Presbyopia can seemingly happen overnight. One day, your 40-something patient can read the text on their phone screen, and the next, their arm is suddenly not long enough. In reality, presbyopia is a process that progresses as we move through adulthood. Contact lens wearers may experience subtle, early presbyopic symptoms before they reach their mid-40s, including eyestrain, fatigue with near work and headaches. Initiating presbyopic contact lens correction efforts earlier on can ease adaptation and prevent unnecessary contact lens dropout.
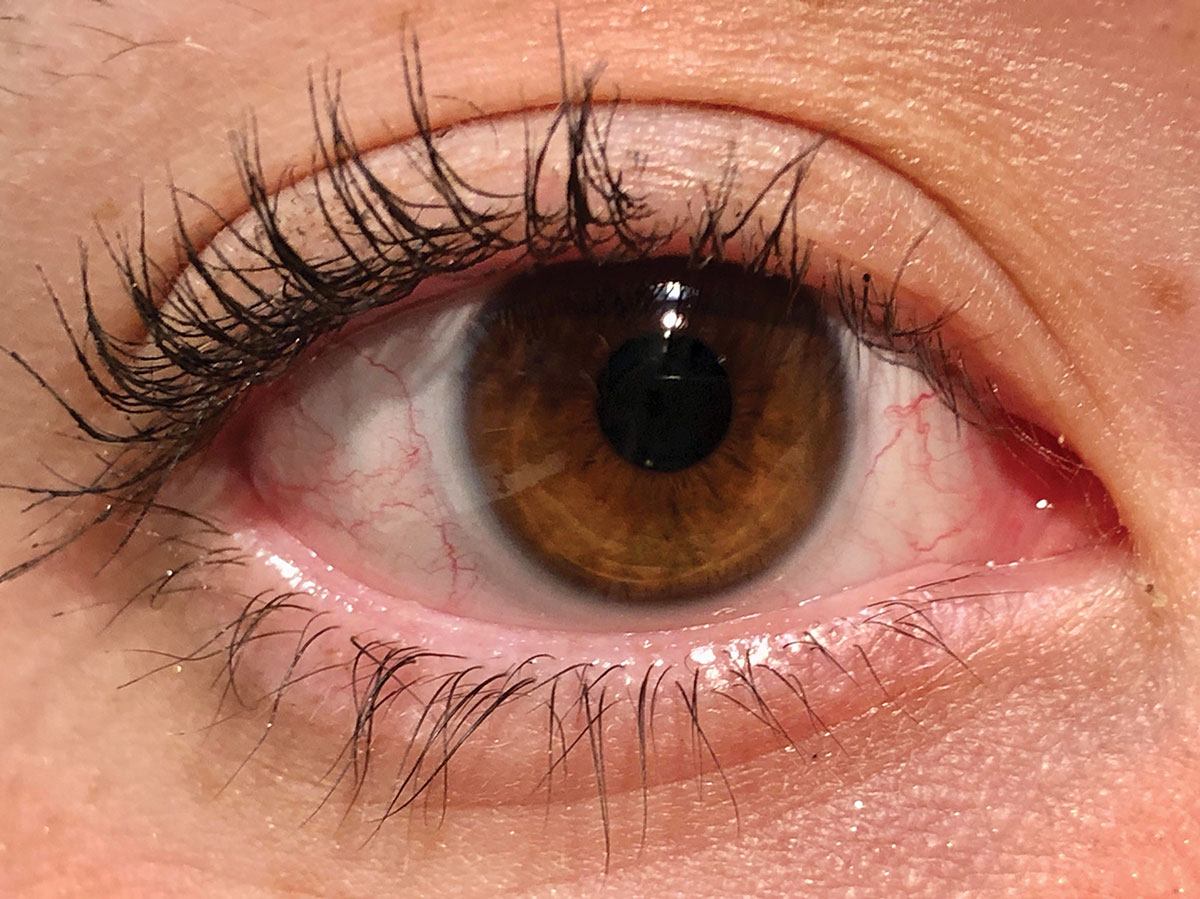 |
| Recommend multifocal contact lenses early for easier adaptation. Click image to enlarge. |
Initiate Management
The discussion about presbyopic contact lens options typically starts when patients complain of near blur. It is important to remember, however, that near blur is not the only symptom associated with presbyopia, and it may not be the first symptom to present. Blurry near vision may not occur for most patients until their mid-40s, but symptoms associated with declining accommodative amplitude can begin as early as age 30. Be proactive and address presbyopic symptoms before complete near blur occurs.
Accommodative amplitude remains relatively stable throughout childhood and into our mid-20s, when it starts to rapidly decline.1 Between the ages of 30 and 40, accommodative amplitude can decrease by up to 3.00D.1 This means that we lose almost half of our accommodative amplitude before even reaching an age many associate with presbyopia onset.
