Empirical contact lens fitting is defined as the designing of lenses without the use of diagnostic lenses.1 This is traditionally accomplished by providing refractive information supplemented by keratometry values to the fabricating laboratory. In 2024, the empirical fitting of gas permeable (GP) lenses has become more of the rule than the exception. This is the result of many advancements, including:
- The lenses are designed through a well-tested manufacturer’s nomogram.
- The use of contemporary online calculators.
- The use of corneal topography data, which sometimes includes lens design software.
- Corneal-scleral topographers allowing for the ability to design scleral lenses empirically through profilometry.
- Improved manufacturing methods, including state-of-the-art lathing equipment.
As a result, most designs commonly used today can be successfully designed empirically, especially with the recent advancements in both instrumentation and manufacturing technology. These latter advances may ultimately result in the empirical fitting of all GP lenses in the future.
Why Empirical Fitting?
It most certainly saves chair time, with both patients and eyecare professionals (ECPs) benefiting from not having an initial fitting visit with application and subsequent disinfection of multiple diagnostic lenses. Empirical fitting also eliminates any concerns over whether a practice’s diagnostic lenses are properly disinfected and maintained.
Of course, a very important benefit is the powerful effect achieved when the initial GP lens worn provides very good vision. It would not be unrealistic to think that this “wow effect,” which is not uncommon with initial GP lens wear, would actually detract from the perception of initial awareness and serve as a very good incentive for ultimate success in this modality. This is a powerful effect for both patients and ECPs.
With today’s technology, a lens that has been empirically designed and subsequently manufactured can be customized specifically to the patient’s corneal topography and refractive considerations. Combined with an ultrathin, reproducible edge and optimized edge clearance (often pseudo-aspheric) peripheral designs, empirically designed GP lenses are likely to achieve an optimal lens-to-cornea fitting relationship which, in turn, enhances patient satisfaction.
 |
|
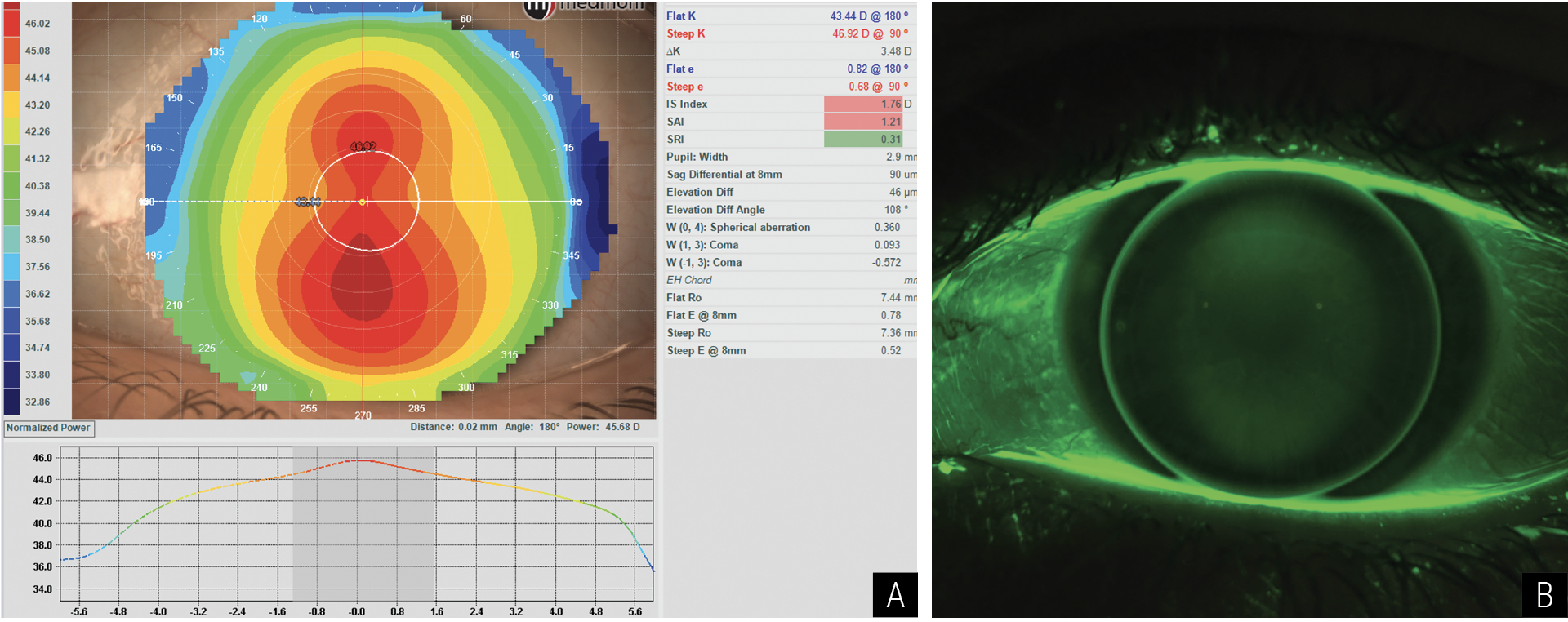
Fig. 1. (A) The topographical map of a patient. (B) The resultant empirical lens generated from the topographical and refractive information. Photo: Randy Kojima. Click image to enlarge. |
Fitting Challenges
Traditionally, and even today in practices that still maintain a large number of fitting sets, diagnostic fitting was the preferred modality for GPs. It allowed for the ECP to “trial” a lens on the eye and evaluate the fit and change the design to optimize the fitting relationship if necessary. This is followed by a careful overrefraction, thus providing a level of confidence that the lens ordered will ultimately fit well, provide optimal vision and result in patient success.
