Scleral lenses have myriad indications beyond the correction of irregular astigmatism. Sclerals are commonly used for rehabilitation of the ocular surface, even in cases of severe exposure and non-healing epithelial defects. Since scleral lenses are rotationally stable with minimal movement with blinking, they are currently being used as a stable platform for a range of optical applications.
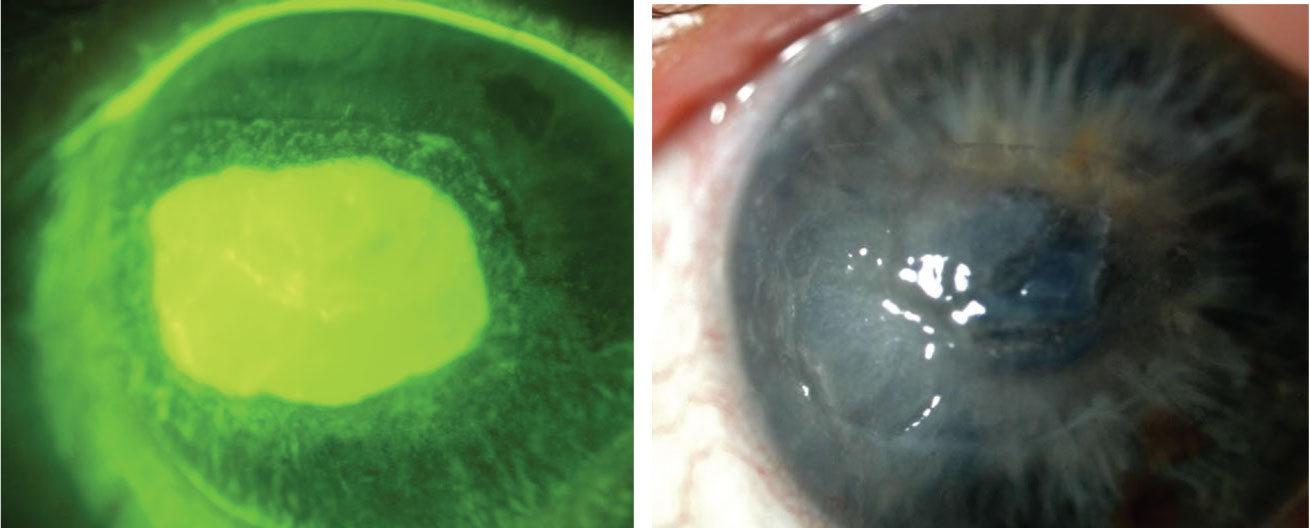 |
| One study reported treating longstanding retinal pigment epithelial detachment with extended-wear scleral lenses using moxifloxacin in the scleral lens reservoir, and none of the eyes developed microbial keratitis. Click image to enlarge. |
Drug Delivery
Scleral lenses for this purpose are an exciting possibility that can have far-reaching benefits across a multitude of ocular conditions. Interestingly, it is not a new concept. One of the first reports of using modern gas permeable scleral lenses as a vehicle for therapeutic topical drug delivery and antibiotic prophylaxis was described in 2000.1 They noted that fluorescein applied to the surface of the lens slowly seeped into the post-lens fluid reservoir and remained up to 24 hours later. Tear dynamics and scleral lenses were even studied in the early 1970s and referenced the phenomenon of fluorescein entrapment from work done in 1952.2 In fact, many studies have examined the turnover rate of fluorescein, or lack thereof, especially when it comes to midday fogging.3-6 This quality of slow turnover of tears underneath a scleral lens suggests that the drug may maintain its constant ocular contact during the entire duration of scleral lens wear with minimal loss.
