Extended contact lens wear has long been thought to be the most desirable modality for our patients because it offers great convenience, uninterrupted good vision and suits those with an active lifestyle.1 Despite these benefits, extended wear is not prescribed with any frequency in the United States—at least not since the late 1980s, when researchers found a much higher incidence of ulcerative keratitis with this modality compared with daily wear.2
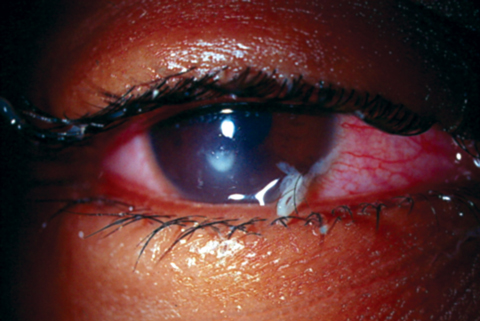 |
| This extended wear patient developed culture-proven Pseudomonas keratitis that has mucopurulent discharge. Photo: Joseph Sowka, OD, and Alan G. Kabat, OD |
Currently, only about 5% of new fits in the United States are extended wear contact lens prescriptions.1 This has not changed over the last 20 years, with the exception of a brief spike in the early 2000s when Ciba Vision released Focus Night and Day and Bausch + Lomb introduced PureVision—the only two contact lenses on the market FDA-approved for up to 30 nights of continuous wear. With these came the term continuous wear to distinguish it from extended wear (30 days vs. seven days).1 For the purposes of this article, we will refer to any overnight wear as extended wear.
While a few extended wear contact lens options remain on the market, many uncertainties hinder their use, including concerns that not enough oxygen passes through the lens to support a healthy cornea or that a toxic tear film exists beneath a contact lens that needs to be flushed by removing the lens. In addition, a practitioner’s history of contact lens patients with microbial keratitis (MK) or inflammation may lead them to prescribe a more limited wearing time.
This article takes a look at extended wear today, how advances have improved the modality and what questions remain.
Let the Ocular Surface Breathe
With contact lens wear, oxygen reaches the cornea both by diffusing through the lens material and mixing with the tears, thereby getting around and beneath the lens. Many studies have looked at the oxygen needs of a healthy cornea, and today’s contact lens materials, FDA-approved for extended wear, meet those requirements (Dk/t of 125 x 10-9) according to the widely accepted, relatively straightforward calculation of Dk/t.3-5 The new high Dk silicone hydrogel lens material used for extended wear contact lenses provides several benefits, such as:
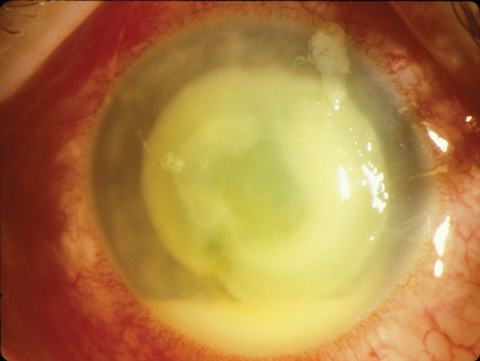 |
| This extended wear patient presented with a large hypopyon ulcer (Pseudomonas cultured). Photo: William D. Townsend, OD |
• Reduced incidences of endothelial polymegethism, which occurred as a result of chronic hypoxia with hydrogel lenses.3
• Only rare instances of vascular changes (i.e., limbal hyperemia and neovascularization) commonly seen in hydrogel lenses worn on an extended wear basis.3
• No more myopic shifts, once observed when changing patients from hydrogel to silicone hydrogel materials—presumed to result from chronic hypoxia.3
Although research has yet to identify the actual amount of oxygen diffusing into the cornea underneath a contact lens, investigators suggest it may be an alternate means for evaluating contact lens performance.3 Further research may help to reveal the rate of oxygen consumption of the cornea, and thus help clinicians to properly evaluate contact lens performance and the impact of extended wear.
Cornea metabolism is also affected by contact lens wear. Epithelial cells originate at the limbus and travel across the cornea before sloughing off at the ocular surface—a process that might be affected by covering the cornea with a contact lens, possibly inducing hypoxia. When measuring basal epithelial cell proliferation in extended wear contact lens patients, researchers found that oxygen transmissibility of the contact lens material does make a difference with chronic hypoxia, causing a decrease in the metabolic activity of the corneal epithelium and decreased epithelial oxygen consumption. These changes negatively impact normal epithelial growth.6 Research also shows epithelial thinning and conjunctival hyperemia in extended wear patients, possibly due to alterations in proliferation or exfoliation, which was exaggerated in patients wearing lower Dk materials.6 Such epithelial thinning due to decreased metabolism might make it prone to infection.6
However, Dk/t is only a physical measurement and does not incorporate any physiological component, such as changes due to trapped debris behind a lens worn overnight in a warm environment (e.g., a closed eyelid traps heat from the eye), which is more conducive to bacterial growth.
