 |
Despite a wave of advances that have greatly improved our capabilities at disease diagnosis and management, patients continue to present to clinical practices with challenging corneal conditions. Practitioners are fortunate to have options like specialty soft contact lenses, small-diameter gas permeable lenses and hybrids to treat these cases—increasing the ranks of our contact lens patients while helping to improve corneal health for many.
In the spirit of this month’s issue focusing on scleral lenses, Practice Progress will review a few key improvements to scleral lens options that exist today. This knowledge is critical for contact lens practitioners to be able to provide adequate vision to those who need our services the most. We have always felt that the best strategies involve identifying unmet needs in our patient base and then providing them the services they need.
The following three-step procedure is suitable for practitioners who are either neophyte scleral lens fitters or those who have begun to fit sclerals and wish to increase their confidence levels with this specialty design.
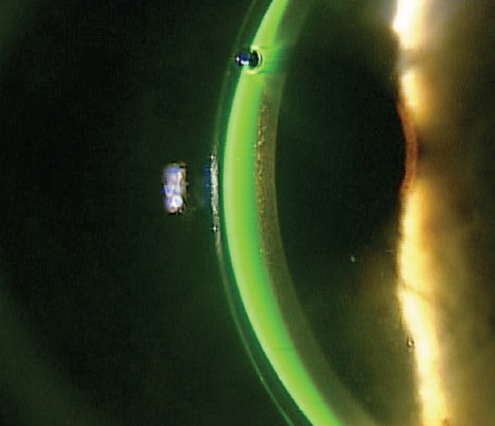 | |
| Fig. 1. Excessive clearance is noted. The contact lens thickness is about 350μm. The fluorescein seen between the lens and the cornea is about three times the thickness of the contact lens, which makes the lens clearance over 1,000μm. |
Low-tech Lessons
There are a number of new designs available that help us more successfully fit scleral lenses. For example: practitioners can order toric scleral landing zones, and some manufacturers even make their diagnostic lenses with this technology. Additionally, a number of scleral lenses have incorporated reverse geometry into their design to adequately clear the limbal corneal area while not excessively vaulting the central cornea. Multifocal scleral lenses are also available for presbyopic patients.
Regardless of these advancements, there are still three primary fitting rules to keep in mind:
1. Make sure the scleral lens clears the central cornea. Simultaneously, we also need to keep in mind that the non-preserved saline used to fill the bowl of the lens has a resistance to oxygen permeability. As such, we want to balance the appropriate scleral lens clearance with avoiding the provision of excessive resistance to oxygen permeability. The generally accepted that the goal of central corneal clearance is between 100μm and 300μm.1 Of course, in some of our more irregular cornea patients, it may be impossible to obtain clearance of this level across the entire cornea, but still—keep these clearance levels in mind when fitting scleral lenses, and attempt to meet this target as much as possible (Figure 1).
2. Respect the limbal region of the cornea. This is where the limbal stem cells of the cornea are located and, when fitting scleral lenses, this area must be cleared. When filling the bowl of the lens with non-preserved saline prior to installation, we can also add fluorescein to the bowl to help identify a level of clearance. Using the slit lamp to observe an optic cross section through any portion of the lens, practitioners can identify the level of clearance by examining the presence of fluorescein between the lens and cornea. Additionally, looking at the lens using a wide beam can help determine whether fluorescein is visible at the limbal area of the cornea: if none is seen between the lens and the cornea in the limbal region, then the limbal zone of the lens should be steepened to provide additional clearance (Figure 2).
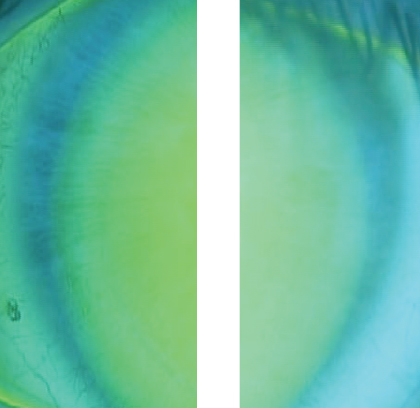 | |
Fig. 2. This is a view of the nasal and temporal areas of a scleral lens on the eye. There is no fluorescein present in these areas, representing the lens compressing that area. | |
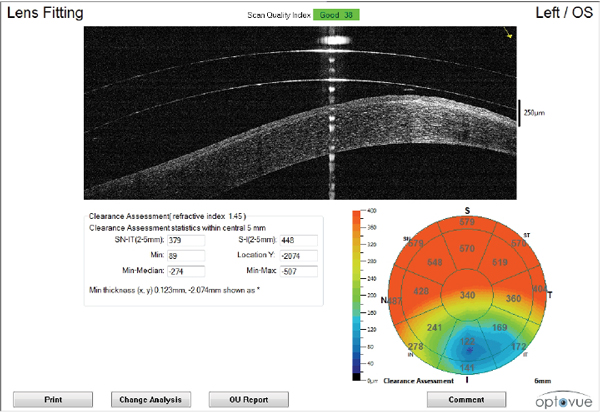 | |
Fig. 3. This is a new software application that allows the clearance of the central 6mm to be seen in one report. The top of the report shows a vertical cross section through the lens and the cornea, while the bottom right side of the report shows the clearance map. Note that the clearance is significantly less in the inferior temporal aspect of the map. |
3. Monitor the scleral landing zone. Ideally, the scleral lens bearing area should mimic the curve of the sclera and overlying conjunctiva to lie flat on the tissue. When the landing zone profile is steeper than the sclera, impingement of the conjunctival tissue will occur, requiring that the lens be flattened; when the landing zone profile is flatter than the sclera, compression in the proximal portion of the scleral landing zone can occur, necessitating that the lens be steepened instead.
High-tech Help
If faced with a more complex case, practitioners can also consider incorporating new advances into their fitting process. There have been numerous developments in scleral lens designs, and technology continues to support lens fit efforts. For example, one of the most widely used devices in the area of scleral lens fitting is optical coheren
ce tomography (OCT), which gives us greater precision in determining sagittal height and the anatomical structure of the peripheral cornea and sclera for better lens edge design.
OCT technologies now exist that are capable of capturing a central 6mm radius circle in the center of the cornea. This can now be applied to scleral lenses that are on eye, allowing practitioners to visualize the clearance of the lens over the cornea. For years, we have had the ability to manually measure clearance: the examiner would identify the anterior surface of the cornea and posterior surface of the lens, then use software measurement tools to identify the clearance. Now, software on the OCT can provide a global 6mm diameter view of the clearance of the lens over the cornea in one scan (Figure 3). This provides the examiner with a clearer view of the variation in clearance throughout the central 6mm of the cornea under the lens.
Practitioners wishing for more experience with the fitting process outside of the clinic may want to attend a workshop or find a mentor. Live scleral fitting workshops can provide significant experience and insights from experts; often attendees are given the opportunity to fit patients with help from some of the best in the industry. It is also important to have someone available for consultation and mentorship as you continue to gain fitting experience. Many GP lens manufacturers have phenomenal consultation departments to provide help during the fitting process.
Scleral lenses have offered a number of patients clear, comfortable vision that they would otherwise not be able to attain. Taking into account these three strategies will help practitioners set themselves up for success when fitting this lens modality.
1. van der Worp E. A Guide to Scleral Lens Fitting [monograph online]. Forest Grove, OR: Pacific University; 2010. Available at: commons.pacificu.edu/mono/4/.


