 |
A 47-year-old female presents complaining of mild discomfort while wearing her contact lenses. A comprehensive ocular examination reveals no physiological basis for the discomfort, as the ocular surface appears normal.
In this case, many of us may try to alleviate the discomfort using a new lens material, solution or even a daily disposable lens. These technologies may make the patient comfortable for now, but will she return in a year and report more discomfort? And if she does, should she be re-fit again, or is there an underlying cause that needs to be treated first?
The Great Population Shift
The rapid decline in the number of contact lens wearers is no coincidence—our population is aging, and the prevalence of dry eye increases proportionally with age. Studies have found the prevalence of dry eye to be 3.5% to 33%, depending on the criteria used for inclusion and the age of the population studied.1-5
With any number of endogenous factors contributing to alterations in the ocular surface, simply changing the contact lenses, solutions and designs won’t necessarily address the underlying factor(s) responsible for the decreasing comfort of the lenses.
In other words, the examination of the patient above revealed no ocular abnormalities—but does that necessarily mean the ocular surface is functioning normally?
The Meibomian Glands
The meibomian glands produce the lipid layer of the tear film that acts to prevent evaporation of the underlying aqueous layer. A robust lipid layer is critical for a healthy tear film, so the meibomian glands need to be functioning properly. In a healthy individual, the meibum has a melting point between 660°F and 890°F, meaning it exists in a fluid state at normal body temperature (98.60°F).6
| |
|
|
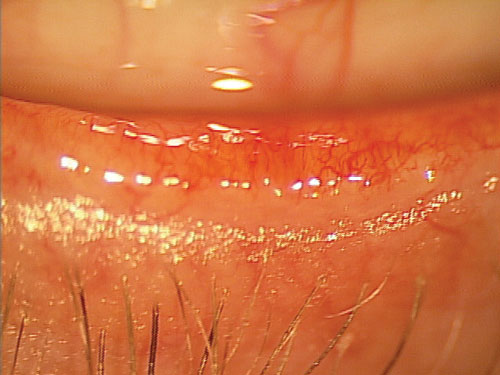
Fig. 1. Lower eyelid of a patient with obvious meibomian gland dysfunction. |

| |
|
|
Fig. 2. Lower eyelid of a patient wearing makeup with non-obvious meibomian gland dysfunction. |
Traditional thinking on meibomian gland dysfunction (MGD) suggests that a deficiency in the glands is accompanied by inflammation of the eyelid margins, visible capping of the gland orifices and generalized conjunctival injection. There are two types of meibomian gland dysfunction: obvious MGD and non-obvious MGD. The obvious form is the scenario just described. Non-obvious MGD, on the other hand, is not characterized by visible inflammation. Rather, the glands look normal, but the meibum is of abnormal consistency when expressed.7 The meibum may be completely stagnant—application of pressure yields no visible meibum—or abnormally thickened, instead of fluid as expected.
The clinical challenge here is that non-obvious MGD, as the name implies, is elusive. Often, the lid margin appears normal. Only upon attempted expression would the clinician notice any abnormalities in gland function; unfortunately, if gland expression is not attempted, there will be no obvious reason to consider MGD treatment.
In light of this, think about attempting gland expression at every visit, regardless of whether the patient is exhibiting dry eye symptoms. This is the only way to determine for sure whether the meibum is in fact being expressed properly from the gland.
Most examiners can easily perform this by applying gentle pressure along the eyelid margin and visualizing the meibum that is expressed. Certain specialized tools can also assist with this procedure, such as the meibomian gland expressor (MGE), a device that applies pressure to the lid margin similar to the amount placed by the eyelids during a normal blink. This allows for an assessment of the meibum released from the glands under the pressure of a normal blink. Additionally, meibography allows the examiner to view the meibomian glands to determine abnormalities in structure that may exist in symptomatic patients.
Non-Obvious MGD Diagnosis—Now What?
Once the diagnosis has been made, it is important to educate the patient on the cause of the decreased comfort and your plan: to increase functionality of the glands by producing meibum that is more fluid in nature. Often, this will require sustained heat to the eyes. A number of eyelid heating systems are available, such as the Tranquileyes goggles from Ocusoft and moist heat compresses from Bruder.8,9
Recommended application time varies; many practitioners suggest 10 minutes at a time, twice a day.
