 |  |
Between the two of us, we have been fitting scleral lenses for more than 25 years. We have encountered the steepest corneas, the worst LASIK ectasias, the flattest plateaus and the driest eyes. We’ve found that having a working laboratory partnership is critical to our scleral lens success. Equally important is completing training, being skilled and paying attention to detail to provide our patients good health, comfort and clarity.
Sclerals are unlike any lens a patient has seen or worn before. Maybe some have heard of them. Others can only imagine what they’re like. But everyone is always shocked by how big the lenses actually are, even if they’ve been previously warned. As such, the initial insertion of the lens is always associated with a level of trepidation. These patients are encountering something alien to them that comes with a brand new set of wear and care instructions. We’ve learned that if you want to maximize your success and patient’s outcomes, you need to start with proper communication and education.
Lens Presentation
Performing scleral lens workshops around the country, we have observed hundreds of practitioners learning how to fit and evaluate contact lenses, but one crucial area that is often missed, even by us, is teaching how to explain the lenses. Consequently, most practitioners use the lens itself to educate the patient, who, at this point, is too busy trying to comprehend how they’ll be able to get the lens in their eye to hear a single word the practitioner is saying.
We have found that new patients perceive scleral lenses differently than conventional cornea-fit contact lenses, so, as such, it may be helpful to refer to them in a different way—as a device. It’s important to make sure the patient can visualize the lens before you actually show them what it looks like by telling them that it will cover nearly all of their visible eye, including the white part. Generally, we tend to be more accepting of things, especially things we’ve never seen before, if we understand them first, and giving patients a good explanation of what a scleral lens is ahead of time may help reduce anxiety.
Next, we like to explain how the lens works. Let the patient know that the larger surface of the lens vaults over the top of the cornea or, in most cases, the irregular part of their eye, and is filled with a moisturizing solution that is used when putting the lens in.
Lastly, we discuss insertion and removal methods with the patient. Explain that since scleral lenses are larger than conventional contact lenses, they require some simple tools to help get them in and out of the eye. Then show them how to use these tools. We give patients several tools and have more at the office if they need them.
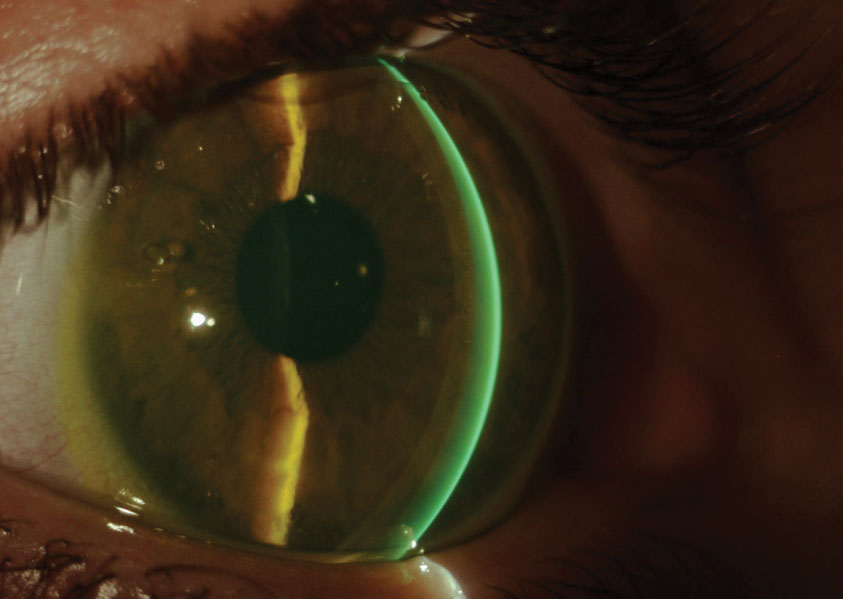 |
| Scleral lenses can make a world of difference once a patient is educated thoroughly. Click image to enlarge. |
Lens Fitting
Now, it’s time for the lens fitting. To start, we offer the diagnostic trial lens that we intend to place on the patient’s eye to them to get them comfortable. We reassure them that the lenses are safe and comfortable, and, in the case that they are not, we make modifications. Clarify that diagnostic lenses are demonstration or fitting devices and are not intended to match the patient’s prescription or correct their vision.
Once the patient is ready, we show them how to clean the lens, place it on the insertion device and fill it with solution. Then we demonstrate on our own eyes how we will hold their eyelid to insert the lens. It’s important that the patient looks straight ahead when we place the lens on their eye. Once we ensure there are no bubbles in the lens, we have the patient close their eye and let us know what the lens feels like.
At this point, different practitioners proceed in different fashions. Some check the fit with an OCT, while others use a slit lamp. Regardless of the method you choose, talk your patient through what you’re doing and reassure them, especially if they are not finding the lens to be comfortable. Once the ideal fit is achieved, it is time for the over-refraction. Some practitioners only do spherical over-refractions and use over-glasses for cylinder and presbyopic correction. Others do spherocylindrical over-refractions and put the cylinder in the lens. We strongly suggest not making any claims or promises about the patient’s final vision based on the over-refraction. With lens settling, fogging and other complications that can arise, it is best to set expectations at a point when you can confidently say you’ve met your objective.
Some practitioners allow the patient to remove the lens after the initial insertion, while others like to remove it for them. We see the value in both and proceed based on the patient’s demeanor. If the patient is comfortable with it, we allow them to remove the lenses to show them how easy it is and to start removal training. However, if the patient shows signs of nerves or anxiety about the lenses or the fitting process, we elect to remove the lenses on their behalf to avoid overcomplicating the rest of the process.
The initial presentation and fitting of scleral lenses sets the tone for a patient’s entire experience with them. Whether a patient is willing to try the lenses, how much effort they put into wearing them and their perceptions toward them all start here. If we can reduce a patient’s anxiety and motivate them upfront, success becomes much more attainable.


