In today’s digital age, the majority of people interact with near vision targets and screens on a daily basis. Therefore, it has become critical that their vision correction options meet those demands, whether those are work-related or recreational tasks. Progressive spectacles have become one of the most popular methods of management, offering a stable optic that allows patients to focus on targets at different working distances by looking into different zones of the lens with variable powers. This creates a challenge for contact lenses by comparison, which have the disadvantage of being on the eye. As a result, many commercially available soft lens multifocal options utilize a gradual, aspheric and often center-near multifocal optic.
When someone views a near target, accommodation is stimulated along with the rest of the “near triad” including pupil constriction. Many soft multifocal designs take advantage of this, using a center-near add power to give the patient the ability to focus on that near image.1 Due to the contact lens being fixed in position on the patient’s eye, they are unable to look into a different optical zone to view through a different power and must view the optics simultaneously; however, this carries a couple inherent design flaws. The first is that the patient does not have the ability to search for a “sweet spot” or zone of the lens where they can find the desired power for the working distance they are viewing. Another issue is that performance of the multifocal is pupil-dependent which leads to problems in suboptimal lighting conditions. The final problem is that, in the case of center-near multifocals, the patient must suppress the bifocal power when viewing at distance and may ultimately find the distance vision a bit blurry. This central distance viewing issue is avoided in the dominant eye with monovision; however, the issue of reduced stereopsis is then introduced.
Another pitfall of monovision is the need for clear vision at three distances far: distance, the intermediate distance of computer screens and near when clear focus can only be given to two of them between both eyes. Additionally, if a soft multifocal decenters on the eye, the optics are displaced, which disrupts the visual axis receiving the desired optical effect.2 Specialty contact lenses allow different features of customization to overcome the challenges of these typical soft multifocal pitfalls.3 The following cases illustrate several different types of designs and troubleshooting methods.
 |
|
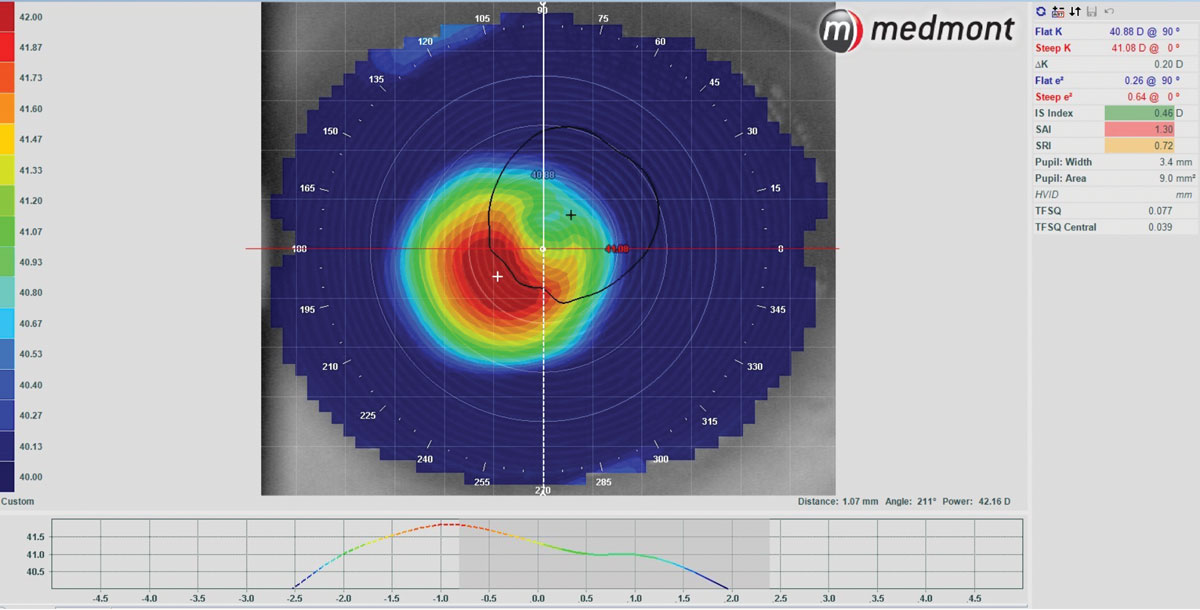
Fig. 1. Here, an axial map was used with a custom scale to show approximately 1.07mm of decentration along the 211° angle, inferior-temporal OD. The scale was set to be 1D steeper than flat K to 1D flatter than flat K. Click image to enlarge. |
Case One
A 55-year-old woman was looking for contacts to wear for the first time to improve her vision while playing tennis. She typically wore glasses while on the court but found those to be annoying and wanted to try contact lenses. She was offered multifocal correction but initially opted for distance-only vision. However, when she looked down at her watch and phone, it wasn’t clear like it was when she wore her glasses, and she found it to be “quite annoying,” so she wanted to try multifocals. Her soft lenses were then refit into a multifocal and she was given another two-week trial.
