Many patients prefer to wear contact lenses over glasses because they provide a more natural experience and correct refractive error without covering the eyes. A survey conducted in the United Kingdom found that the top reasons for wearing contact lenses were freedom and self-confidence.1 In another study, 80% of consumers agreed that wearing contact lenses makes them feel more confident.2 This indicates that, despite practical applications, aesthetics are king.
 |
| Fig. 1. Patient with eyelash extensions and blepharitis. Click image to enlarge. |
Dryness and Discomfort
Usually, if the contact lens is well-fitting, patients can barely feel it. However, in those affected by dry eye disease (DED), contact lens wear can become uncomfortable. As many as 36% of new contact lens wearers drop out of lens wear due to discomfort.3 A survey conducted by the University of Waterloo included 1,444 contact lens dropouts and found that the primary reasons cited for discontinuation were discomfort, dryness and red eyes.4
Changing the contact lens material, design and fitting characteristics will only improve patient comfort to a certain degree. Patient success with contact lens wear is actually hinged on identifying and appropriately treating blepharitis and the ocular surface.
COVID-19 forced meetings that were once face-to-face into the virtual space of Zoom. Many people were stuck at home with little else to do but use electronic devices. This created another “epidemic” of exponentially more prevalent DED.
Now that the world has somewhat returned to normal, patients are wanting to wear their contact lenses more consistently. Many have discovered that their use of screens during the last few years has aggravated their dry eye and made them far less tolerant of contact lens wear.
So, how do we keep our patients in their lenses? It starts with taking a good look at the ocular surface.
 |
Fig. 2. Patient with incomplete lid closure due to lower lid retraction. Click image to enlarge. |
Examination
When a contact lens wearer has dry eye complaints, it may be tempting to assume it is simply the contact lens and refit them into the latest technology.
Start by implementing a dry eye questionnaire for all your contact lens wearers. Questionnaires like the Standard Patient Evaluation of Eye Dryness (SPEED), Ocular Surface Disease Index (OSDI), Dry Eye Questionnaire (DEQ) and Contact Lens Dry Eye Questionnaire (CLDEQ) can help gauge symptom severity and establish a good baseline. The scores can also guide your technician on the need for extra testing, which can help with clinic flow, efficiency and profitability.
One of the major culprits of dry eye is systemic medication use. Unfortunately, some of the most commonly used drugs are the biggest offenders. Oral contraceptives, antihistamines and antidepressants are major contributors. While patients may not be able to modify their drug therapies, we can manage expectations and adjust our DED treatments to better accommodate any aggravating factors.
A thorough dry eye evaluation can add very little time to your exam especially if you know what to look for before you begin. With Demodex present in roughly 58% of dry eye patients and meibomian gland dysfunction (MGD) present in 86%, a close look at the eyelids is a critical starting point in all your contact lens patients.5,6 Figure 1 shows a patient with eyelash extensions and blepharitis.
Start your exam with the patient’s eyelids closed to look for lagophthalmos and floppy eyelid syndrome, which will elicit symptoms of morning dryness. Figure 2 shows a patient with incomplete lid closure due to lower lid retraction. In addition, a subtle finding that can lead to patient discomfort is incomplete blinking. Without prompting your patient to blink, observe their blink pattern as you proceed through the exam.