Where to Turn for Scleral Lens FabricationBy RCCL Staff There are over a dozen US scleral lens manufacturers to choose from, depending on the needs of your patients. Whether you’re already fitting sclerals or just now ramping up to add the modality, check out the list of labs below that currently manufacture scleral lenses. The names listed after each company represent the person of contact for inquiries on product offerings or sales. ABB Optical Group: Andy Jackson, Ann Shackelford AccuLens: Troy Miller Advanced Vision Technologies: Keith Parker Alden Optical: Sam Ewing Art Optical Contact Lens: Jill Anastor Blanchard Contact Lens: Jean Blanchard BostonSight: Sara Yost Custom Craft Lens Service: Daren Nygren Essilor Custom Contact Lens Specialists: Jeff Birk Metro Optics: Steve Webb TruForm Optics: Jan Svochak, George Mera Valley Contax: Josh Adams Visionary: Cindy Belliveau Visionary Optics: Monica Sanders X-Cel Specialty Contacts: Derrell James |
Constant contact of topical ocular medications is an ideal situation, especially considering that most of the ocular medications are lost to drainage after 15 to 30 seconds.7 The tear turnover rate is approximately 16% per minute. Therefore, all of the drug should disappear within ten minutes after initial administration. Furthermore, the instilled drop is diluted to approximately one-third of the original strength—that is, if the drop even makes it onto the ocular surface.8 Compliance is always an issue with all forms of prescription medications, and ocular medications are no exception. Correct application of topical ocular medications is not always properly performed.9-11 There are a variety of limitations to the optimal usage of topical medications. Patients with poor dexterity, hand tremors and problems with grip may make the administration of medications challenging. Topical medications may require more frequent administration and doses can easily be missed or forgotten even under the best intentions and circumstances. Therefore, single administration of topical medications in the reservoir of a scleral lens seems like an ideal solution as long as the patient can successfully apply the lens.
In the literature, there have been examples of drug delivery with scleral lenses. Extended wear of scleral lenses was used to resurface persistent epithelial defects. In the first retrospective review of epithelial defects, there were four cases of microbial keratitis in 19 eyes with a variety of antibiotics used including ciprofloxacin, ofloxacin, trimethoprim polymyxin B sulfate, and polymyxin B gramicidin.1 Subsequently, twenty eyes with epithelial defects were treated with extended wear using moxifloxacin in the scleral lens reservoir, and none of the eyes developed microbial keratitis.12 The advantage of using moxifloxacin, a fourth-generation fluoroquinolone, is that it is self-preserved, with no added preservatives that can be toxic to the corneal surface.13 This is consistent with the importance of using non-preserved filling solutions in the scleral lens reservoir.
The treatment of persistent epithelial defects with scleral lenses using antibiotic (moxifloxacin) prophylaxis was published in different case series studies.14-16 Additional supplements were also administered in the lens including autologous serumand amnion in some cases.16
Scleral lenses have also been used to deliver compounded preservative-free bevacizumab, which is a recombinant, monoclonal antibody that binds to and deactivates vascular endothelial growth factor (VEGF). Topically, bevacizumab has been used to reduce active neovascularization and improve comfort in patients with Stevens-Johnson syndrome.17 Drug delivery of bevacizumab for corneal neovascularization was first reported in 2009 in five patients with success.18 Later reports looked at long-term status of 13 patients where only one patient had progression of neovascularization.19 While it has been shown to be successful, great care must be taken when using bevacizumab due to complications of poor wound healing and systemic absorption of the medication.