She returned and reported that the distance wasn’t as good, making it harder to see the ball. It was then discussed if she would be interested in becoming a full-time contact lens wearer to try a gas-permeable (GP) multifocal, and she agreed to give it a try. Lenses were designed empirically with consideration of her K values, HVID, spectacle Rx, pupil size and eye dominance. Pupils and eye dominance can be particularly important when considering the zone size for the multifocal optics. A center-distance aspheric was designed for her to allow clearest vision at distance. The central-distance zone was about 3.9mm in diameter, just smaller than the 5mm pupil diameter in regular mesopic lighting conditions with an aspheric add zone surrounding.
 |
|
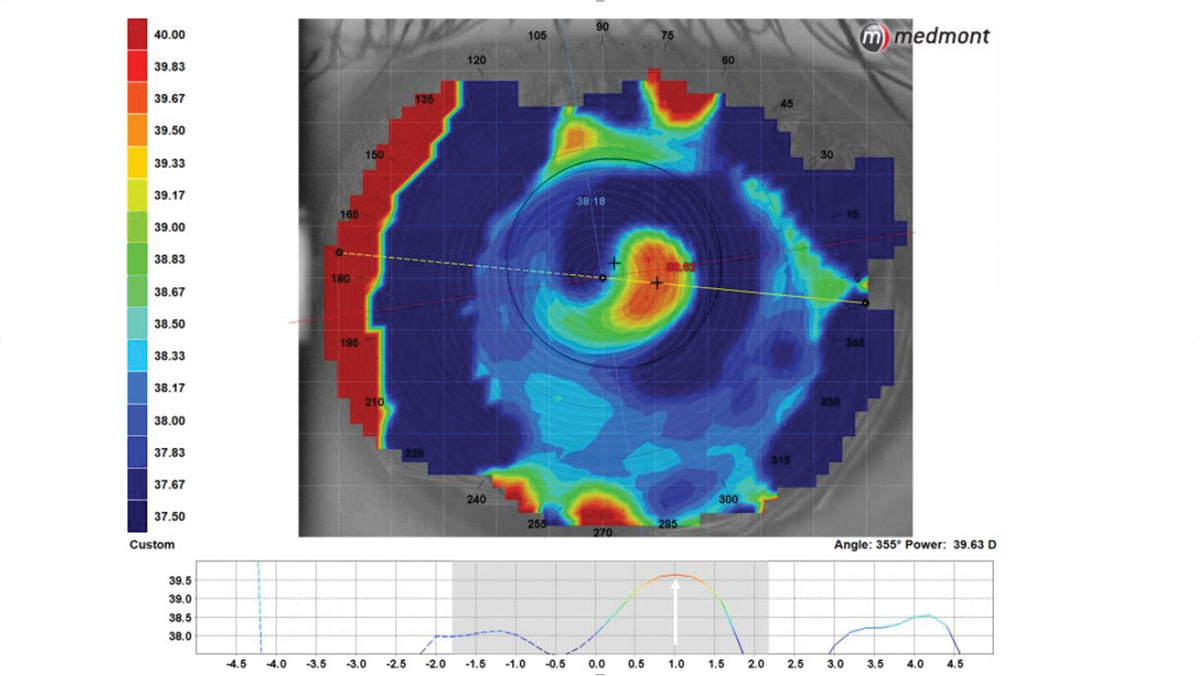
Fig. 2. The condensed topography scale shows a 2.5mm center-near scleral multifocal optical zone that is 1mm decentered temporally on the eye . Click image to enlarge. |
She appreciated improved distance vision compared to the soft lenses while being able to see her watch and check her phone. She then asked, “Can the up-close be any clearer?” In order to troubleshoot this, eye dominance was confirmed using the sensory method by taking a +1.50 trial lens and blurring each fully corrected eye to determine which was the dominant eye.