In the past, soft lenses were not available with both the quality and quantity of different refractive corrections. Limited technological capability of corneal topography software and laboratory fabrication methods (not as advanced) made empirical design less initially successful; therefore, diagnostic fitting was most certainly justified. In 2024, however, patients desiring contact lens wear expect to leave the office with lenses that will likely be successful after initial application. Diagnostic fitting is time-consuming, both for staff and the ECP, and time is money for a busy practice; certainly, this can serve as a disincentive to fit GP lenses in clinic.
There is also the “elephant in the room,” which is, of course, initial comfort. If the patient’s initial GP lens experience is with lenses that are not in their prescription, it would make sense that the resultant blurry vision would exacerbate any perceptions they have about the initial lens awareness. This could be quite disconcerting for both patient and ECP.
Diagnostic fitting sets themselves can pose several challenges. Each diagnostic lens is a standard design from the manufacturer and not necessarily custom-designed to provide the best possible lens-to-cornea fitting relationship, especially as you consider the advancements that have been made in recent years.2 Secondly, there is the matter of storage space and disinfection upkeep for each fitting set which can represent a challenge in the contact lens supply room. Recent standards require the disinfection of all trial contact lenses following guidance provided by the International Organization for Standardization 19979.2018(E) and endorsed by the American Optometric Association Contact Lens and Cornea section and American Academy of Optometry section on Cornea, Contact Lenses and Refractive Technologies.3 A practical, easy-to-use disinfection nomogram is available from the Gas Permeable Lens Institute.4
These standards are consistent with current COVID-19 concerns and the need to clean and thoroughly disinfect every diagnostic lens. However, these disinfection standards can be time-consuming to comply with, requiring attention to detail and appropriate logging.2 Likewise, these lenses are typically stored in a dry state and need to be both cleaned and conditioned (preferably stored in a multipurpose solution) prior to initial application for optimal surface wettability.
How to Optimize Success
There are myriad resources available to help ECPs achieve success in empirical fitting. A laboratory consultant can assist with lens selection design and troubleshooting. Since they manage their lab’s designs on a daily basis, their guidance throughout the entire fitting process is invaluable. ECPs can easily transmit corneal topography information and lens fit photos and/or video, the latter simplified by the use of a slit lamp camera or mobile phone slit lamp adaptor. Careful refraction of the patient’s refraction, lid position and pupil size are often helped in empirical design. Corneal topographers with lens design software, in particular, has been especially beneficial in empirical fitting with the ability to show the simulated fluorescein pattern such that an optimum fitting relationship would be likely after ordering the lens (Figures 1a and 1b).
Applications
There are many applications for empirical GP lens designs and the use continues to increase. According to a recent survey, the empirical prescribing habits (vs. diagnostic fitting) resulted in five modalities that were predominantly fitted empirically.5 This included multifocals (86%), torics (83%), spherical (79%), corneal reshaping (71%) and hybrids (67%).