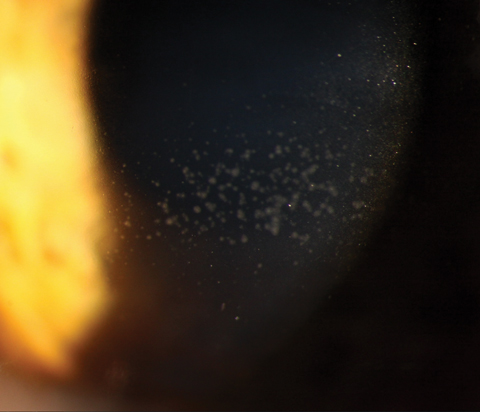 |
| Mucin balls, as seen here, are a typical finding under extended wear contact lenses. Photo: Christine W. Sindt, OD |
Ward Off Inflammation
Researchers know that any contact lens on the eye initiates an inflammatory response, and extended wear options are no different.7 Even with daily disposable contact lens wearers, clinicians sometimes see evidence of a prior inflammatory event on slit lamp examination, such as subepithelial infiltrate scars, despite the patient denying any clinical event. Studies have yet to uncover whether extended contact lens wear moves the inflammatory response from subclinical to clinical with a statistical difference over daily contact lens wear.
What researchers do know is that corneal erosions—another potential risk for infection—are more likely to occur during extended wear.8 Overnight, the posterior lens surface adheres to the epithelium; upon awakening and the resumption of blinking, an epithelial disruption is more likely, removing the barrier to bacteria and increasing the risk of an infection.9
Hypoxia during extended wear also leads to increased binding of bacteria to corneal epithelial cells. Soft contact lens wear significantly increases the amount of binding relative to baseline (no contact lens use), and this binding only increases with extended wear, leading to an increased risk of infection.10
MK is the most serious complication of contact lens wear, and while the prevalence is low in the United States, it is still an ocular emergency.11 Immediate treatment is crucial to minimize the overall size and depth of the ulcer and the inevitable scarring.11 The greatest risk factor for MK is overnight lens wear—a risk that is similar for both hydrogel and silicone hydrogel lenses.12
In the United States, contact lens use and misuse—including overnight wear—accounts for 19% to 42% of culture-proven MK.13 However, only a small number of those patients were prescribed lenses as extended wear, leading researchers to believe the oxygen permeability of most contact lenses is sufficient to prevent contact lens-related issues.13,14 Thus, in most cases, complications such as MK must be caused by some other factor, such as entrapped debris, mechanical irritation or drying of the lens and eye, for example.
Other inflammatory events negatively impact contact lens wear and can be a particular concern for extended wear users:
Contact lens-associated red eye is typically caused by a unilateral acute inflammation as a result of endotoxins—heat-stable toxins associated with the outer membranes of certain gram-negative bacteria—and often occurs in patients suffering from upper respiratory infections.7
Contact lens peripheral ulcer is typically due to an inflammation caused by a hypersensitivity reaction to the endotoxins of gram-positive bacteria. These sterile ulcers usually scar and have the potential to negatively affect best-corrected visual acuity even after the acute inflammation is gone.
Despite the widespread thought—by patients and even the government—that contact lenses are a commodity and not a medical device, it is imperative doctors address contact lens wearing schedule, handling and care. A patient’s compliance with contact lens wear and care is a crucial factor when prescribing contact lenses. Proper patient education and early detection can prevent most of these events from becoming sight-threatening problems.15
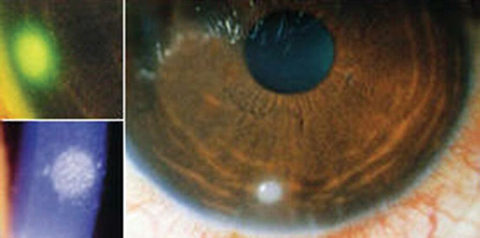 |
| Management of an acute contact lens peripheral ulcer, as seen here, requires only temporary discontinuation of lens wear until all signs of inflammation are resolved. Photo: Clark Chang, OD, MSA, MSc |
The Eye’s Environment
The contents found naturally in tears, in addition to what the eye has been exposed to during the day—which can dissolve or became entrapped in the tear film under a contact lens—are huge factors to consider with contact lens wear.