Another patient, a 63-year-old male stable keratoconus in OU, presented for a contact lens refit. He had been seen a few years prior but discontinued contact lens wear from his GPs because he was frustrated, as he was unable to see at near. Topography showed his keratoconus condition to be mild with marginal ectasia, with the steepest part of his corneas only reaching around 45D but showing an inferiorly decentered corneal apex. This indicated he may not have needed an aspheric keratoconic GP design and could potentially find success with a GP multifocal.
With 3D of corneal astigmatism in each eye, initial lenses were selected based on average or mean K and lenses were ordered empirically. The fluorescein showed a touch with flush pattern with the lenses on dispense. He was able to maintain his BCVA of 20/25 OU at distance and was ecstatic with his improved near vision. This is a reminder that our keratoconic and irregular cornea patients are also seeking presbyopic correction later in life and should ask evaluate clinical data to determine if they are reasonable candidates for multifocals.5
GP lenses offer customization and great corneal astigmatic correction. One of their primary uses is for patients with corneal irregularity, especially keratoconus. This is a reminder that our keratoconic and irregular cornea patients are also seeking presbyopic correction later in life. Therefore, we should evaluate their clinical data to determine if they are reasonable candidates for multifocals. This introduces another issue as keratoconus often causes inferior steepening of the cornea. As a result, GPs will often decenter inferiorly over the apex of the cone when placed on eye. This again introduces the problem of the optics becoming displaced on eye.