GP multifocals. There are a number of presbyopic patients—including spectacle wearers and those dissatisfied with their vision in soft lens multifocals—who could benefit from empirical fitting of GP multifocals. Aspheric designs, in particular, can both result in good first fit success.6 An optimal fit would include movement with the blink. Initial lens awareness should be less than a standard spherical GP design. Fitting these can be as simple as providing the refractive (and topographic if available) results and add power to the laboratory. Pupil size can be another value add for determining best first-lens parameters in certain designs. Not all laboratories provide diagnostic lens fitting sets of their GP aspheric multifocal designs. However, diagnostic fitting regains the standard for fitting segmented, translating designs, to ensure the lens is translating on down gaze, is not lifted excessively on the blink and that the segment line is located in the appropriate position.
 |
|
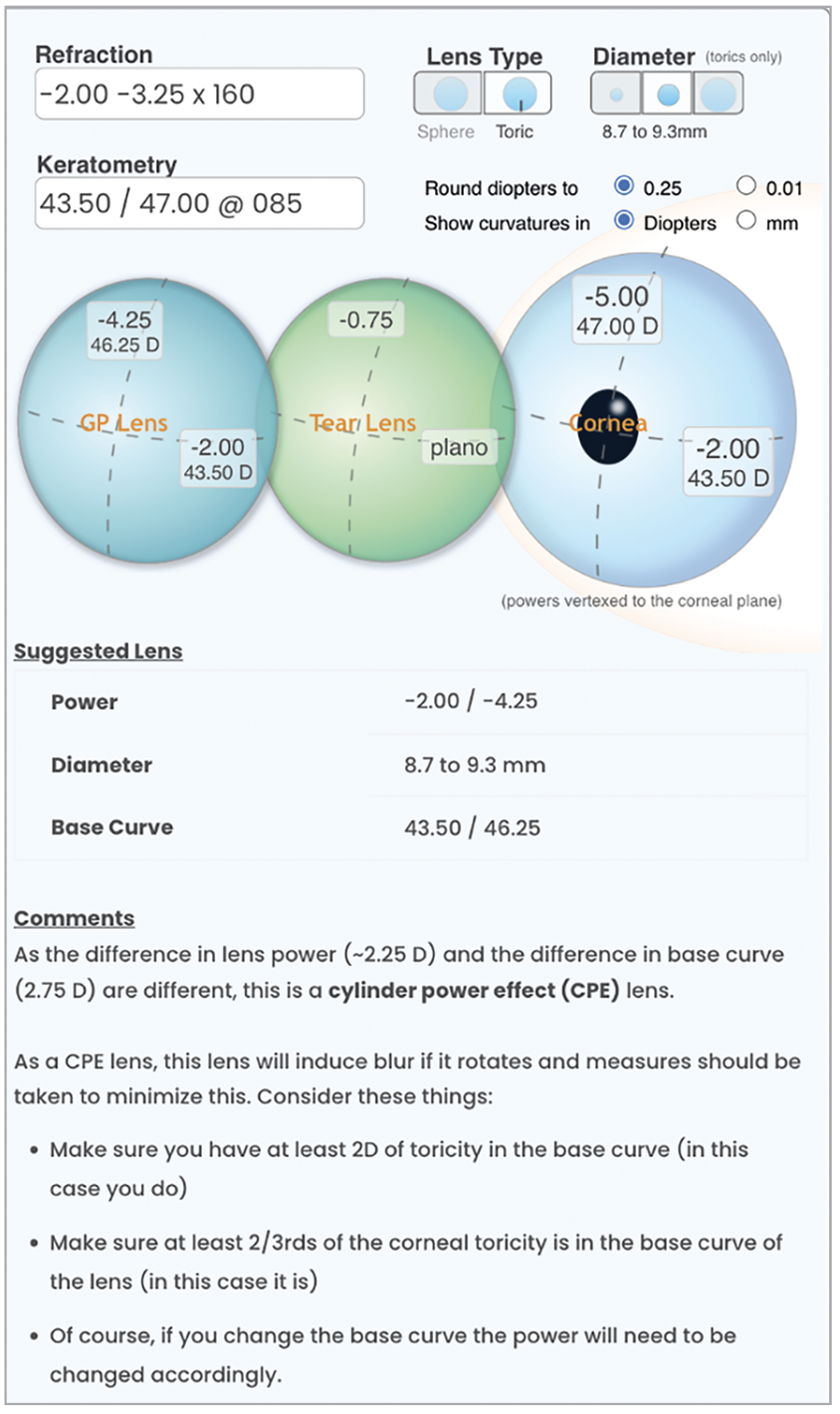
Fig. 2. A representative bitoric example using the GPLI Toric and Spherical Lens Calculator (Available at www.gpli.info). Photo: Todd Zarwell, OD. Click image to enlarge. |
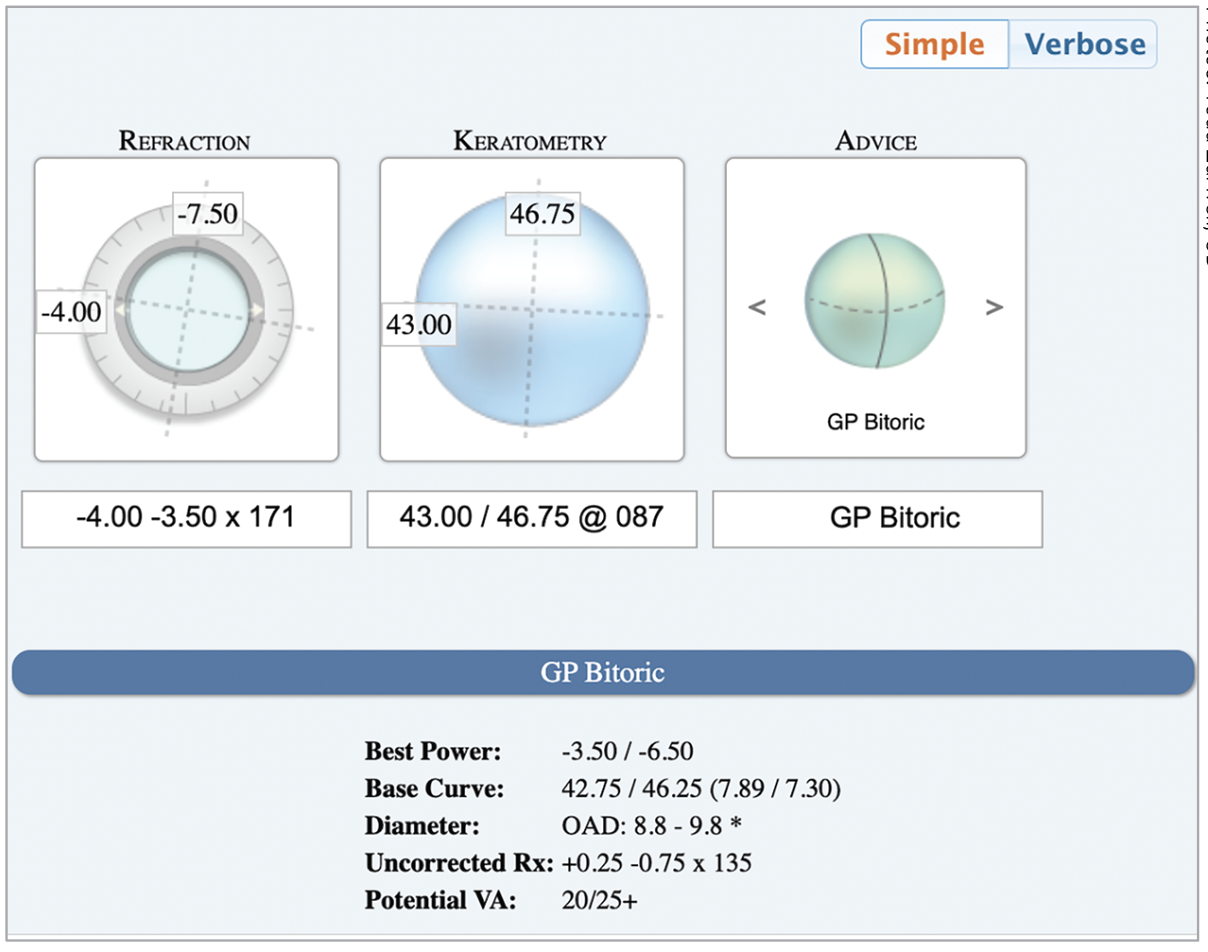
Torics. Fitting a bitoric lens is actually quite simple and can be more successful when compared to soft toric lenses due to better visual results.7 There are a number of online calculators that, in a matter of seconds, provide the necessary powers and base curve radii (Figure 2) while also providing some key design and fitting pearls (Figure 3). Other online calculators include the Mandell-Moore Guide for Empirical Bitoric Design and Dr. Clarke Newman’s custom bitoric fitting guide (both available at www.gpli.info). Both are downloadable forms that can allow ECPs to custom design a bitoric lens. GP bitoric lens success is also more likely as a result of improvements in the toric-generating lathes and tools in common use by laboratories today.