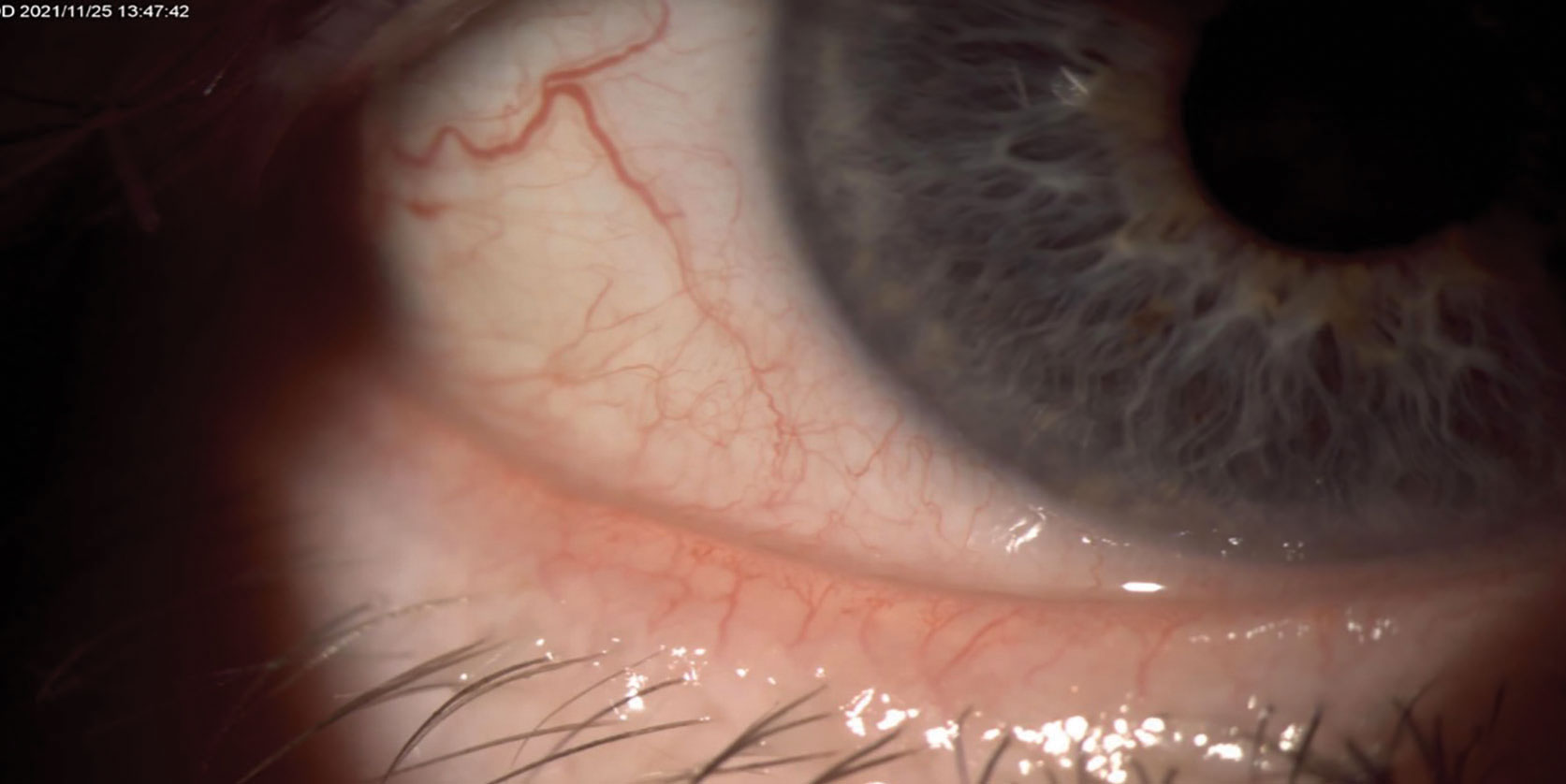 |
Fig. 3. Patient with ocular rosacea and eye telangiectasia contributing to MGD. Click image to enlarge. |
Next, examine the lashes for the presence of debris/biofilm indicating staphylococcal blepharitis and/or collarettes, which are pathognomonic for Demodex. With the patient’s eyes open, scan the lid margin looking for eyelid telangiectasia and MGD. Consider pushing on the lids to observe the meibum that excretes. MGD leads to poor meibum quality and production, causing tear film instability. This also contributes to the inflammatory cycle of DED and inevitably leads to contact lens intolerance and dropout. Figures 3 and 4 show a patient with MGD.
Vital dye testing is an inexpensive way to gain valuable information. Sodium fluorescein will highlight damaged corneal cells, and lissamine green penetrates damaged conjunctival cells to stain the nucleus.7 These tests are important to conduct on all your contact lens patients. Also, use the dye to detect the potential occurrence of an imprint of the lens on the conjunctiva, indicating a poor-fitting lens.
Eyelid eversions are beneficial to look for papillary reactions and lid wiper epitheliopathy that may lead to contact lens intolerance. Examination of the cornea for staining, scarring, neovascularization or active inflammation can provide insight into previous lens wear habits or ocular surface conditions and guide lens material selection and patient education to maximize compliance.
Common conjunctival conditions can also play a role and compound dry eye. Studies have demonstrated normal tear secretion but decreased tear breakup time (TBUT) with pingueculae.8 TBUT was also substantially increased after a single excision.8 This highlights the potentially significant impact of pingueculae on tear film stability and its underestimated role in dry eye.8
Carefully looking for additional aggravating factors like conjunctivochalasis is also important. These structural changes alter tear coverage and can create an environment that is ripe for swelling and irritation with increased friction from DED.
Advanced testing like MMP-9, tear osmolarity and meibography can help further guide treatment and are important tools for patient education and buy-in.