Scleral lenses have become extremely popular options for correcting these patients’ vision in the past few years. They are excellent for correction of corneal astigmatism and are comfortable lens options for patients, including those with dry eye like many presbyopes. However, like GPs, scleral lenses are fit to be stable on eye with little to no movement and can decenter, often inferior-temporally. As such, many scleral multifocals utilize an aspheric center-near optical system.5,6
 |
|
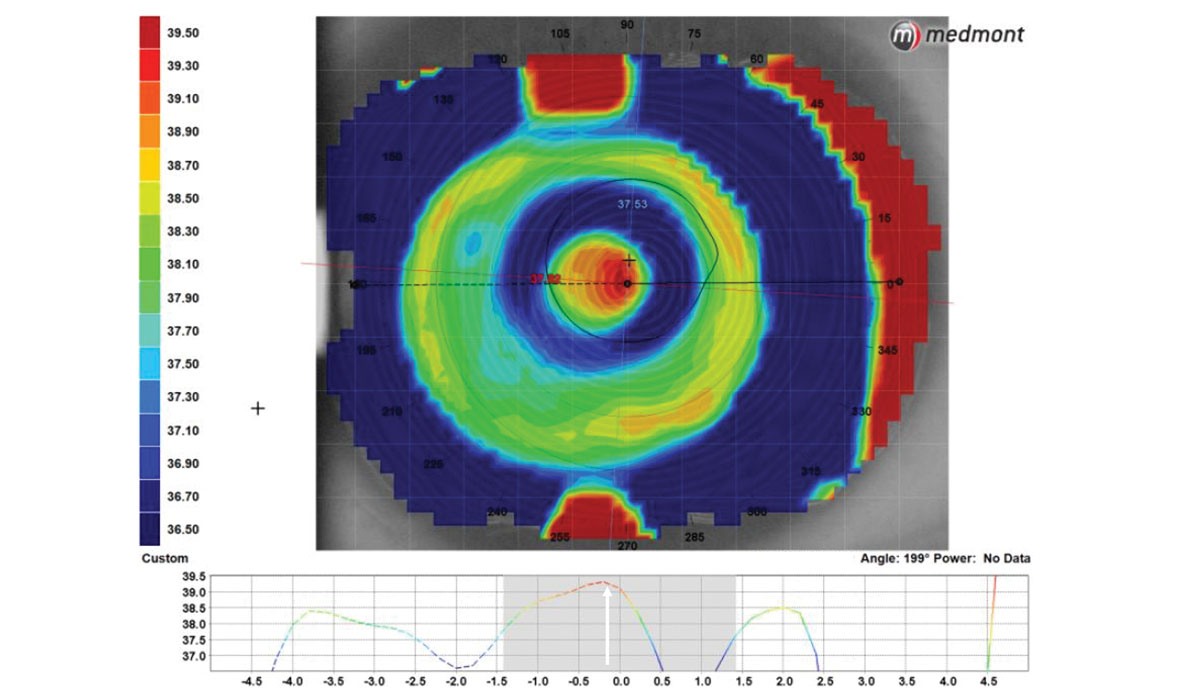
Fig. 3. After adjusting for the decentration measured on the previous lens, labs can realign the optic by decentering the multifocal to better align with the visual axis. Click image to enlarge. |
Case Three
A 57-year-old male with keratoconus returned for his yearly contact lens exam. He was successfully fit with scleral lenses but was becoming frustrated with needing readers. When the option of a multifocal was explained, he was interested in trying it. The problem was that his sclerals showed typical inferior-temporal decentration (Figure 1).
Topography has been shown to be an effective tool in visualizing multifocal optic location with a lens on eye. The best way to visualize this is by compressing the scale of the map to focus on the values in the center of the lens, where the multifocal is located (Figure 2). Labs are now able to purposely decenter the multifocal optic zone to reposition it to the center of the visual axis (Figure 3). This decentration can be measured topographically or through specially marked diagnostic fitting sets.
Case Four
A woman with high myopia presented for contact lens fitting several years ago, seeking better vision than her glasses where she was correctable to 20/40 in each eye at distance. She was fit with GP lenses that gave her 20/20 vision for the first time in years. She was stable for several years when she began to notice blur at near with her contacts.