While patients approaching presbyopia may be able to visualize clear images, they may not be able to do so comfortably, especially after a long day of near or computer work. Symptoms associated with accommodative fatigue and insufficiency can contribute to symptoms of asthenopia and discomfort.2 Myopic patients who wear glasses may be able to alleviate some of this accommodative fatigue by removing their glasses when doing near work. When corrected with contact lenses, however, these myopes cannot escape their waning accommodation and may mistakenly assume discomfort associated with accommodative fatigue is related to their contact lenses.
Recognize that presbyopic accommodative decline happens before a patient experiences sustained near blur. You can uncover other signs by asking those in their 30s and early 40s about specific symptoms of discomfort resulting from near and computer work. “Discomfort” can describe symptoms that stem from different etiologies. While symptoms of discomfort such as dryness, itchiness and burning can be caused by an ocular surface or fit issue, symptoms such as eyestrain, headaches and blurry/variable vision are likely associated with discomfort related to presbyopic accommodative fatigue and insufficiency.2,3
Perform Refraction
The first step to ensuring your emerging presbyope is optimally corrected in their contact lenses is to confirm that their lenses reflect your refraction, which you’ve confirmed is accurate. To do this, focus on accurate myopic and full astigmatic correction.
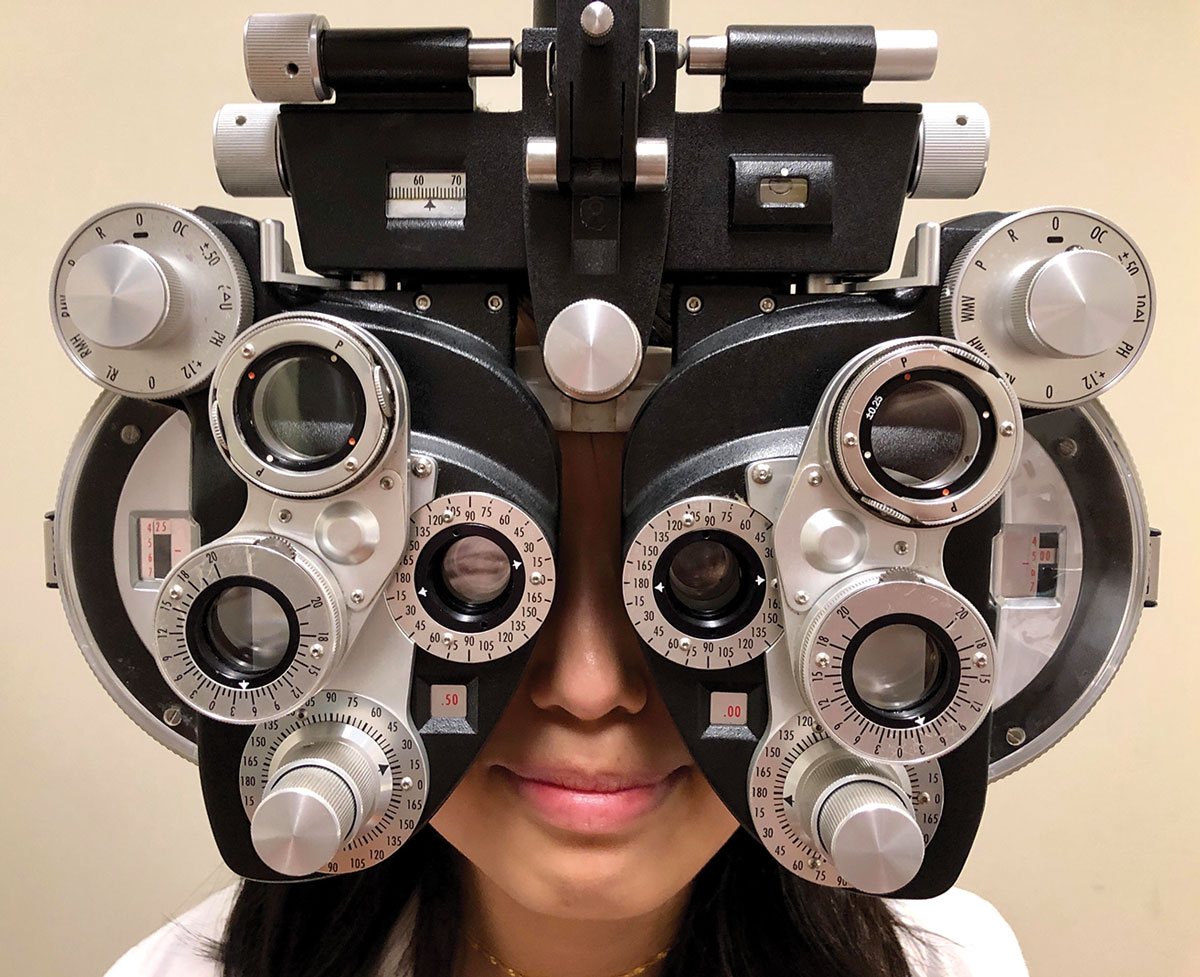 |
| Contact lens parameters must line up with your refraction for optimal correction. Click image to enlarge. |
As our accommodative amplitude is robust from childhood until early adulthood, myopic patients who prefer “smaller, darker” distance vision (i.e., overcorrected myopia) can overcome the increased accommodative demand that “over-minusing” causes. As these patients enter their 30s, that extra accommodative demand, however, can exacerbate symptoms related to their natural decline in accommodation.