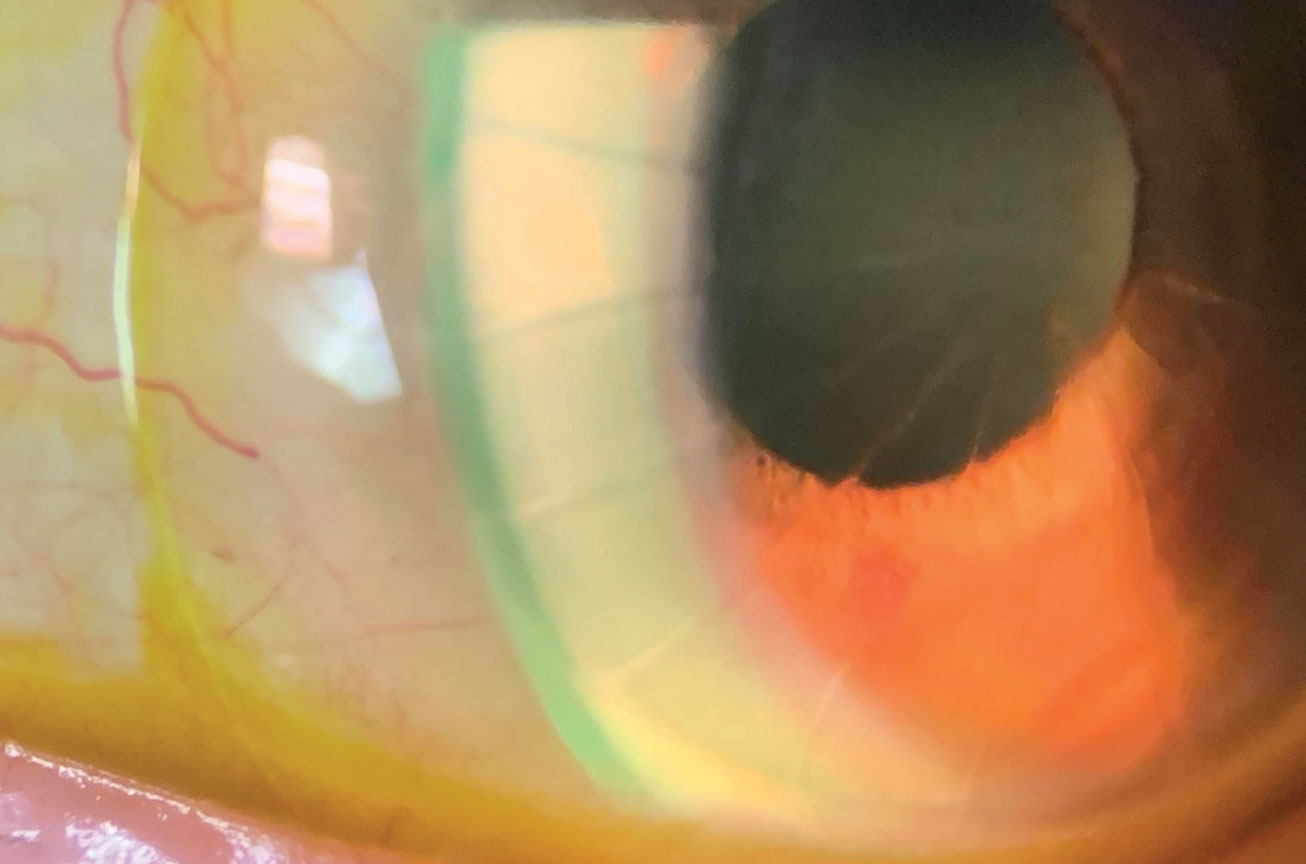 |
| Studies have reported on the use of anti-VEGF agents in the bowl of a scleral lens to treat corneal neovascularization. Click image to enlarge. |
In animal studies, drug delivery of ofloxacin demonstrated corneal and aqueous humor concentrations higher than the minimum inhibitory concentration for Staphylococcus epidermidis, Staph. aureus, Haemophilus influenzae, Streptococcus pneumoniae and Pseudomonas aeruginosa.20 Cultivated adipose-derived stem cells were cultured on the back surface of scleral lenses and administered to rabbits with alkaline burns. Those treated with the stem cells had less neovascularization, no symblepharon formation and less haze.21
This is an exciting time for the potential uses of scleral lenses for drug delivery, but there is a need for research in this area. The current topical drugs applied in the scleral lens reservoir are diluted with the filling solution. The appropriate concentrations of medications must be determined, and the length of exposure may also need to be examined. Furthermore, some of the medications themselves may be toxic to the corneal surface. Despite these considerations, the potential to treat a variety of ocular conditions and reduce concerns about compliance is exciting.