The patient was initially shown new trials with a monovision setup, decreasing the power in the nondominant eye by 1.50D to allow some suppression at distance. After a three-week trial period, she returned unhappy with the vision and unable to adapt to the optics, feeling “thrown off” by them and finding particular difficulty at night. Her lid anatomy was ideal for a translating GP multifocal design since her lower lid rested at the level of the lower limbus.7 The Expert Progressive design uses progressive optics while others offer segmented bifocals or trifocals. These designs often feature seg heights to customize where the different optical zones begin and end along with base-down prism and/or truncation techniques to stabilize the lens on the lower lid and aid with translation.8
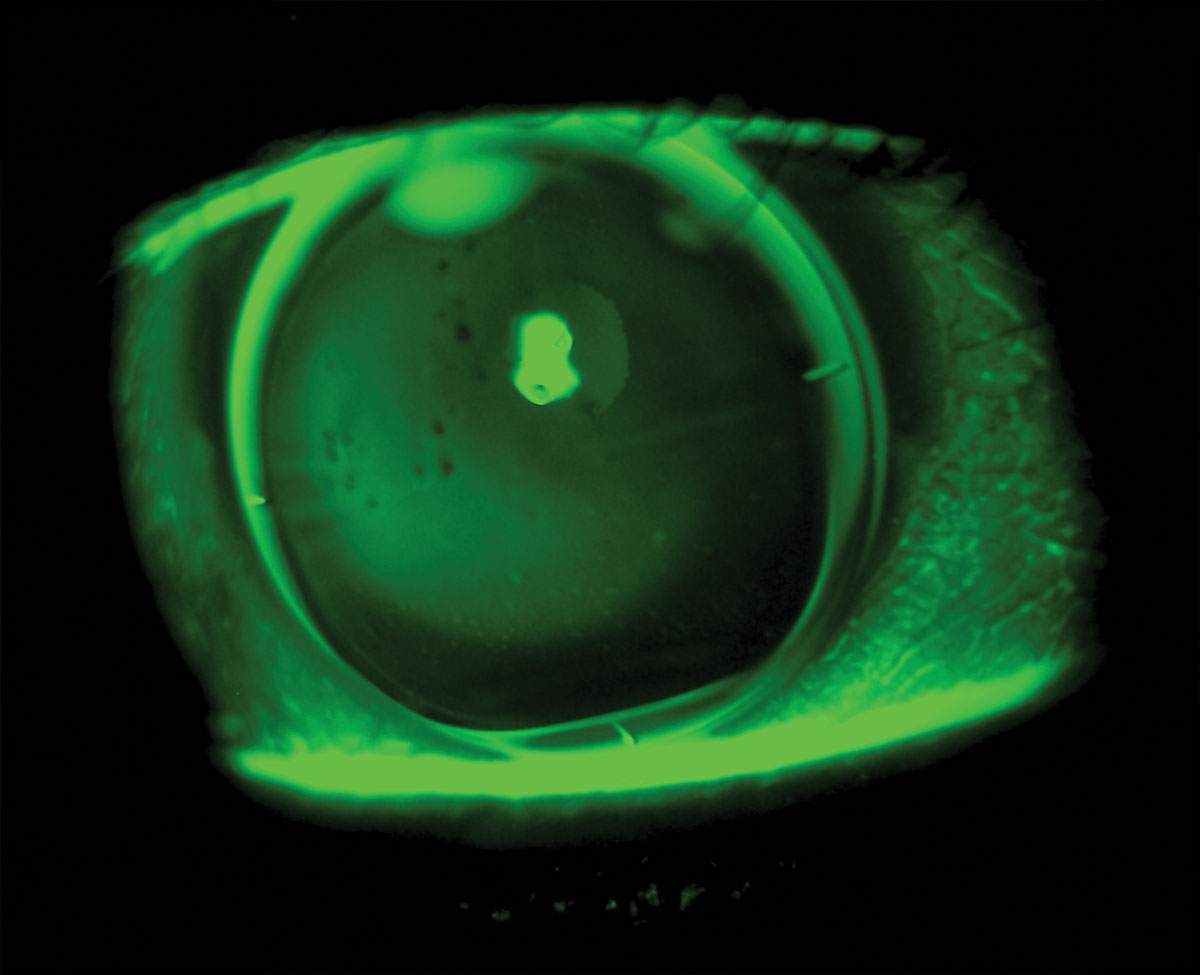
The patient reported crisp 20/20 VA at distance with the first pair of trials. While her near vision was better, she still wasn’t overly impressed yet. Slit lamp examination showed the seg lines at three and nine were a little low when they are typically desired to be inside the bottom portion of the pupil (Figure 4). After bringing the seg height up 0.2mm in each eye, she found the near vision much improved.
Another key feature to success in this case was the translation of the lens on eye. The lens should be able to move up to the superior edge of the cornea when the patient looks down; this ensures the patient can access the intermediate and near zones of the lens. The amount of prism can be adjusted along with the overall fit pattern to allow for the desired translation. Increasing the amount of prism can help if the lens is superiorly decentered, rotates out of position or slips below the lower lid on down gaze.