Make sure the manifest refraction doesn’t include any myopic power that these patients do not actually need to achieve acceptable distance vision. Also ensure you have appropriately vertexed the manifest refection on which you are basing your contact lens power. Accounting and correcting for even small amounts (0.25D to 0.50D) of myopic overcorrection can alleviate discomfort associated with near work.
With glasses, we almost always prescribe exactly what we find in our phoropter. Rarely do we round up to the major meridian or totally disregard cylinder power. Unfortunately, with contact lenses, we commonly ignore small amounts of astigmatism if the patient is “fine” in a spherical lens. About half of all contact lens wearers have at least 0.75D of astigmatism, but we only prescribe toric contact lenses for about 25%.4
Uncorrected astigmatism can contribute to overall and visual discomfort.3 Studies have shown that, even in cases of low astigmatism, visual acuity and performance in low light/glare conditions improve with toric contact lens correction compared with spherical correction.5,6 Patients tend to prefer having their astigmatism maximally corrected when wearing contact lenses, and full toric correction may alleviate symptoms associated with eyestrain and discomfort at near.7
Failing to correct astigmatism to the best of your ability could cause visual strain and result in a patient removing their contact lenses and relying on their spectacles that fully correct for astigmatism. Before even initiating presbyopic contact lens correction, ensure the patient’s distance prescription, including spherical and astigmatic elements, is optimally corrected with their contact lenses. This alone may eliminate symptoms associated with declining accommodation for the next year or so or, at the very least, will optimally position you to choose how to proceed with presbyopic contact lens correction.
Introduce Multifocals
When a patient consistently complains of early presbyopic symptoms, including difficulty concentrating, tiredness while reading and consistent headaches and eyestrain, it’s time to introduce a multifocal contact lens. Especially earlier on, a multifocal contact lens is the best option to alleviate symptoms of presbyopia while maintaining binocular vision at all distances.
Multifocal contact lenses are sometimes associated with a bad reputation and are consequently woefully under-prescribed in presbyopic contact lens wearers.8 The simultaneous, aspheric optics used in today’s modern multifocals sometimes compromise near, intermediate and/or distance vision. Patients may also experience glare in low light situations when pupil size increases. Prescribers assume these are deal breakers and tend to shy away from considering multifocals, suggesting an over-the counter reading spectacle or turning to monovision contact lens correction.
Contact lens wearers, however, typically prefer multifocal contact lens correction to other presbyopic contact lens options when given the chance to try them. Compared with monovision, multifocal contact lenses consistently provide superior overall visual experiences and have similar acuities at all distances in high contrast conditions and superior stereoacuity.9-11 Even though objective low contrast visual acuity is sometimes better with monovision, patients usually lean toward the vision and overall wearing experience multifocal contact lenses offer.9,11 When your patient begins having presbyopic symptoms, it’s worth taking a look at multifocals.
Set Expectations
Before beginning the multifocal fitting process, make sure your patient is educated, optimistic and confident so that compliance isn’t an issue down the road. Successful multifocal contact lens fittings are achieved during patient education. If you take a few extra minutes during the initial fitting to explain why you are introducing a new contact lens, what the patient can expect during the adaptation period and how they will benefit from the change, your success rate will dramatically increase. It’s also worth mentioning the consequences of improper wear and care practices in this stage.
Especially in early and emerging presbyopes, explaining presbyopia can be difficult. This age group may not know what presbyopia is or that they will inevitably experience it. Be concise when introducing the condition to patients who may have no prior knowledge or understanding of it and explaining that as we get older, our eyes are unable to focus up close as effectively because we spend so much of our time looking at a screen and reading.
It also helps to use clear language when describing how vision correction lenses work, especially as the optics of these lenses are complex. Combining your description of the lenses with what patients can expect may be an effective way to do this. Note that because these lenses focus images from multiple distances on your eye at the same time with your brain deciding what image to pay attention to based on what you are looking at, it may take a few days to figure out how to find the sweet spot in your vision.