The tear film is full of potential inflammatory stimulants, including lipids, proteins and mucin, exfoliated cornea epithelial cells, byproducts of corneal metabolism and chronic blepharitis, to name a few. In addition, exposure to a smoky or toxic environment can initiate any number of ocular side effects that can complicate contact lens wear. The eye’s ability to respond to any of these factors may be affected by the individual’s genetics, the wearing schedule and contact lens material.7
Contact lens wear changes the natural flow of tears across the corneal epithelium. It also hinders the mechanical effect of blinking to clear toxins.8 Tears are even more stagnant with extended lens wear, further increasing the exposure of these potential toxins to the cornea. Research suggests mucin balls, which are typically seen under extended wear lenses, might act as protective agents. They were once thought to be innocuous, but some research now suggests they are protective against inflammatory events, as they appear to form due to corneal surface irregularity and might help to smooth out the cornea and activate keratocytes.16,17
Indications for Extended Wear
Other factors to consider when choosing the right contact lens modality are the patient’s ocular and systemic medical conditions that might impact their contact lens use. While extended wear is necessary for bandage lenses in patients with corneal abrasions, bullous keratopathy and keratoprostheses, these patients are often prescribed antibiotics and anti-inflammatory drops while wearing the lenses. Contraindications to extended contact lens wear include patients with collagen vascular diseases and diabetes, for example.
| Extended Wear of the Future Many companies are even looking at contact lenses to project a televised image directly to your retina for a larger-than-life virtual reality experience or to aid as a reflecting telescopic for our low vision patients.4 All of these advances, particularly those used for health monitoring, might lead to more extended wear of contact lenses and will demand rigorous patient education to ensure they stay safe in contact lens wear. 1. Yao H, Shum AJ, Cowan M, et al. A contact lens with embedded sensor for monitoring tear glucose level. Biosensors and Bioelectronics. 2011;26(7):3290-6. |
Over the past decade, overnight orthokeratology has been renewing the discussion on the safety of extended wear, particularly with pediatric patients. Even though extended wear is generally thought to be a safe modality, MK continues to be a concern in this population.18 Poor lens hygiene and noncompliance with cleaning regimens are risk factors for Acanthamoeba keratitis, for example, especially in pediatric patients caring for their own lenses.18 To keep this a safe modality, clinicians must overemphasize the wearing and cleaning regimens with patients and their parents.
Unanswered Questions
Research has yet to reveal whether a difference in inflammation or infection rates exists for patients who are prescribed extended wear lenses vs. those who choose this modality without a prescription. A better understanding of the impact of patient education on extended contact lens wear will help clinicians to avoid negative outcomes. Inflammatory events are common in contact lens wearers—and research shows these events are more likely in extended wear patients—but it is unclear whether an increase in inflammatory mediators in the tear film while sleeping is the only cause. Future studies are needed to explore patients’ possible genetic predisposition to inflammation, as well as affordable in-office tests for genetics, goblet cell density and antigen-presenting cells. A better understanding of specific environmental factors that make extended wear an impossibility for at-risk patients would also help clinicians with patient selection. Some contact lens wearers are perpetually noncompliant and wear their lenses continuously without any negative events—these patients may be the key to understanding who can and cannot tolerate extended wear due to their genetic makeup.
Most clinicians know their patients would prefer extended wear contact lenses. To help make that desire a reality while maintaining safe contact lens wear, we must further the research. Worldwide, contact lenses are a multi-billion dollar industry—we should harness some of that money to continue to research ways of determining what makes some patients excellent contact lens wearers with no or minimal complications.
Dr. Kaplan has been teaching contact lenses to optometry students at SUNY College of Optometry and ophthalmology residents at NY Eye and Ear Infirmary for over 25 years. After graduating from Washington University in St. Louis, he completed his optometry degree from SUNY College of Optometry. Dr. Kaplan continued studying at SUNY to earn a master’s degree in vision science and complete his fellowship in cornea and contact lenses. Additionally, he is the co-owner of two group optometry practices in New York City.
1. Morgan PB, Efron N, Helland M, et al. Global trends in prescribing contact lenses for extended wear. Cont Lens Ant Eye. 2011;34(1):32-5. |