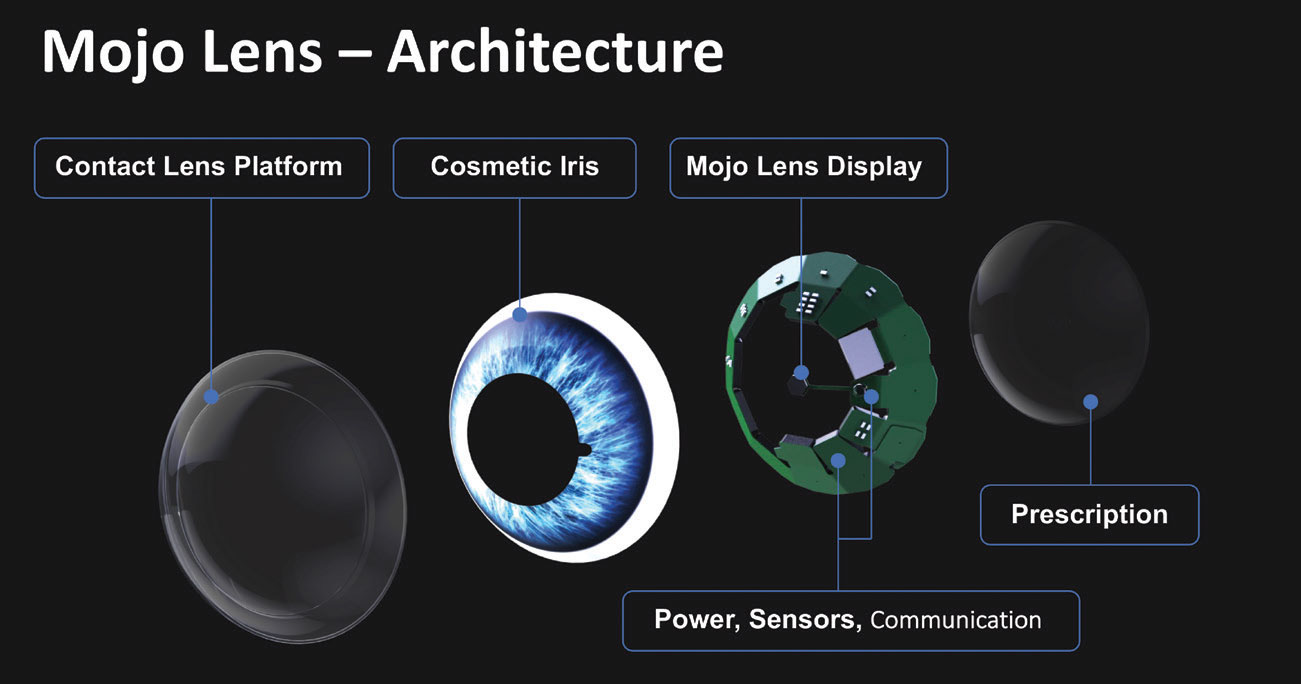 |
| This scleral lens in development uses an LED display to incorporate AR into a patient’s vision. Photo: Mojo Vision. Click image to enlarge. |
Augmented Reality
One innovative new technology developed by Mojo Vision is a smart scleral lens that features augmented reality (AR).22 A 14,000 pixel-per-inch MicroLED display measuring less than 0.5mm in diameter with a pixel-pitch of 1.8µm provides a small and dense display. The Mojo lens has custom application specific integrated circuit designs that incorporate a 5GHz radio and an ARM Core M0 processor that transmit sensor data off the lens and stream AR content to the display. A custom-configured accelerometer, gyroscope and magnetometer continuously tracks eye movements, so that the AR imagery is stable with eye movement.
The lens is controlled with a unique and intuitive interface based on eye tracking that allows users to access content and select items using the natural movement of the eyes. The anatomy of this lens includes an optic zone, transition zone and landing zone similar to commercially available scleral lenses. The technology may also help presbyopes so that they may experience sustained clear vision at all distances as well as patients with low vision.