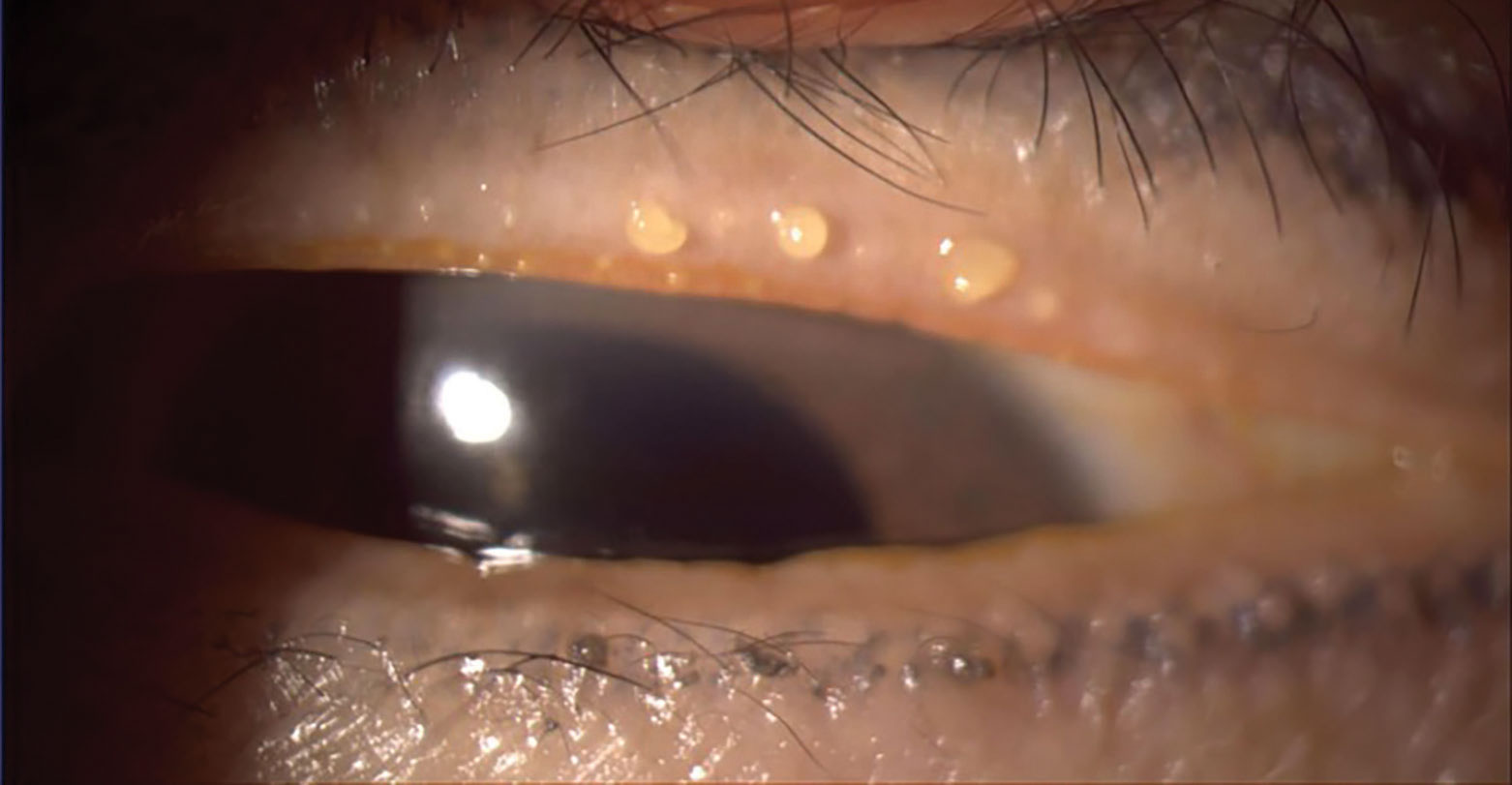 |
Fig. 4. Patient with poor meibum, resulting in MGD. Click image to enlarge. |
Treatment
By the time your patient presents, they will have likely already tried over-the-counter artificial tears. For mild cases, this may suffice; however addressing the root cause will result in better outcomes. Even when your contact lens patients tell you everything is fine, often they are far from it. Interestingly, these patients may ask about alternative options such as refractive surgery. A history of contact lens intolerance may be a predictor of post-LASIK dryness and should be part of the preoperative discussion.9
Noncompliance with contact lens care is common; studies suggest that 40% to 70% of patients fall into this category.10 Healthy contact lens wear depends on many factors, including age, sex, lens brand, smoking habits, cleaning regimen and wear schedule.10 Higher rates of complications were associated with men, youth, smokers, longer periods of wear, a lack of hand washing and internet purchase.10
Noncompliance with the manufacturer’s recommended frequency of replacement of contact lenses is highest among teenagers and non-silicone hydrogel wearers.10
Patients using hydrogen peroxide solutions were found to be more compliant with their contact lens replacement schedule, perhaps because the care regime is more complex and demanding.10 Daily disposables were found to be associated with the lowest rate of complications in general. They also have lower risks for severe contact lens–related microbial keratitis and associated vision loss.10
All patients should be educated on the importance of UV protection to avoid complications associated with such exposure such as pingueculae.8 Contact lens wearers who are dry eye sufferers may especially benefit from such precautions.8
For patients with staphylococcal blepharitis, at-home treatments that target lid hygiene with hypochlorous spray are excellent at removing debris and biofilm. For Demodex blepharitis, lid hygiene that includes tea tree oil has proven beneficial. One particularly exciting drug in the pipeline is TP-03 from Tarsus Pharmaceuticals, which is a treatment for Demodex blepharitis. The active ingredient is lotilaner, which causes paralysis and death of the Demodex mite. The company’s Saturn 1 and 2 data showed a clinically meaningful collarette cure in 89% of patients.11
For patients with lagophthalmos, a simple treatment can be the use of gel tears or ointments at night. For more advanced cases, sleep goggles and/or lid tape can help keep the eye closed while sleeping, alleviating morning dry eye symptoms.
For patients who are more symptomatic or who have moderate levels of MGD, combining in-office treatments with at-home management will lead to better results. In-office blepharoexfoliation, similar to in-office dental lid cleaning, can help. Both automated devices like Blephex and manual options like Zocular Zest can be helpful. Manual expression and debridement can also be used in concert to provide a more comprehensive in-office treatment. More advanced in-office thermal pulsation therapies for MGD include LipiFlow (Johnson + Johnson), iLux (Alcon) and TearCare (Sight Sciences). One study found an improvement in contact lens wear after a single in-office thermal pulsation treatment.12