Spherical corneal GPs. Although less commonly used than in the past, the ability for manufacturers to make consistently good ultrathin lens designs custom manufactured to a given ocular surface bodes very well for first-fit success. The availability of several online calculators—as with toric lenses—is also quite beneficial.
Corneal reshaping. Whereas it was once commonplace to use diagnostic fitting sets or inventories to fit orthokeratology/corneal reshaping lenses, with today’s corneal topography capabilities, complimented by the ability to generate high-quality lenses, success can easily be achieved in the first fit. In fact, one multicenter study reported a first-fit success of 80% with empirically fit corneal reshaping lenses.8
 |
|
Fig. 3. A representative bitoric example using the EyeDock Calculator (www.eyedock.com). Photo: Todd Zarwell, OD. Click image to enlarge. |
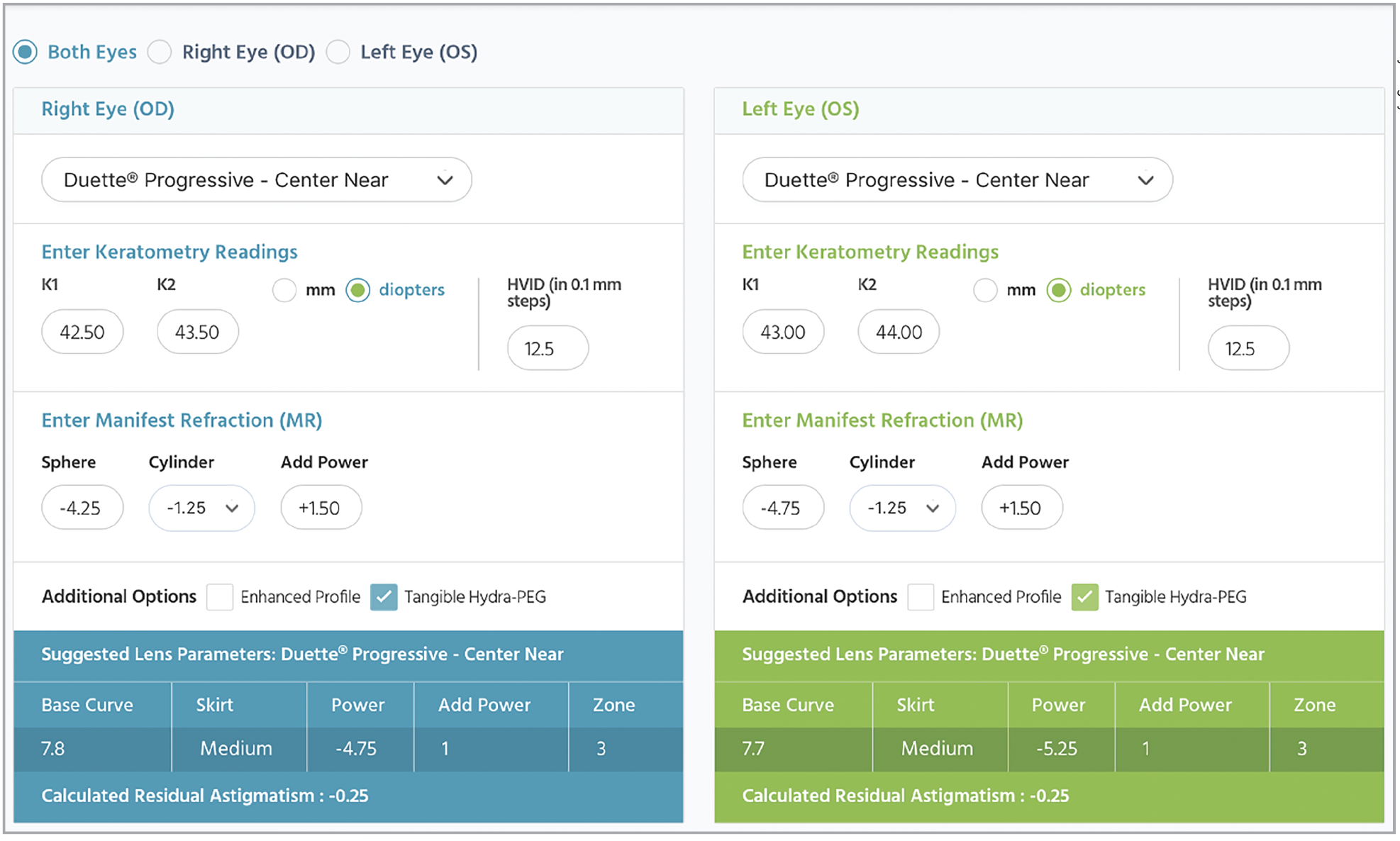
Hybrids. Essentially all forms of hybrids lenses can be ordered empirically. It is as simple as using the SynergEyes Empirical Lens Calculator, which calculates the lens parameters for the Duette Progressive Center-Near hybrid multifocal (Figure 4).