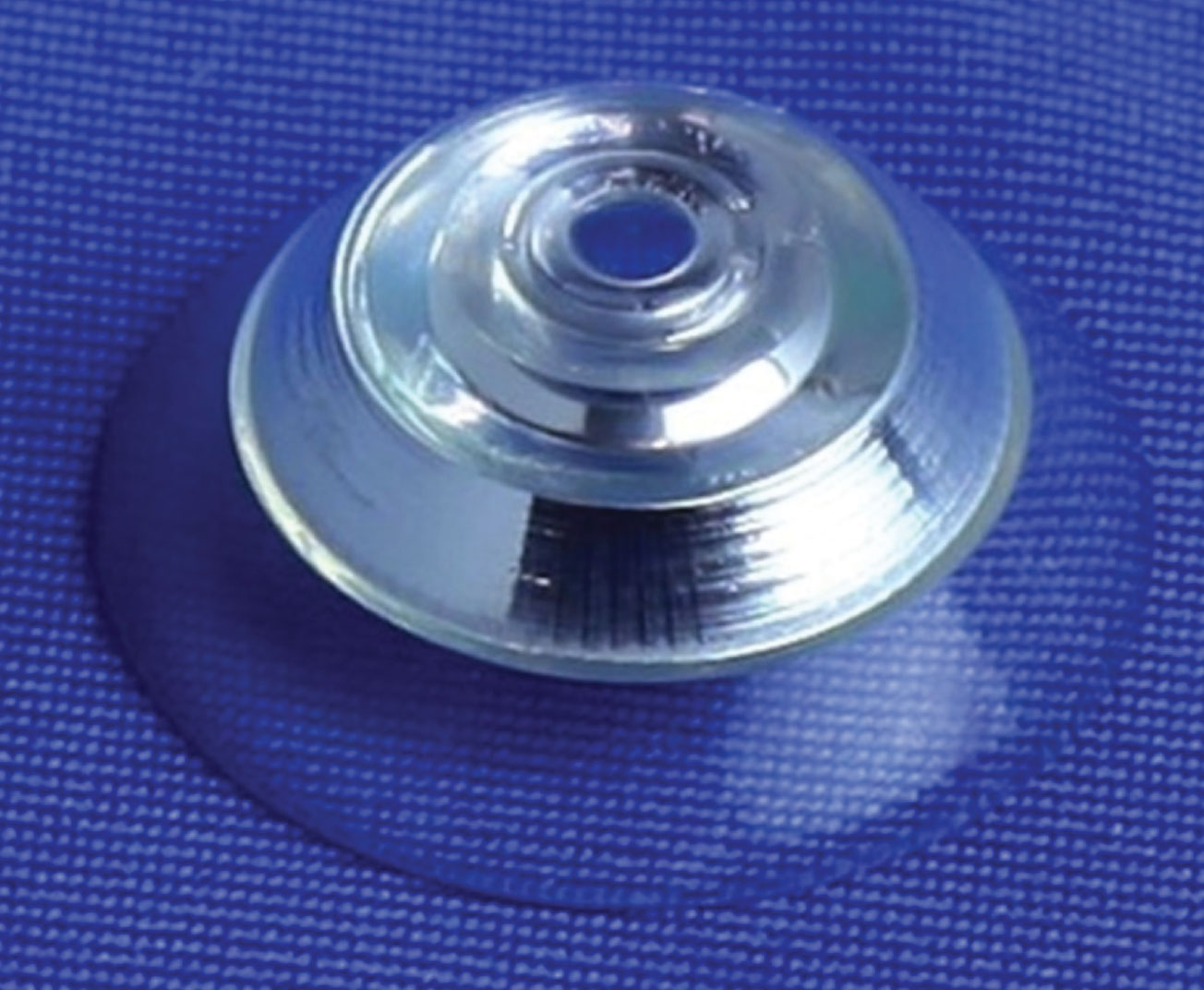 |
| An image of a scleral lens telescope. Photo: Jacobs School of Engineering/University of California San Diego. Click image to enlarge. |
Electrolyte-Sensing Lens
It is well established that dry eye disease is complex in its etiology and management while also being debilitating to patients. Scleral lenses are often used as a palliative treatment for dry eye and severe ocular surface disease, but with sensor integration, they may become diagnostic as well. One study reported on a unique scleral lens that can measure pH, sodium, potassium, calcium, magnesium and zinc levels.23
A carbon dioxide laser ablated the scleral lens and created microconcavities, and the sensors were fluorescent probes for the electrolytes. A silicone hydrogel film was bonded to the lens to create a sealed and leakproof lens that protected the probes from evaporation. The electrolytes that were measured were free to diffuse through the system. By using a combination of LEDs, optical filters and an imaging unit, the concentrations and pH were able to be quantified.23 The ophthalmic system allows the assessment of dry eye severity stages and the differentiation of its subtypes. Hopefully, this technology will become readily available to assist the diagnostic process of dry eye disease.