Intense pulsed light (IPL) therapy for the treatment of MGD is an effective option that produces results patients can see and feel. IPL uses light energy to destroy abnormal telangiectatic blood vessels, which are a reservoir of inflammatory mediators, thus removing a significant source of inflammation from the eyelids and meibomian glands. IPL also helps kill Demodex, soften meibum and improve meibomian gland structure and function over time.13
Rosacea sufferers with associated ocular surface disease are ideal patients for IPL treatment. This does have limitations, however, with only certain skin types meeting the criteria for treatment (Fitzpatrick skin types I through V). Studies suggest combining IPL with lid debridement and meibomian gland expression to create a “force multiplier” and help improve DED symptoms and meibomian gland function.13
Another option to consider in lens wearers is the use of immunomodulators to help reduce inflammation in DED. There are currently four FDA-approved immunomodulators on the market. The BID dosing is convenient, as patients can use these drops before they put their lenses on in the morning and after they remove them at the end of the day. For patients who are not keen on using drops, Tyrvaya (Viatris) nasal spray may be a good option.
Punctal occlusion to increase tear volume may be especially beneficial in contact lens patients. Punctal plugs can help reduce dependency on artificial tears while preserving the patient’s natural tear film and increase the effectiveness of other DED medications by retaining them longer on the ocular surface. One study found that punctal plugs used in conjunction with cyclosporine provided longer symptomatic relief than either treatment on its own.14
Punctal plugs can be a key player in patients who suffer from neurotrophic, aqueous-deficient dry eye or non-resolving persistent epithelial defects, as is the case in patients affected by lagophthalmos.
Before reaching for punctal plugs, though, it is important to manage ocular inflammation first with other methods. Punctal plugs are contraindicated when there are signs of active infection or allergies present. Plugs are also not ideal in patients with blepharitis or meibomianitis, as these patients need management of their lid disease first.
When patients present with moderate to severe dry eyes with significant punctate keratitis, we can turn to blood biologics to help “rescue” and rehabilitate the ocular surface. The two most common drops available in this field are autologous serum and platelet-rich plasma eye drops. Both have been successfully used in the treatment of moderate to severe DED; however, research suggests platelet-rich plasma eye drops are superior in restoring the ocular surface.15 Figure 5 shows preparation of these drops.
When drawing the patient’s blood is not an option, amniotic membranes can also be considered. These come either cryopreserved or dehydrated.