 |
|
Fig. 4. The SynergEyes Empirical Lens Calculator. Photo: SynergEyes. Click image to enlarge. |
What About Scleral Lenses?
As most of the sclerals are toric and asymmetrical, the use of diagnostic lenses has traditionally been recommended.9 However, elevation-driven scleral lens designs combined with the manufacturer’s ability to custom design the lenses using profilometry or corneal-scleral topographer information, is driving increased uptake and success in empirical scleral lens fitting. As more ECPs integrate advanced forms of topography instrumentation into their practice, this trend will continue.
Small-diameter corneal GPs for application on irregular corneas is still predominantly via diagnostic fitting as a result of the irregularity of the cornea, making it more challenging to determine what lens parameters would be optimum. That said, several topographers incorporate keratoconus lens design software to make empirical design possible in many cases.
Conclusion
The benefits of empirical GP lens fitting are numerous and only increase each new technological advance introduced to contact lens practice. At a time when increased efficiency and reduced chair time (if possible) can be critical to success, empirical fitting can contribute to patient satisfaction.
Sophisticated lens manufacturing equipment, complemented by high-quality in-office ocular surface instrumentation, is a marriage made for producing custom GP lenses that are well aligned to the eye, achieve less lens awareness and provide optimal vision—all without the need for a diagnostic lens fit.
Adoption of this approach enhances the patient’s sensation of initial comfort, optimizes ocular health and competes effectively with the inventory approach to soft lens fitting. And the good news is, it will only get better with time!
Dr. Bennett is Professor Emeritus at the University of Missouri St. Louis College of Optometry. He is past chair of the Contact Lens and Cornea Section Council of the American Optometric Association and is a diplomate and a past Chair of the Cornea, Contact Lenses and Refractive Technologies section of the American Academy of Optometry. Dr. Bennett is also a Fellow in the Scleral Lens Education Society and current president and executive director of the Gas Permeable Lens Institute.
1. Bennett ES, Sorbara L, Kojima R. Gas-permeable lens design, fitting and evaluation. In Bennett ES, Henry VA: Clinical Manual of Contact Lenses (5th ed.). Wolters Kluwer, Philadelphia, 2020:122-73. 2. Maller K. Empirical fitting of specialty GP lenses. Cont Lens Spectrum. 2021;36(8). 3. Sindt C, Bennett E, Szczotka-Flynn L, et al. Technical report: guidelines for handling multpatient contact lenses in the clinical setting. Optom Vis Sci. 2020;97:544-8. 4. Gas Permeable Lens Institute. Accessed January 20, 2024. www.gpli.info. 5. Bennett ES. GP and custom soft annual report. Cont Lens Spectrum. 2023;38(10):24-31. 6. Benoit D, Ames K. Diagnostic versus empirical fitting. Cont Lens Spec. 2010;25(4):12-3. 7. Michaud L, Barriault C, Dionne A, Karwatsky P. Empirical fitting of soft or rigid gas-permeable contact lenses for the correction of moderate to severe refractive astigmatism: a comparative study. Optometry. 2009;80(7):375-83. 8. Davis RL, Eiden SB, Bennett ES, et al. Stabilizing myopia by accelerating reshaping technique (SMART) study: three year outcomes and overview. Adv Ophthalmol Vis Sci. 2015;2(3):92-8. 9. DeNaeyer G, Sanders DR, van der Worp E, Jedlicka J, et al. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer: The SSSG Study. J Cont Lens Res Sci. 2017;1:12-22. |