Scleral Lens Telescopes
Contact lens reflecting telescopes are an alternative to spectacle-contact lens refracting telescopes, which eliminate the need for a high-powered spectacle lens.24 A combination of mirrors called a Cassegrain reflector and polarizers embedded within a scleral lens allows the wearer to alternate between distance refractive correction and 2.8x magnification triggered by a forced blink sensed by a detector mounted on a pair of spectacles, which alters the polarization state of the spectacles.
A scleral lens including a reflecting telescope is currently under development, to provide up to approximately three-times magnification and does not require a high-powered spectacle lens objective.24-26 The proposed lens design has a total lens thickness over 1,000µm. Thus, providing adequate corneal oxygenation during lens wear remains a design challenge to minimize corneal hypoxic stress.
Many patients and practices today can benefit from fitting scleral lenses, which can be improved further upon and solve many issues. Sclerals may function as an ideal drug delivery system to provide a therapeutic level of drug to the desired target tissue. We are one step closer to incorporating augmented reality and contact lens telescopes to assist our patients’ vision. The future of this modality is bright, as many researchers and innovators continue to demonstrate the amazing uses it can provide in the modern era.
Resources for Scleral FittingScleral lenses have been gaining momentum and popularity; however, just like their size, they may be intimidating. There are many resources available to practitioners with all levels of experience. A comprehensive textbook, Contemporary Scleral Lenses: Theory and Application that we’ve developed details the extensive history of scleral lenses, examines all of the indications for use and describes scleral lens shape as well as ocular shape. Readers will learn how to assess the fit of scleral lenses and recognize complications. Troubleshooting scleral lens problems, practice management, and a wide variety of topics are included in this textbook.1 Another valuable textbook was written by Daddi Fadel entitled Scleral Lens Issues and Complications: Their Recognition, Etiology and Management. She explores the use of different dyes in the assessment of scleral lens fits, scleral shape evaluation using diagnostic lenses and slit lamp evaluation. Various scleral lens issues and complications from ill-fitting relationships , handling and patient compliance are described and clinical pearls to troubleshoot these problems are provided.2 There are three informative and introductory scleral lens guides that are available for free download. “A Guide to Scleral Lens Fitting” by Eef van der Worp was one of the first modern scleral lens resources written in 2010. It is still available for download in numerous languages.3 To date there are over 38,000 downloads of this original guide and resource. The guide had since been updated in 2015.4 Melissa Barnett and Daddi Fadel collaborated on a “Clinical Guide to Scleral Lens Success.” This guide can also be downloaded and is available in English, Italian, Portuguese, Russian and Spanish and has numerous photos of scleral lens fits and complications.5 The “Scleral Lens Fit Scales” is a valuable tool that is available for download from Ferris University Michigan College of Optometry that is both in English and Spanish. The images demonstrate set amounts of clearance ranging from 50µm to 600µm. Images of fitting relationships of the landing zone and edge relative to the conjunctiva are also demonstrated in this resource.6 “The Scleral Lens Education Initiative” is a downloadable scleral lens e-resource featuring published research, evidence-based clinical recommendations and expert-backed insights.7 Clinically relevant information is applicable to practitioners with all levels of experience. The BCLA CLEAR scleral report provides a brief historical review of scleral lenses and a detailed account of contemporary scleral lens practice including common indications and recommended terminology.8 The report illustrates recent research on the ocular surface in addition to a comprehensive account of modern scleral lens fitting and on-eye evaluation. This report summarizes the latest research and clinical understanding of scleral lens fit assessment. The Scleral Lens Education Society (SLS) has numerous resources on their website (sclerallens.org). Patients can be directed to an instructional video teaching them about proper application and removal of their scleral lenses. There is a practitioner locator for scleral lens practitioners that have earned their fellowship in the organization. For practitioners, there are videos and fitting tips. It is free to join and access the resources on the site. The Gas Permeable Lens Institute website, gpli.info, is an educational resource for all types of gas permeable and specialty contact lenses—including scleral lenses. The site offers resources on billing and coding medically necessary contact lenses, archived videos and webinars. It also has printed materials including application and removal laminated instructions for the office and patients. On Facebook, there is a dedicated group called the Scleral Lens Practitioners that welcomes everyone interested in scleral lenses. Colleagues collaborate with one another, sharing their experiences and seeking advice for interesting and complicated cases.
