 |
An 81-year-old male presented with a 60-year history of aphakia OU secondary to idiopathic crystalline lens dislocations. He was referred over concerns about corneal edema and whether he should discontinue wear of his gas permeable (GP) contact lenses.
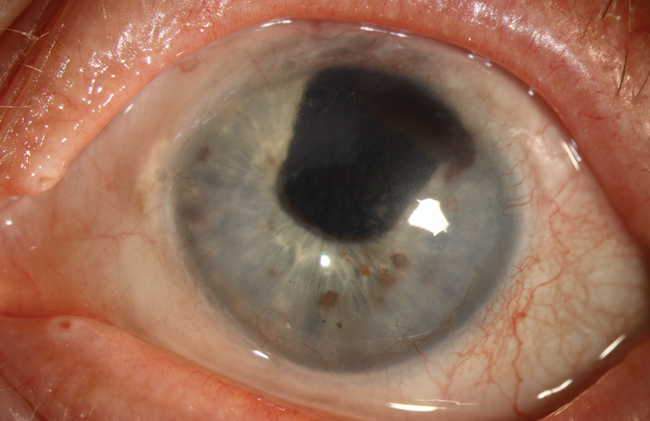
Slit lamp exam showed posterior crocodile shagreen centrally with microcystic edema 360 degrees in the periphery with 2mm of peripheral neovascularization, consistent with Brown-McLean syndrome (BMS). This condition is typically observed after intracapsular cataract surgery, but has also been reported in extracap procedures with phaco, pars plana lensectomy/vitrectomy and Marfan’s syndrome with lens subluxation.
While the exact etiology of BMS is unknown, it is generally benign and rarely affects vision. Stromal/microcystic edema is seen in the peripheral 2mm to 3mm of the cornea with orange or brown deposits at the level of Descemet’s membrane.1 The edema often begins inferiorly and spreads circumferentially. In some cases, the patient will present with a foreign body sensation or bullae, which can be treated with lubrication or hyperosmotics.
Central posterior crocodile shagreen is believed to be a primary degenerative process involving rearrangement of the posterior stromal lamellae.2
Brown-McLean syndrome is not a contraindication to contact lens wear. The high oxygen transmissibility of GP materials is favorable over soft lenses in this case, given the propensity for edema formation. The patient was advised to continue GP lens wear and instructed to alert the clinic of any untoward events or discomfort.
1. Gothard TW, Hardten DR, Lane SS, et al. Clinical findings in Brown-McLean syndrome. Am J Ophthalmol. 1993 June 15;115(6):729-37.
2. Belliveau MJ, Brownstein S, Agapitos P, Font RL. Ultrastructural features of posterior crocodile shagreen of the cornea. Surv Ophthalmol. 2009 Sep-Oct;54(5):569-75.
 |