Ocular nutrition has also become important in helping normalize the tear film in those with MGD.10,11 Omega-3 fatty acids in particular have been shown to decrease ocular surface inflammation.12-14 Evening primrose oil, green tea extract and vitamin A have also been demonstrated to improve and maintain ocular surface health.15-17
Other contemporary treatments include Lipiflow, a technology that distributes heat to the meibomian glands via the tarsal surface while providing pressure to the anterior surface of the eyelids to help renormalize the meibum secreted from the glands.18 A similar device is the MiBoFlo Thermoflo.
All of these strategies, while varied in application, are geared towards renormalizing the patient’s tear film to improve the environment the lens is placed into. By following this process, we will have the best chance of preserving the wearing experience in individuals who are finding their lenses to be increasingly uncomfortable.
Back To The Patient At Hand
So, how do we handle the patient in question? First, we need to determine whether the patient’s meibomian glands are in fact producing quality meibum. As said before, this requires gentle pressure to determine the quality of the meibum. In this patient, it was evident that there was very little meibum expressed from the glands—in fact, significant pressure was needed to express any meibum at all.
The patient was started on a regular regimen of heat applied to the eyelids in the morning and evening for 10 minutes per session, as well as an ocular nutraceutical that contained multiple ingredients to help with dry eye. She was also given a lipid-based artificial tear to use before inserting her contact lenses and then as needed throughout the day.
Of course, it’s important to remember treating non-obvious MGD is only one way to improve lens wear. Always be sure to try a multi-faceted approach—the use of daily disposable lenses, a change in solutions and experimentation with different new materials can also enhance a patient’s wearing experience.
1. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264-8.
2. McCarty CA, Bansal AK, Livingston PM, et al. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998;105:1114-9.
3. Schein OD, Munoz B, Tielsch JM, et al. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723-8.
4. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003 Aug; 136(2): 318-26.
5. Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405-12.
6. Abelson MB, Oberoi S. Treating Dysfunctional Meibomian Glands. Review of Ophthalmology, Vol. No: 13:08. 2006
7. Blackie CA, Korb DR, Knop E, et al. Nonobvious obstructive meibomian gland dysfunction. Cornea. 2010 Dec;29(12):1333-45.
8. www.ocusoft.com/SearchResults.aspx?q=tranquileyes
9. http://www.bruder.com/eye/products/
10. Roncone M, Bartlett H, Eperjesi F. Essential fatty acids for dry eye: A review. Cont Lens Anterior Eye. 2010 Apr;33(2):49-54.
11. Rosenberg ES, Asbell PA. Essential fatty acids in the treatment of dry eye. Ocul Surf. 2010 Jan;8(1):18-28.
12. Miljanović B, Trivedi KA, Dana MR, et al. Relation between dietary n-3 and n-6 fatty acids and clinically diagnosed dry eye syndrome in women. Am J Clin Nutr. 2005 Oct;82(4):887-93.
13. Pinazo-Durán MD, Galbis-Estrada C, Pons-Vázquez S, et al. Effects of a nutraceutical formulation based on the combination of antioxidants and omega-3 essential fatty acids in the expression of inflammation and immune response mediators in tears from patients with dry eye disorders. Clin Interv Aging. 2013;8:139-48.
14. Brignole-Baudouin F, Baudouin C, Aragona P, et al. A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients. Acta Ophthalmol. 2011 Nov;89(7):591-7.
15. Sheppard JD Jr, Singh R, McClellan AJ, et al. Long-term Supplementation With n-6 and n-3 PUFAs Improves Moderate-to-Severe Keratoconjunctivitis Sicca: A Randomized Double-Blind Clinical Trial. Cornea. 2013 Jul 23.
16. Cavet ME, Harrington KL, Vollmer TR, et al. Anti-inflammatory and anti-oxidative effects of the green tea polyphenol epigallocatechin gallate in human corneal epithelial cells. Mol Vis. 2011 Feb 18;17:533-42.
17. Kheir AE1, Dirar TO, Elhassan HO, et al. Xerophthalmia in a traditional Quran boarding school in Sudan. Middle East Afr J Ophthalmol. 2012 Apr-Jun;19(2):190-3.
18. Lane SS, DuBiner HB, Epstein RJ, et al. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea. 2012 Apr;31(4):396-404.