The amount of truncation can also be adjusted. Minus power lenses have greater edge thicknesses so should not be overly truncated to avoid thinning the inferior edge. Therefore, minus lenses benefit from more prism stabilization while plus lenses, with greater center thickness, can stabilize more from truncation.4
 |
|
Fig. 4. Translating progressive GP lens. Note the seg lines below the inferior pupil margin indicating the seg height will likely need to be raised for improved near vision.Click image to enlarge. |
Case Five
A 65-year-old woman had a long-established history of GP lens wear, fit over 15 years ago with monovision. She was asked how she feels about her vision while wearing contacts, and she explained that she felt like the vision up-close was okay, not great, with a lot of glare at night and asked if there is there anything that can be done about the glare. There was no sign of any ocular pathology and cataracts only showed trace nuclear sclerotic. She was told that she was a good candidate for multifocals since she was already a GP lens wearer, and she was fit with a translating trifocal design. This was selected because she had good lower lid anatomy to support a translating lens, and it would still provide an intermediate zone of correction, something lacking in her monovision lenses.4,7 The greatest advantage, though, would be a distance zone at the top of the lens to allow sharp distance vision in both eyes, undisturbed by near or multifocal optics. Lenses were ordered empirically where base curve selection depends on the amount of corneal cylinder and a default seg height of the trifocal was selected as 4.7/4mm with a 1.5D base-down prism ballast.
On dispense, the lenses showed good movement and positioning on the lower lid, but the central fluorescein pattern looked a bit flat, showing some mild central bearing in each eye. Her VA was 20/20 at distance and near in each eye, but she reported her vision still seems off. She was recommended to try the lenses for two weeks to aid with adaptation; however, at follow-up, she reported she was really struggling with the distance vision despite how good the near looked.
