The loss of accommodation can be frustrating, especially for today’s busy and somewhat demanding presbyope. Digital devices combined with active lifestyles can simultaneously increase demands on near vision while also making wearing spectacles seem burdensome. Meeting the needs of our presbyopic patients, especially those with astigmatism, may sound challenging; however, there is a growing number of contact lens options at our fingertips.
According to the 2018 US Census Bureau, approximately 119 million people, or nearly 40% of the population are between the age of 40 and 69.1 Patients in this age range may have the inability to keep up with the demands on their accommodative system. One approach to provide functional near vision is with the use of contact lenses. In fact, many patients entering their presbyopic years currently wear contact lenses or have previous experience. For these patients, maintaining independence from the use of spectacles is often a priority. Additionally, at least one study suggests that spectacle wearing presbyopes would prefer contact lens use, if using them would achieve good vision and comfort.2
Despite the interest in contact lens wear, there are challenges for the presbyopic patient. Physiological changes to the tear film and ocular surface can contribute to contact lens discomfort, which is commonly cited as the main reason for dropout.3,4 However, poor vision is equally responsible for discontinuation among presbyopic patients.5 One perceived barrier to optimal vision in contact lenses is the presence of astigmatism.
Nearly 50% of contact lens patients have astigmatism of 0.75D or greater in at least one eye, yet only 30% of contact lenses are prescribed for astigmatism.6,7 This discrepancy is concerning, considering the decrease in acuity and symptoms of eyestrain that occurs from not correcting astigmatism as low as 0.75D.8,9 Accordingly, as astigmats become presbyopic, their astigmatism can play a crucial role in the ability to achieve the desired range of vision.
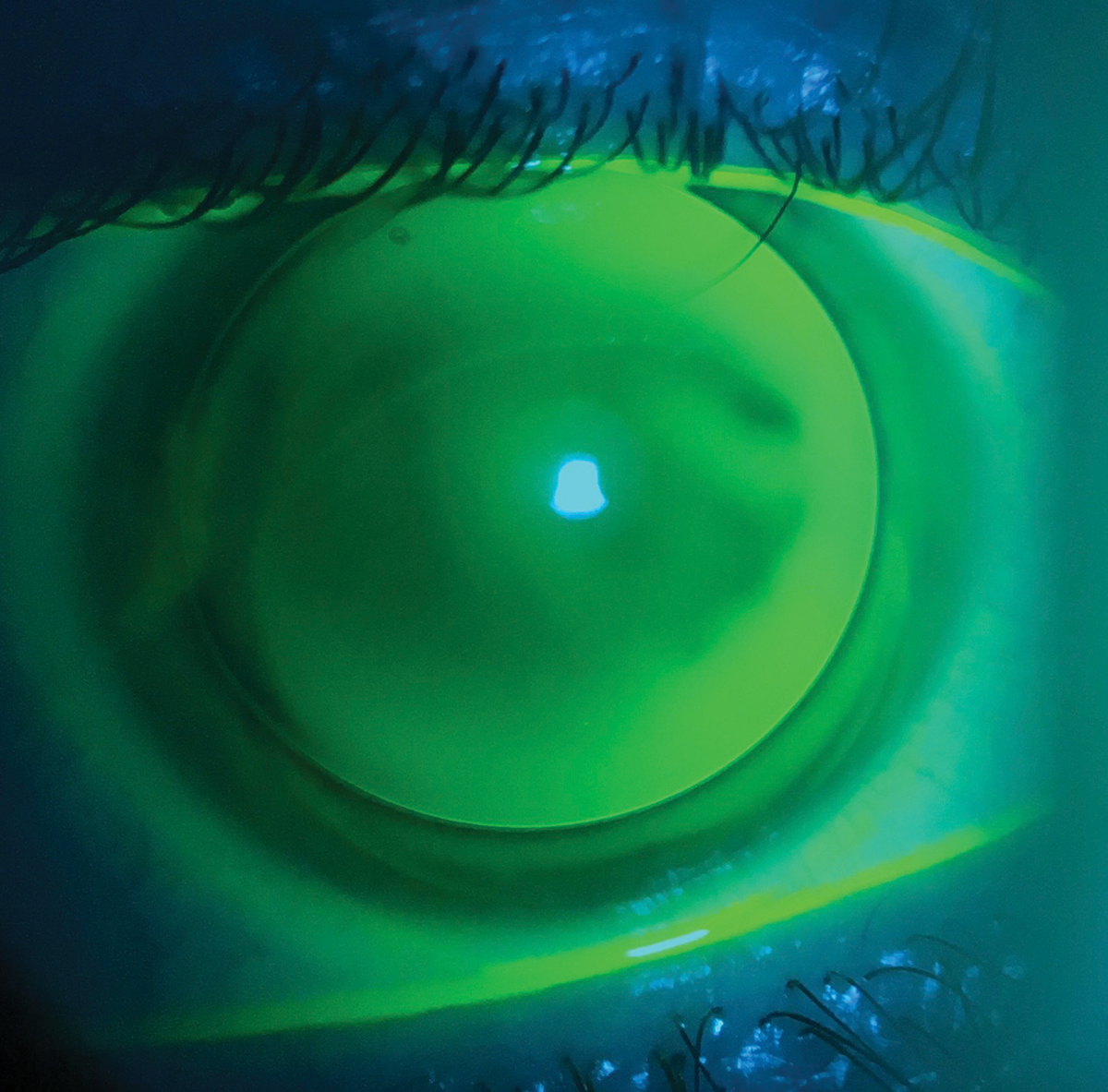 |
| Astigmatism up to 2.50D can be addressed easily in both soft toric and GP lens modalities. Click image to enlarge. |
Multiple Choices
Early contact lenses made from polymethyl methacrylate evolved to higher oxygen-permeable gas permeable (GP) lenses, which have remained a mainstay in the correction of astigmatism. GP lenses rest on the cornea and use the smooth refracting surface of the lens in combination with the post-lens tear layer to neutralize corneal astigmatism and provide crisp, stable optics. Before the rise of contemporary GP multifocals, presbyopic patients resorted to using reading glasses over their spherical, distance-only contact lenses or using monovision contact lenses.