Patients benefit from reassurance that any preliminary issues they may experience are normal and will gradually subside with your help or with time. Displaying confidence in the lenses and communicating openly about them before a patient experiences multifocal lenses for what could be the first time will make them more willing to work through any frustrations they have until they reach a more successful outcome.
 |
| Use different resources to educate your patients and make sure you’re always on the same page. Click image to enlarge. |
Optimize the Fit
In recent years, the parameters and modalities of soft multifocal contact lenses have expanded significantly. An increase in daily disposable options and myopic and hyperopic spherical powers and the emergence of soft toric multifocals means that there are solutions available for the majority of presbyopic patients. When possible, start with a daily disposable. The frequent replacement schedule associated with these lenses allows for the most consistent and comfortable experience. When a daily disposable is not an option, find another lens with an appropriate replacement schedule, and prescribe a solution that works best with that lens material.
Regardless of what lens you choose, make sure to follow the manufacturer’s fitting guide for initial lens selection and troubleshooting. While suggestions included in these guides often seem like common sense, some recommended adjustments and starting points that have proven to be successful through extensive research may not be intuitive to you. Save yourself chair time and frustration by implementing these guides in your practice. Most fitting guides suggest initial lens powers based on add power. If your emerging presbyope does not require an add yet but is experiencing symptoms of accommodative fatigue, select a lens with the minimum add power the manufacturer advises.
Assessing vision with a multifocal contact lens is different than taking entering acuities at the beginning of your exam, especially on the first day. It is common for vision to improve with adaptation, so don’t be discouraged if your patient can’t see their best-corrected line right after you insert the multifocal. Make sure they know what to expect too; their first impression is important. Assess what they can see with the new lenses, and don’t make what they cannot see the focus of the conversation. Remember, you want the patient to leave your office optimistic about the wearing experience they are about to embark on.
Evaluate vision binocularly and with normal room illumination. At distance, start with large, isolated lines, and go down in size as long as the patient is able to easily read each visual target. If you have good refractive data and began with the lenses suggested by the fitting guide, you should not need to make many, if any, changes on the initial fitting day.
The impressive moment with a multifocal comes when a presbyope is able to read small print without reading aids. You will not get this opportunity with an emerging presbyope who can still read small print clearly. Because you are introducing a new optical system, these patients may actually report that their vision feels different at all distances initially. In these instances, remind the patient that the purpose of the lenses is to alleviate symptoms of focusing fatigue. After the patient adapts to the lenses and wears them for a full day of work, reading or computer use, they will be able to fully appreciate them.
Once the patient is ready to leave your office on the first day, make sure they understand the importance of communicating any negative experiences they have after the initial adaption period, as these can be addressed at follow up visits. This is when you can lean on the corresponding fitting guide for solutions to near and/or distance vision issues. If comfort isn’t desirable and/or satisfaction cannot be reached after one or two lens swaps, consider switching brands.
Managing early presbyopic symptoms by keeping patients informed and prescribing multifocal contact lenses will prevent premature, unnecessary contact lens dropout. Transitioning presbyopes when the discrepancy between distance and near powers is the least problematic also helps ensure your patient experiences minimal negative symptoms and their visual system more easily adapts to future changes as you introduce greater add powers. Multifocal contact lenses are a great solution for patients who are entering a stage in their life when things are starting to become blurrier and they need an option to correct this unwanted change.
1. Anderson HA, Hentz G, Glasser A, et al. Minus lens-stimulated accommodative amplitude decreases sigmoidally with age: a study of objectively measured accommodative amplitudes from age 3. Invest Ophthalmol Vis Sci. 2008;49:2919-26. 2. Reindel W, Zhang L, Chinn J, et al. Evaluation of binocular function among pre- and early-presbyopes with asthenopia. Clin Optom (Auckl). 2018;10:1-8. 3. Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optom Vis Sci. 2003;80(11):732-9. 4. Morgan PB, Efron N, Woods CA. An international survey of toric contact lens prescribing. Eye Contact Lens. 2013;39(2):132-7. 5. Black AA, Wood JM, Colorado LH, et al. The impact of uncorrected astigmatism on night driving performance. Ophthalmic Physiol Opt. 2019;39(5):350-7. 6. Richdale K, Berntsen DA, Mack CJ, et al. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969-75. 7. Cox SM, Berntsen DA, Bickle KM, et al. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers. Eye Contact Lens. 2018;44 Suppl 1:S296-9. 8. Morgan PB, Efron N, Woods CA. An international survey of contact lens prescribing for presbyopia. Clin Exp Optom. 2011;94(1):87-92. 9. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci. 2006;83(5):266-73. 10. Situ P, Du Toit R, Fonn D, et al. Successful monovision contact lens wearers refitted with bifocal contact lenses. Eye Contact Lens. 2003;29(3):181-4. 11. Woods J, Woods CA, Fonn D. Early symptomatic presbyopes—what correction modality works best? Eye Contact Lens. 2009;35(5):221-6. |