On closer examination, it was observed that the lenses showed lid grab after blinking that would pull the lens up, bringing the near zone over the pupil when trying to view at distance. This was determined to be because of the flat-fitting pattern so the lenses were steepened by 0.75D and the seg height was dropped by 0.2mm, reducing it to 4.5/3.8mm (Figure 5). After trialing the new lenses, the patient was thrilled and reported better near vision than she ever had in her contacts and elimination of the glare she had at distance.
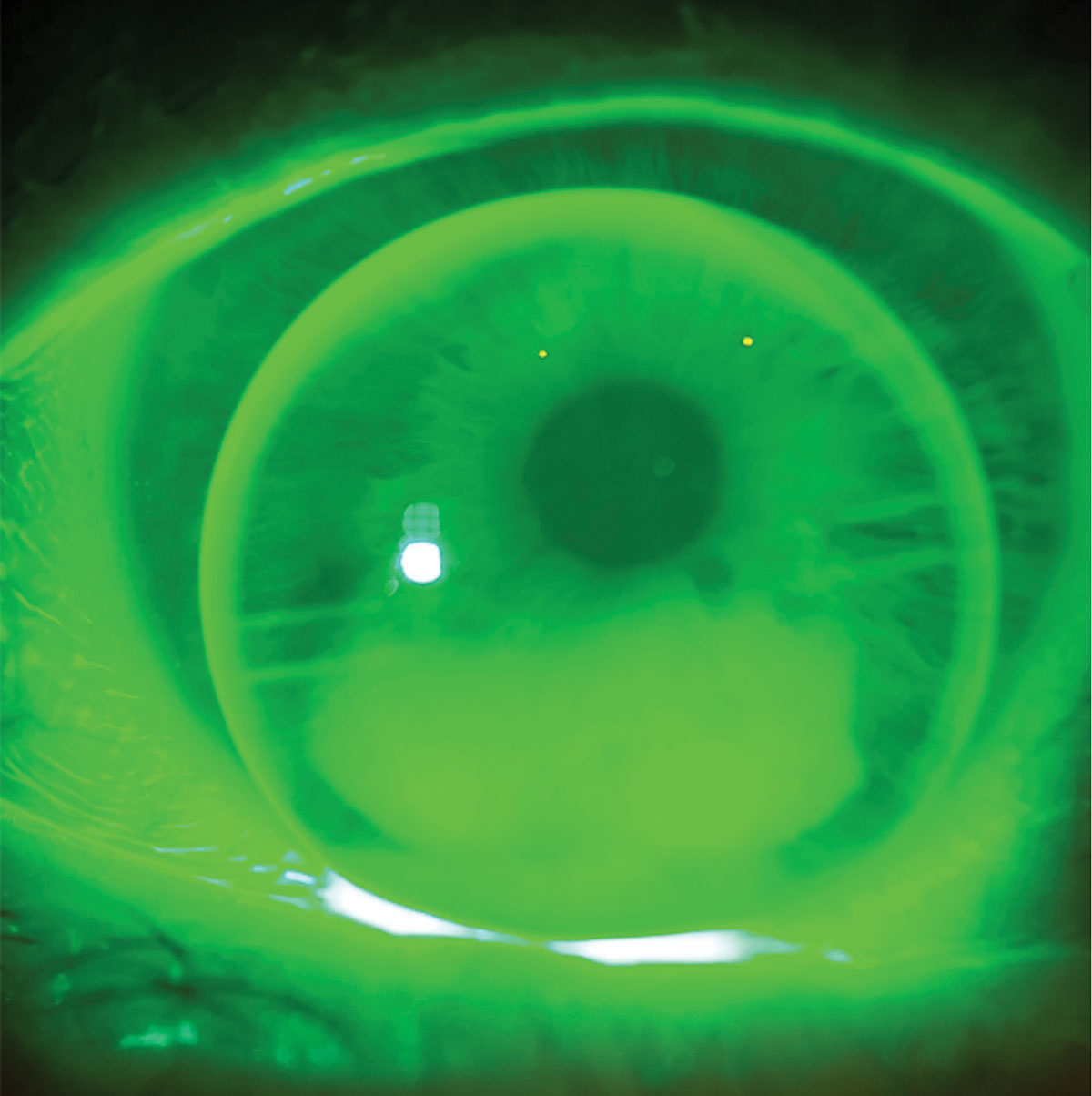 |
Fig. 5. Seg height was brought down 0.2mm to improve the patient’s vision at distance while still allowing easy access to the intermediate and near zones in the translating trifocal optic. Click image to enlarge. |
Takeaways
While scleral lenses come with their own unique array of potential complications, mitigating them typically comes down to three goals: maximizing corneal oxygenation, ensuring proper lens fit and emphasizing proper lens compliance. Implementing these fundamental traits when fitting scleral lenses can help one avoid potential complications or drive appropriate management should they arise.
Dr. Gidosh graduated from the Pennsylvania College of Optometry and completed a Cornea and Contact Lens residency at the Michigan College of Optometry at Ferris State. He is a Fellow of the American Academy of Optometry and has served as a clinical investigator for studies involving hybrid, scleral, multifocal and orthokeratology lenses. He is a consultant for Acculens and Bausch + Lomb.
1. Gurnani B, Kaur K. Commentary: leap forward in presbyopia management – correcting beyond spectacles. Ind J Ophthalmol. 2023;71:1843-4. 2. Fernandes PRB, Neves HIF, Lopes-Ferreira DP, et al. Adaptation to multifocal and monovision contact lens correction. Optom Vis Sci. 2013;90(3):228-35. 3. Bennett ES. Options Abound: A 2015 REPORT on Custom Contact Lenses. Review of Cornea & Contact Lenses. September 2015:22-25. 4. Davis RL, Schwartz M. Seeing multifocal optics more clearly. Review of Cornea & Contact Lenses. 2021;16-20. 5. Chang CY, Denaeyer GW. Specialty Contact Lenses: Treat Your Keratoconus Patients Right. Review of Cornea & Contact Lenses. 2017;14-17. 6. Sicks L, Nguyen TA. Managing Presbyopia With Sclerals. Review of Cornea & Contact Lenses. 2020; 38-39. 7. Turpin S, Skorin L. How Lid Malposition Can Compromise Contact Lens Wear. Review of Cornea & Contact Lenses, [s. l.], p. 24–28, 2016. 8. Ensley R, Miller H. Don’t Forget to Check the Lids. Review of Cornea & Contact Lenses. 2016;36-7. |