Monovision. This option provides near vision by reducing minus power or adding plus power, typically over the non-dominant eye. Although effective, especially for early presbyopes, there are drawbacks to this setup. As the power difference between eyes increases, it can become more difficult to suppress blur, affecting binocularity and depth perception. Monovision has also been shown to reduce both contrast sensitivity and acuity.10 Despite these issues, monovision is still commonplace, with reduced chair time commonly cited as a reason for prescribing.11 However, when comparing monovision with multifocal contact lenses, studies consistently show patients preferring multifocals.12,13
Multifocal lenses. GP multifocals can be split into two categories, segmented and aspheric multifocals. Segmented or translating multifocals are similar to lined bifocals in that distance and near optics are separated into distinct segments. In primary gaze, the distance segment is in front of the pupil and visual axis, allowing for uninterrupted distance clarity. The reading segment is positioned at the pupil margin with the inferior lens edge resting on the lower eyelid. On down gaze, the reading segment translates upwards to move the near optics into the necessary position.
Aspheric multifocals have both distance and near zones, but the optics for both distance and near are presented in front of the pupil simultaneously. Near add power is created by a change in curvature on either the anterior or posterior curvature of the lens. These changes can create a smooth transition between working distances, but the brain must still adapt to the simultaneous vision optics.
Moving established GP wearers to multifocal designs is an easy transition, but having GP neophytes adapt to the initial comfort is a hurdle. If comfort is an obstacle, hybrid lenses provide GP optics with comfort similar to a soft lens. The smooth junction between the GP center and the soft skirt reduces lid interaction, while the skirt maintains centration and keeps the optics stable. Hybrid multifocals are available with aspheric optics in both center-near and center-distance designs. The center-near design has a set 3.0mm zone size with three different add powers, while the center-distance design has a flexible zone size with variable add powers up to 5.00D.
