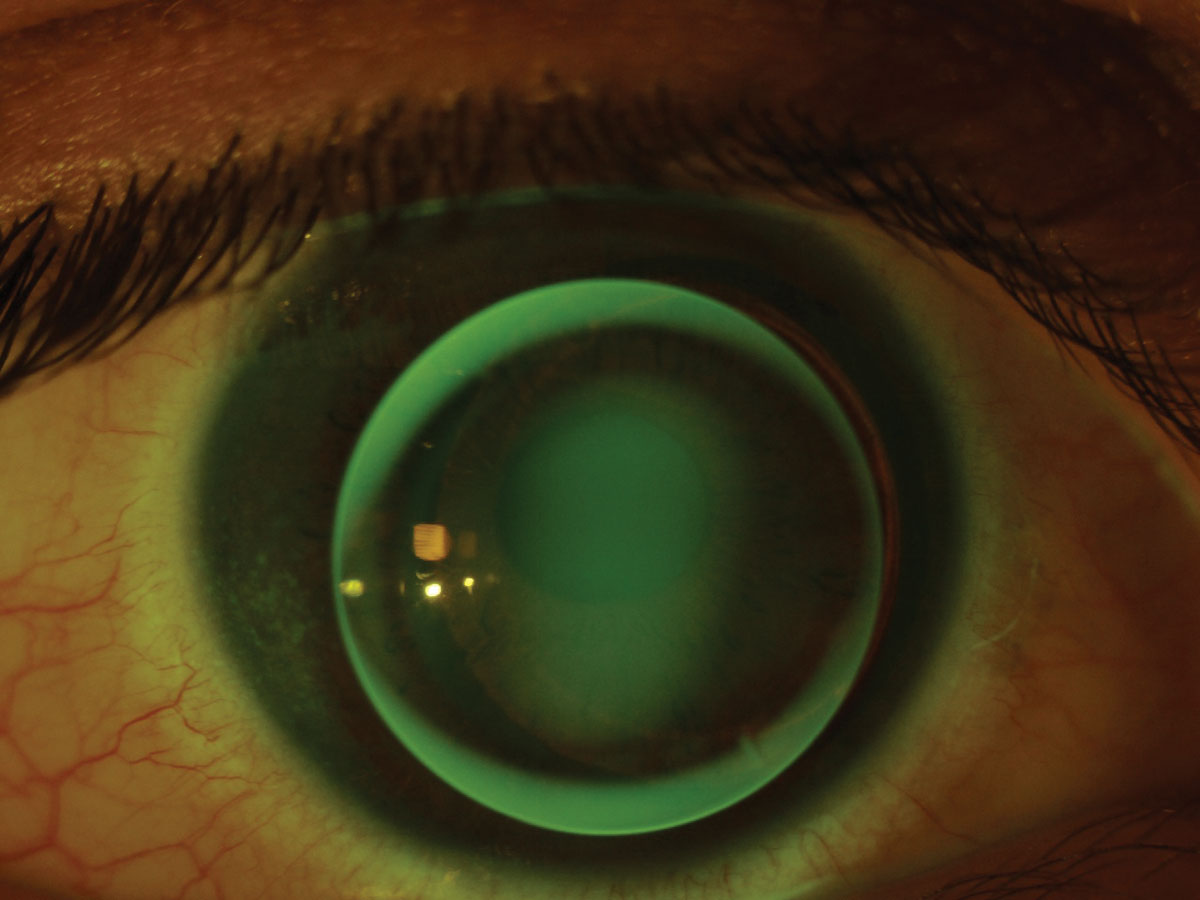 |
| Fig. 1. Temporal corneal staining present at follow-up on a keratoconic corneal GP lens. Click image to enlarge. |
We reordered the lens with a flatter edge and an increased toricity (1.3mm) in the periphery to improve comfort. We also initiated aggressive lubrication at nighttime, recommended warm compresses and proper lid hygiene and then reviewed proper rubbing with the multipurpose GP solution. Upon follow-up of the re-designed lens, the staining resolved and symptoms improved. The patient successfully wore the lenses for the following 18 months.
If 3 o’clock and 9 o’clock staining are present, increase the lens’s overall diameter. This will cover more of the cornea, reduce exposure and improve comfort. Ensure appropriate edge thickness, edge clearance and movement. Address any tear film abnormalities with tear supplementation and blinking exercises.2
Case Two
A 40-year-old African American male presented for his annual evaluation wearing a piggyback system for keratoconus OU. He complained of fogginess and reduced vision in the right eye that had been getting worse over the past six months. Vision in the left eye was stable, and the patient had recently purchased a replacement GP lens for that eye after breaking it when cleaning it a month ago. The blur OD was constant through all 16 hours of daily wear. He did not adhere to the recommended rubbing steps in either regimen due to fear of lens breakage. There was some apical scarring OS, limiting best-corrected vision. The tear break-up time was normal at 15 seconds per eye.
The patient’s entering acuity was 20/50 OD and 20/300 OS. There was independent movement of both the soft lens and GP lens on each blink. The entering OD GP lens was showing extensive surface deposits (Figure 2). Factors that cause deposits include lens replacement frequency, hand contamination and tear film properties of the patient.3 The most common tear-derived lens deposits are proteins and lipids, which in-office cleaning can remove.3
Laboratory-grade cleaning solution in-office cleaned the GP lenses, leading to visual acuities 20/30 OD and 20/125 OS. Despite the improvement, we still recommended that a new GP lens be ordered for the right eye.