1. Barnett M, Johns LK. Contemporary Scleral Lenses: Theory and Application Volume 4. Bentham Science; 2017. 2. Faddel D. Scleral Lens Issues and Complications. sclerallensbook.com. Accessed September 13, 2022. 3. Van der Worp, E. A Guide to Scleral Lens Fitting. Forest Grove, OR: Pacific University. 2011: Pacific University Libraries at CommonKnowledge. commons.pacificu.edu/work/sc/6797b4a0-f0aa-43c6-a05e-a25df442591e. Accessed September 13, 2022. 4. Van der Worp E. A Guide to Scleral Lens Fitting 2nd ed. Forest Grove, OR: Pacific University. 2015: Pacific University Libraries at CommonKnowledge. commons.pacificu.edu/mono/10. Accessed September 13, 2022. 5. Barnett M, Fadel D. Clinical Guide for Scleral Lens Success. www.scleralsuccess.com. Accessed September 13, 2022. 6.. Scleral lens fit scales. Ferris State University Michigan College of Optometry Vision Research Institute. www.ferris.edu/HTMLS/colleges/michopt/vision-research-institute/pdfs-docs/Scleral-lens-fit-scales_v2.pdf. Accessed September 13, 2022. 7. 2021 Scleral Lens Education Initiative. Review of Optometric Business. www.reviewob.com/2021-scleral-lens-education-initiative. Accessed September 13, 2022. 8. Barnett M, Courey C, Fadel D, et al. CLEAR—scleral lenses. Cont Lens Anterior Eye. 2021;44(2):270-88. |
Dr. Barnett is a principal optometrist at the UC Davis Eye Center. She is immediate past chair of the American Optometric Association’s Contact Lens and Cornea Section, past president of the Scleral Lens Education Society, a Fellow of the American Academy of Optometry, a Diplomate of the American Board of Certification in Medical Optometry, a fellow and global ambassador of the BCLA and a board member of the GPLI. Dr. Barnett has consulting and/or lecturing relationships with ABB, Acculens, Bausch + Lomb, Contamac, CooperVision, EveryDay Contacts, Johnson & Johnson Vision Care, SynergEyes and Tangible Science, among others.
Dr. Johns practices at Massachusetts Eye and Ear and is a research associate in the department of Ophthalmology at Harvard Medical School. She is a fellow of the American Academy of Optometry, Scleral Lens Education Society and the BCLA. She has no disclosures.
1. Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol. 2000;130(1):33-41. 2. Ko L, Maurice D, Ruben M. Fluid exchange under scleral contact lenses in relation to wearing time. Br J Ophthalmol. 1970;54(7):486-9. 3. Tse V, Tan B, Kim YH, et al. Tear dynamics under scleral lenses. Cont Lens Anterior Eye. 2019;42(1):43-8. 4. Paugh JR, Chen E, Heinrich C, et al. silicone hydrogel and rigid gas permeable scleral lens tear exchange. Eye Contact Lens. 2018;44(2):97-101. 5. Skidmore KV, Walker MK, Marsack JD, Bergmanson JPG, Miller WL. A measure of tear inflow in habitual scleral lens wearers with and without midday fogging. Cont Lens Anterior Eye. 2019;42(1):36-42. 6. Nau CB, Schornack MM, McLaren JW, et al. Tear exchange, intraocular pressure, and wear characteristics of quadrant-specific versus spherical haptic scleral lenses. Eye Contact Lens. August 16, 2022. [Epub ahead of print]. 7. Shell JW. Pharmacokinetics of topically applied ophthalmic drugs. Surv Ophthalmol. 1982;26(4):207-18. 8. Maurice D, Mishima S. Ocular pharmacokinetics. In Sears ML, ed. Pharmacology of the Eye. New York, Springer-Verlag; 1984:19-116. 9. Stone JL, Robin AL, Novack GD, Covert D, Cagle GD. An objective evaluation of eye-drop instillation in glaucoma patients. Arch Ophthalmol 2009;127(6):732-6. 10. Kass MA, Hodapp E, Gordon M, et al. Patient administration of eyedrops: observation. part II. Ann Ophthalmol. 1982;14(9):889-93. 11. Kass MA, Hodapp E, Gordon M, et al. Part I. patient administration of eyedrops: interview. Ann Ophthalmol 1982;14(8):775-9. 12. Lim P, Ridges R, Jacobs DS, Rosenthal P. Treatment of persistent corneal epithelial defect with overnight wear of a prosthetic device for the ocular surface. Am J Ophthalmol. 2013;156(6):1095-101. 13. Schlech BA, Sutton S, Rosenthal RA, et al. Antimicrobial preservative effectiveness of VIGAMOX. Invest Ophthalmol Vis Sci. 2004;45(13):4913. 14. Ciralsky JB, Chapman KO, Rosenblatt MI, et al. Treatment of refractory persistent corneal epithelial defects: a standardized approach using continuous wear PROSE therapy. Ocul Immunol Inflamm. 2015;23(3):219-24. 15. Khan M, Manuel K, Vegas B, et al. Case series: extended wear of rigid gas permeable scleral contact lenses for the treatment of persistent corneal epithelial defects. Cont Lens Anterior Eye. 2019;42(1):117-22. 16. He X, Donaldson KE, Perez VL, Sotomayor P. Case series: overnight wear of scleral lens for persistent epithelial defects. Optom Vis Sci. 2018;95(1):70-5. 17. Uy HS, Chan PS, Ang RE. Topical bevacizumab and ocular surface neovascularization in patients with Stevens-Johnson syndrome. Cornea. 2008;27(1):70-3 18. Lim M, Jacobs DS, Rosenthal P, Carrasquillo KG. The Boston Ocular Surface Prosthesis as a novel drug delivery system for bevacizumab. Semin Ophthalmol. 2009;24(3):149-55. 19. Yin J, Jacobs DS. Long-term outcome of using Prosthetic Replacement of Ocular Surface Ecosystem (PROSE) as a drug delivery system for bevacizumab in the treatment of corneal neovascularization. Ocul Surf. 2019;17(1):134-41. 20. Laballe R, Vigne J, Denion E, Lemaitre F, Goux D, Pisella PJ. Preclinical assessment of scleral lens as a reservoir-based ocular therapeutic system. Cont Lens Anterior Eye. 2016;39(5):394-6. 21. Espandar L, Caldwell D, Watson R, et al. Application of adipose-derived stem cells on scleral contact lens carrier in an animal model of severe acute alkaline burn. Eye Contact Lens. 2014;40(4):243-7. 22. Phan C-M. Beyond 20/20: the Mojo smart lens. Contact Lens Update. February 6, 2020. contactlensupdate.com/2020/02/06/beyond-20-20-vision-the-mojo-smart-lens. Accessed September 13, 2022. 23. Yetisen AK, Jiang N, Castaneda Gonzalez CM, et al. Scleral lens sensor for ocular electrolyte analysis. Adv Mater. 2020;32(6):e1906762. 24. Arianpour A, Schuster GM, Tremblay EJ, et al. Wearable telescopic contact lens. Appl Opt. 2015;54:7195-204. 25. Schuster GM, Arianpour A, Cookson S, et al. Wink-controlled polarization-switched telescopic contact lenses. Appl Opt. 2015;54(32):9597-9605. 26. Tremblay EJ, Stamenov I, Beer RD et al. Switchable telescopic contact lens. Opt Express 2013;21(13):15980-6. |