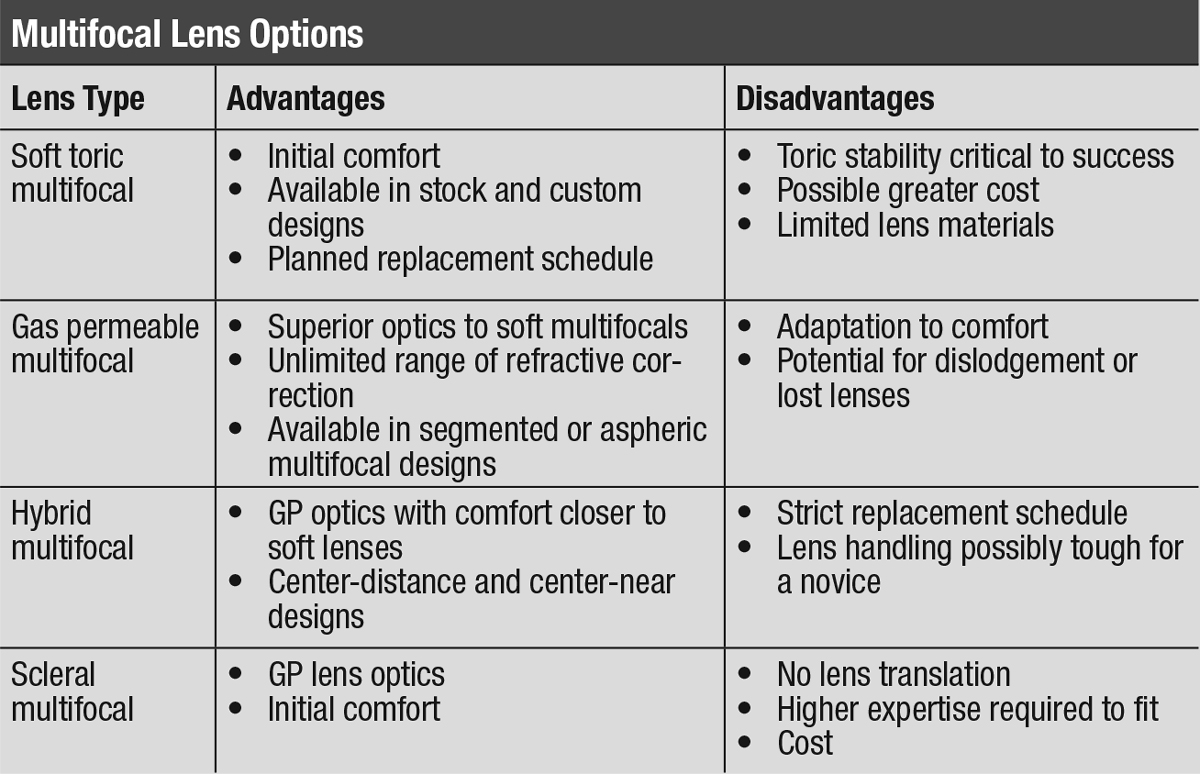 |
| Click table to enlarge. |
Although the popularity of GP multifocals has remained relatively stagnant, one growing market is scleral multifocals.14 Scleral lenses are large diameter GP lenses that vault the cornea and align with the sclera, providing stable optics and great comfort when fit properly. Their primary indication is for the irregular cornea, but their popularity has led to an increase in normal cornea applications, including multifocals, using smaller diameter (<15.5mm) scleral lenses.
Because there is no translation, many scleral lenses use center-near aspheric designs to provide near optics, though there are a few designs capable of center-distance optics. Additionally, at least one scleral multifocal design (Zenlens, Bausch + Lomb) is currently capable of decentering their optics to align with the true visual axis, rather than with the geometric center of the lens.