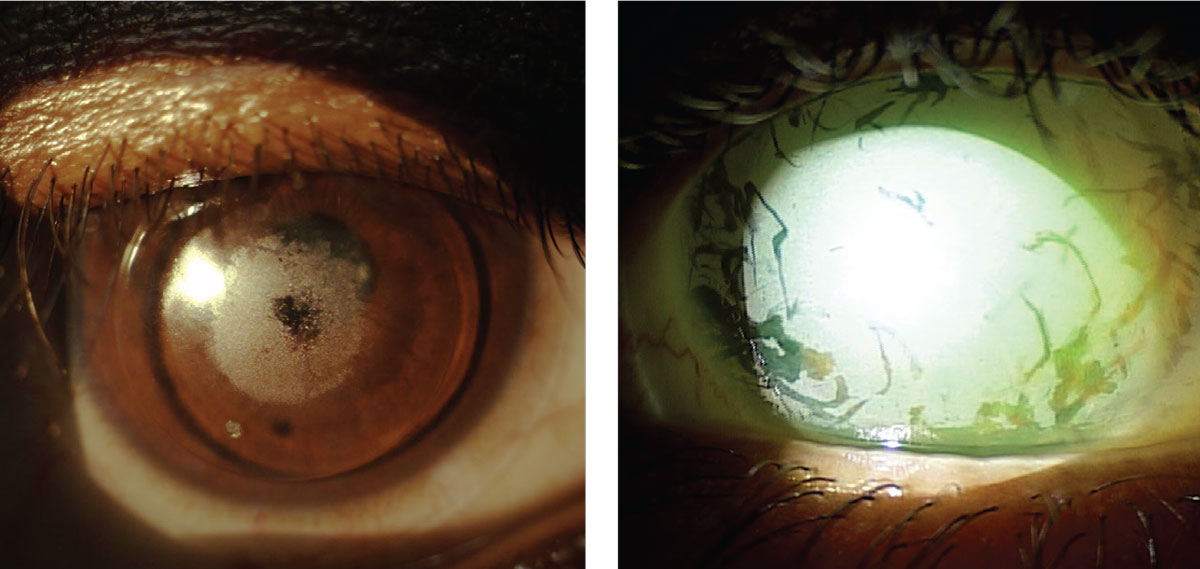 |
| Fig. 2 and 3. Piggyback system with large central area of non-wetting on the GP lens (left). Extensive front surface non-wetting on a 16.0mm scleral lens (right). Click image to enlarge. |
We reviewed with the patient proper lens care and hygiene, including how to properly rub the GP and soft lens to clean each appropriately without excessive force. The patient switched to a hydrogen peroxide-based care system. By using two cases, he could use the same solution for each of the four lenses, reduce confusion and increase adherence to our recommendations.
While GP lenses have a negligible water content and high modulus of elasticity that contribute to their long life expectancy, replace them periodically to ensure optimal wettability, comfort and vision.1,4,5
Case Three
A 30-year-old Asian male presented one year overdue for an annual evaluation of his spherical scleral lenses. He was experiencing blurry vision OU at distance and near and had recently broken his habitual two-year-old scleral OD. He had a history of bilateral keratoconus and was s/p deep anterior lamellar keratoplasty OD, and s/p corneal crosslinking OS with a complicated toric intraocular lens (IOL) implant OS. The ocular surface showed extensive tear film debris, reduced tear break-up time of three seconds and punctate conjunctival staining OU.
We had the patient apply the lens in-office for evaluation and found his entering acuity with the lens in place was 20/70 OS. The patient had been able to achieve 20/20 OS the year before with this spherical lens, which was unusual at the time, considering we expect to employ a front toric scleral design for full correction in a patient with a toric IOL. No over-refraction improved the acuity in this case, presumably due to the severe non-wetting. (Figure 3).
Tear film debris and poor lid hygiene, as well as lack of adherence to the prescribed cleaning regimen, were all contributing factors. We prescribed Clear Care (Alcon) nightly and advised the patient to fill the lens with preservative-free 0.9% NaCl inhalation saline for insertion. Instead, he used Boston Advance (Bausch + Lomb) cleaning solution with no conditioner and did not heed our recommendation of monthly Progent (Menicon) use.
This non-wetting did not improve, even after use of in-office laboratory cleaner. We recommended the patient continue with his habitual spectacles until receiving his new pair of sclerals. A less oxygen permeable material could improve the wettability, and adding a surface coating might improve the lens’s surface properties.
When investigating signs of dryness in the setting of any type of GP lens wear, it is crucial to determine the root cause of the problem. There can be ocular surface- and lens-related causes for any associated symptoms. In the case of untreated or undertreated dry eye disease, consider changing to a preservative-free care system or adding lubricating drops, gels or ointments. More aggressive management of any associated ocular surface disease is a boon to continued, ncomfortable lens wear. Don’t forget about the lens surface either, as any areas of non-wetting can cause reduced vision and discomfort and warrant immediate lens cleaning or replacement.
1. Sorbara, L. Correction of keratoconus with GP lenses. Centre for Contact Lens Research, University of Waterloo. 2010. 2. Bennett ES, Weissman BA, ed. Clinical Contact Lens Practice. 4th Ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2005. 3. Efron N. Contact Lens Complications. 4th Ed. Philadelphia, PA: Elsevier; 2019. 4. Efron N. Contact Lens Practice e-Book. Elsevier Health Sciences. 2016. 5. Jones L, Woods CA, Efron N. Life expectancy of rigid gas permeable and high water content contact lenses. CLAO J. 1996;22(4):258-61. |