The optics of a GP lens is widely recognized as superior to their soft lens counterparts; however, soft toric lenses are significantly more popular. Contemporary soft toric lenses use superior lathing technology to create highly reproducible lenses in both disposable and custom modalities. Disposable soft toric lenses can correct up to 2.75D of astigmatism with around the clock axis in 10-degree increments. Although there has been one monthly replacement toric multifocal available for more than a decade (Proclear Toric Multifocal, Cooper Vision), prescribing soft toric multifocal lenses never gained much traction. The recent launch of Bausch + Lomb’s Ultra Multifocal for Astigmatism in June 2019 has brought soft toric multifocals back to the forefront.
If parameter availability is an issue, custom lens laboratories such as SpecialEyes or Art Optical are capable of customizing all parameters of the lens from the fit of the lens to the power of the astigmatism and the add power. Additionally, these custom lenses have the capability to adjust zone sizes and decenter the optics to help optimize vision.
Clinical PearlsCheck vision binocularly at both distance and near. Perform the over-refraction in free space with loose lenses. Use real-world examples to assess near vision (i.e., a computer screen, phone or tablet). Avoid making changes too early—adaptation time is key. Follow the fitting guide when available. Lab consultants are another great resource. Don’t be afraid to change designs if your first doesn’t work. |
Astigmatism Matters
Perhaps the most important factor in selecting a contact lens for a patient is their refractive error.
For astigmats, correcting the astigmatism is the first priority. The total refractive astigmatism of the eye combines the power from both the cornea and the crystalline lens. If the amount of refractive astigmatism is equal to the corneal astigmatism, the astigmatism is derived primarily from the cornea. Both soft and GP lenses can correct corneal astigmatism effectively.
If the refractive astigmatism is different than the amount of corneal astigmatism, the residual astigmatism originates internally, or from the lens. When lenticular astigmatism is 0.50D or greater, soft toric lenses or toric GP lenses are ideal. Toric GPs require lathing the astigmatic power into the front surface of the lens, which also requires rotational stability, much like a soft toric lens.
The majority of astigmatic patients have regular astigmatism, in which the meridional power is 90 degrees apart. Regular astigmatism can be further classified into with-the-rule (WTR), against-the-rule (ATR) or oblique astigmatism. WTR astigmatism happens when the vertical meridian is steeper, resulting in more power needed, while the flatter meridian is along the horizontal axis. When fitting GP lenses, they will tend to move along the steeper meridian, which makes a WTR cornea a more natural fit due to vertical blink forces. ATR corneal astigmatism will have a steeper horizontal meridian, which may result in lateral decentration of a corneal GP lens. If there is concern about the centration of a corneal GP lens, particularly with ATR or oblique corneal astigmatism, then soft toric lenses, hybrids or scleral lenses may be a better choice.
Also consider astigmatic power when selecting lenses. Astigmatism up to 2.50D can be fit easily in both soft toric and GP lens modalities. Correcting higher levels of astigmatism can be more complex. When choosing a soft toric, consider custom design lenses, given their ability to correct higher cylinder powers with a refined axis in one-degree increments. If the lens is not perfectly centered or rotationally stable, manipulate custom lenses to change base curve, diameter and prism-ballast amount to improve the lens fit.
A highly toric cornea can also cause decentration or poor alignment with a corneal GP lens. In these situations, adding back-surface toricity will improve the lens fit, but the lens may no longer have rotationally stable optics. Another option is scleral lenses, which vault the toric cornea while neutralizing astigmatism.
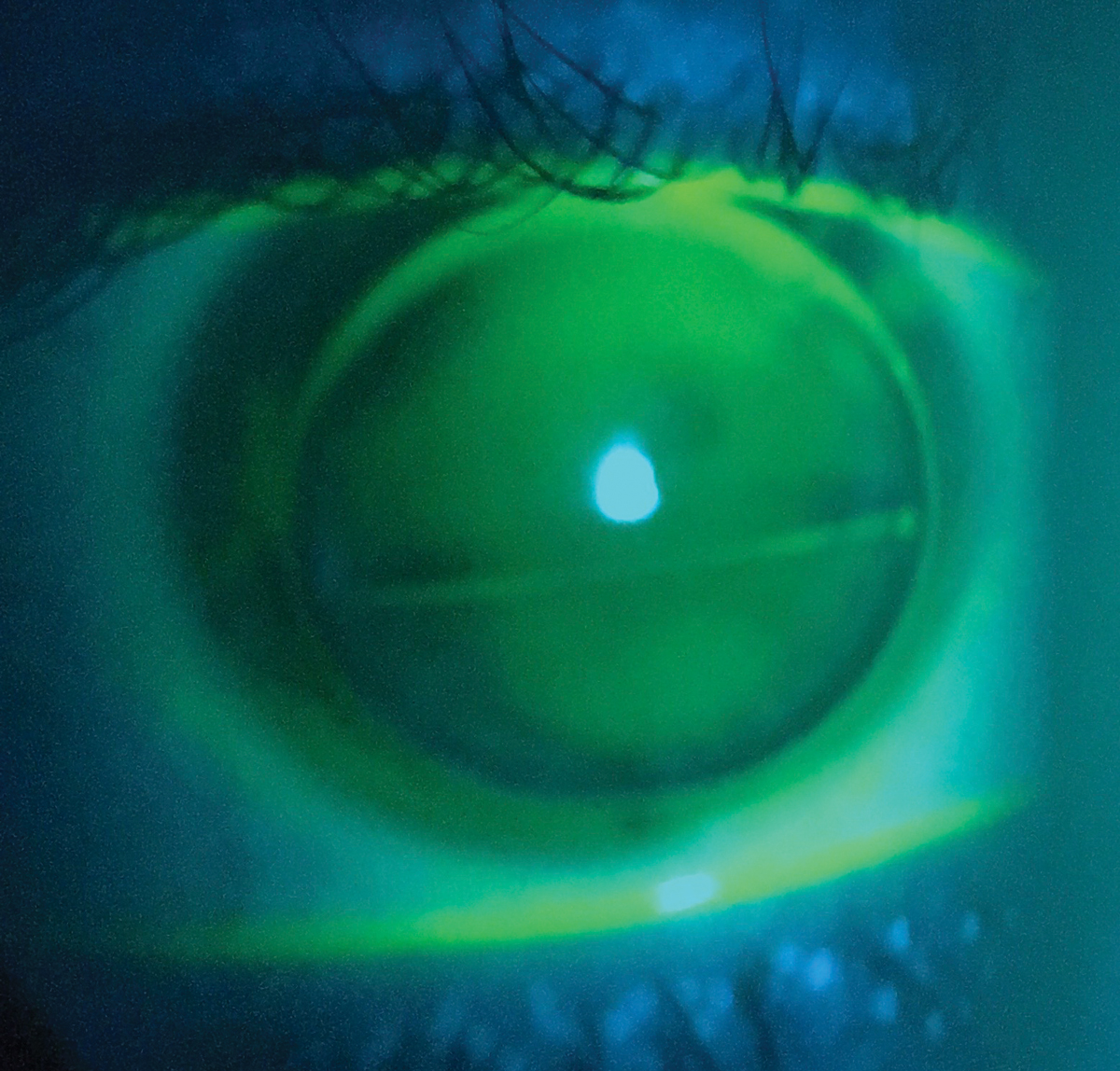 |
| Segmented or translating multifocals are similar to lined bifocals in that distance and near optics are separated into distinct segments. Click image to enlarge. |
An Add for the Near
With as many contact lens options as we have in our tool bag, incorporating the near power for each patient requires careful consideration of two main factors.
Previous experience. Satisfied contact lens wearers may not require a significant deviation from their current contact lenses. GP lens, hybrid and scleral lens wearers can typically have multifocal optics incorporated into their current designs without the need for refit. Soft toric lens wearers may require a discussion about changing lens materials or modality since there are fewer soft lens options than can incorporate both astigmatic and presbyopic correction simultaneously. While most patients are open to switching lens brand and material to accommodate their changing visual needs, there are some who are a bit more hesitant. For example, daily disposable toric lens wearers may be the most difficult, and these wearers may be relegated to readers or monovision if they aren’t willing or able to budge from the daily disposable route. Thorough education is key when determining the best options for your patients.
Visual demands and expectations. Learning the patient’s demands and expectations for their vision is critical to understand their motivation level and to recommend a contact lens. Patients with higher demands and a higher sensitivity to blur would likely do better with a GP lens modality due to the crisper optics and stability.
The desire for a full range of vision will make a multifocal lens of any modality a great choice. However, simultaneous vision designs may involve some manipulation of the range of vision. Knowing if the patient prefers a stronger distance or near range is useful in designing the lens parameters. Conversely, some patients cannot tolerate any compromise in their range of vision. These patients will not be good multifocal candidates, despite the available technology. Presenting the potential lens options, using patient-focused terminology and including them in the lens selection process can keep them involved in the fitting process. Thorough education and setting expectations is also critical to the patient’s contact lens success.
For contact lens neophytes, there is one additional factor to consider other than meeting vision demands. Initial adaptation to contact lens wear, including application and removal, can be a barrier to new wearers of any age. During preliminary testing, if a patient shows high sensitivity to approaching objects near the ocular surface, a soft lens might provide an easier adaptation to initial comfort. Patients with small apertures, deep set orbits or large fingers may also have more difficulty with application and removal and may do better with a smaller diameter corneal GP lens.
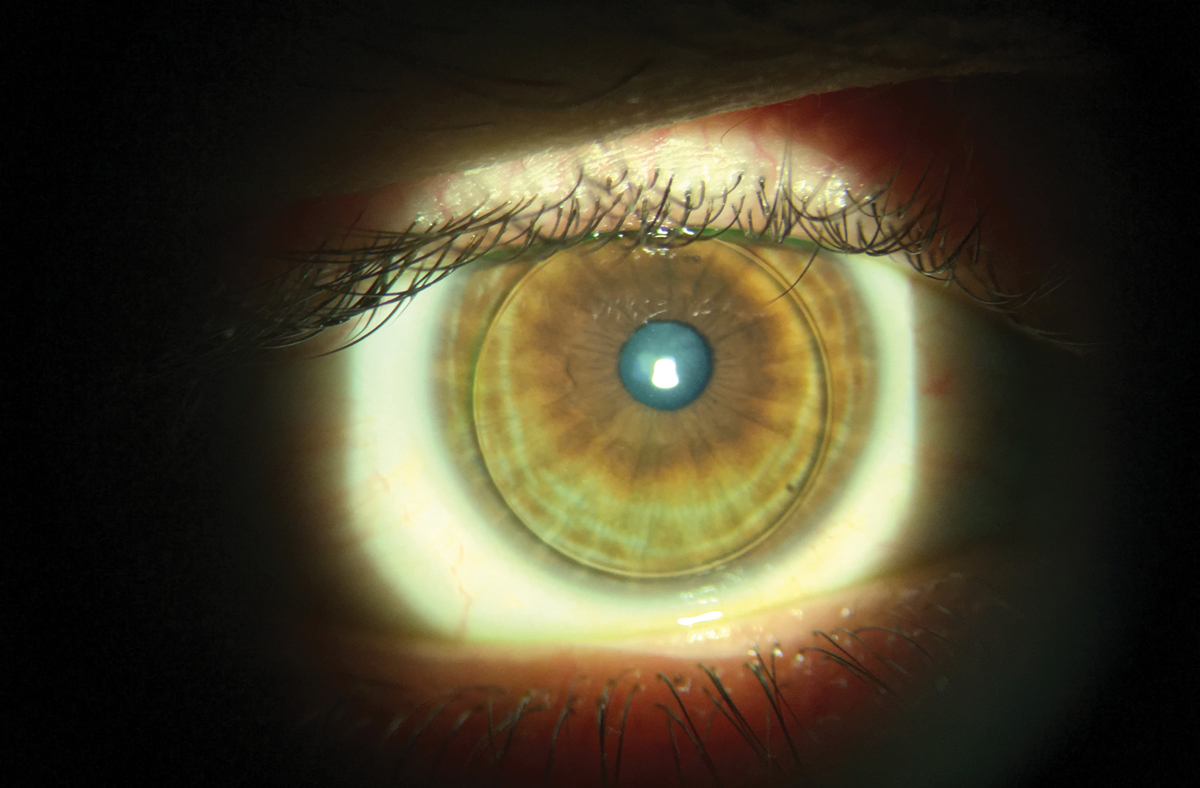 |
| Moving established GP wearers to multifocal designs can be an easy transition. Click image to enlarge. |
Refining the Fit
Providing that initial wow factor is the best way to start off on the right foot. Multifocals can be fit both empirically and diagnostically. Although diagnostic fitting sets are available for custom soft toric multifocals, you can order corneal GP multifocals and now hybrid multifocals empirically. This method can save chair time by producing an initial lens based off data provided to the laboratory. If refinements are necessary, these changes are often minor since empirically designed lenses can be quite accurate.
Scleral multifocals are best fit diagnostically because haptic alignment and lens centration are imperative. Lens power can also vary based on lens vault and variable tear layer. Although it is time consuming, fit scleral multifocals in two phases—first perfect the lens fit and then add the multifocal optics.
Once lenses are dispensed, evaluate progress after one to three weeks, as it allows for adequate adaptation to both fit and vision. If troubleshooting is required, evaluate lens fit and visual performance.
For lenses of all modalities and design, centration is critical to the success of the multifocal optics. If distance and near optics aren’t presented properly, then vision will be poor at one or both working distances. If soft toric multifocals have been fit, confirm rotational stability. A rotationally unstable lens is useless and must be corrected first.
Visual performance is best evaluated binocularly at both distance and near; however, monocular assessment can be useful if the patient feels off-balance. When distance vision is the concern, modify distance power, reduce add power or change zone sizes. Conversely, if near vision needs improvement, push plus power in the distance prescription, increase add power or change zone size. If small refinements are needed, it is good practice to adjust only one variable at a time.
Many viable contact lens options are available for your patients with presbyopia and astigmatism. Communicating with them and making them aware of the solutions at their disposal can help reach or exceed their expectations.
Dr. Ensley practices at Gaddie Eye Centers in Louisville, KY. He is a Fellow of the American Academy of Optometry and the Scleral Lens Education Society.
Dr. Jose is an assistant professor at Midwestern University-Chicago College of Optometry in Downers Grove, IL. She is a Fellow of the American Academy of Optometry and the Scleral Lens Education Society.
| 1. United States Census Bureau. Age and sex composition in the United States: 2018. www.census.gov/data/tables/2018/demo/age-and-sex/2018-age-sex-composition.html. Last revised July 11, 2019. Accessed February 5, 2020. 2. Rueff EM, Bailey MD. Presbyopic and non-presbyopic contact lens opinions and vision correction preferences. Cont Lens Anterior Eye. 2017;40(5):323-8. 3. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39:92-98. 4. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26:168-74 5. Rueff EM, Varghese RJ, Brack TM, et al. A survey of presbyopic contact lens wearers in a university setting. Optom Vis Sci. 2016;93:848-54. 6. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011;37:20-5. 7. Efron N, Nichols JJ, Woods CA, Morgan PB. Trends in US contact lens prescribing 2002 to 2014. Optom Vis Sci. 2015;92:758-67. 8. Richdale K, Berntsen DA, Mack CJ, et al. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84:969-75. 9. Berntsen DA, Cox SM, Bickle KM, et al. A randomized trial to evaluate the effect of toric versus spherical contact lenses on vision and eyestrain. Eye Contact Lens. 2019;45(1):28-33. 10. Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124-43. 11. Bennett ES. Contact lens correction of presbyopia. Clin Exp Optom. 2008;91:265-78. 12. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low astigmatic presbyopia. Optom Vis Sci. 2006;83:266-73. 13. Woods J, Woods C, Fonn D. Visual performance of a multifocal contact lens versus monovision in established presbyopes. Optom Vis Sci. 2015;92(2):175-182. 14. Nichols JJ, Fisher D. Contact lenses 2018. CL Spectrum. 2019;34:18-23. |