While advanced DED patients may not be able to wear contact lenses full time, appropriately treating the ocular surface will give them the freedom to wear them for certain activities, a gift they will truly appreciate.
 |
Fig. 5. Preparation of platelet-rich plasma eye drops. Click image to enlarge. |
Takeaways
Not addressing ocular surface disease in your contact lens patient can have a domino effect. Cycling through lens after lens eats up valuable chair time, and you are likely losing more contact lens patients than you realize. The number of new contact lens wearers each year is roughly equal to the number of contact lens dropouts despite improved comfort and technology with soft contact lenses, as we now know that contact lens dropout is mainly due to ocular discomfort.16
However, those statistics don’t have to be your outcomes. Being proactive about treating your dry eye patients makes sense as a business strategy and keeps your patients in their contact lenses longer.
Dr. Madan has over 17 years of experience practicing medical optometry and managing dry eye patients. She is the president of BC Doctors of Optometry and a lecturer at Pacific University College of Optometry. She is a consultant for Lumenis, Myedrop, Thea, Labtician, Sun Pharma, Santen and Abbvie.
Dr. Eltis practices in Toronto and teaches at the University of Waterloo. He is president of the College of Optometrists of Ontario and the Canadian Ambassador for the American Board of Optometry. He is a consultant for CooperVision, Sun Pharma, Volk, Heine, Myedrop, Labtician, Thea, Zocular and Aequus Pharmaceuticals.
Dr. Garlich runs a dry eye clinic that she built within her primary eyecare practice, Envision Optometry, in Boston. She is a consultant for Aldyera, Allergan, Bruder, Dompé, Kala Pharmaceuticals, Lumenis, Novartis, Orasis, Oyster Point, SleepTite/SleepRite, Tarsus and Thea Pharmaceuticals.
1. CVI data on file. CooperVision consumer insight study, July 2018. GB adults who wear daily disposable contact lenses: n=279 2. CVI data on file 2020. YouGov Plc online consumer survey Nov/Dec 2019 in Germany, UK, Spain, Japan, USA. N=5,117 Contact Lens wearers (“consumers”), screened from total N=35,397 adults. Data weighted and representative of adults in each market (aged 18+). 3. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-82. 4. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999 Nov;26(6):157-162. 5. Trattler W, Karpecki P, Rapoport Y, Sadri E, Schachter S, Whitley WO, Yeu E. The Prevalence of Demodex Blepharitis in US Eye Care Clinic Patients as Determined by Collarettes: A Pathognomonic Sign. Clin Ophthalmol. 2022 Apr 15;16:1153-1164. 6. Lemp MA, Crews LA, Bron AJ, Foulks GN & Sullivan BD (2012): Distribution of aqueous‐deficient and evaporative dry eye in a clinic‐based patient cohort: a retrospective study. Cornea 31: 472–478. 7. Paugh JR, Tse J, Nguyen T, et al. Efficacy of the fluorescein tear breakup time test in dry eye. Cornea. 2020;39(1):92-8. 8. Eltis M. Pingueculae and Their Clinical Implications. Clin Refract Optom. 2011;22(1):10. 9. Eltis, M. (2022). Refractive Surgery: Part 2. Complications and recent advances. Canadian Journal of Optometry, 84(4), 49–58. 10. Eltis M. Contact-lens-related microbial keratitis: case report and review. J Optom. 2011 Oct;4(4):122–7. 11. Yeu E, Wirta DL, Karpecki P, Baba SN, Holdbook M; Saturn I Study Group. Lotilaner Ophthalmic Solution, 0.25%, for the Treatment of Demodex Blepharitis: Results of a Prospective, Randomized, Vehicle-Controlled, Double-Masked, Pivotal Trial (Saturn-1). Cornea. 2022 Aug 11. 12. Blackie CA, Coleman CA, et al. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clin Ophthalmol. 2018 Jan 17;12:169-183. 13. Kassir R, Kolluru A, Kassir M. Intense pulsed light for the treatment of rosacea and telangiectasias. J Cosmet Laser Ther. 2011;13(5):216-222. 14. Roberts CW, Carniglia PE, Brazzo BG. Comparison of topical cyclosporine, punctal occlusion, and a combination for the treatment of dry eye. Cornea. 2007 Aug;26(7):805-9. 15. Alio JL, Rodriguez AE, Ferreira-Oliveira R, Wróbel-Dudzińska D, Abdelghany AA. Treatment of Dry Eye Disease with Autologous Platelet-Rich Plasma: A Prospective, Interventional, Non-Randomized Study. Ophthalmol Ther. 2017;6(2):285-293. 16. Pucker AD, Tichenor AA. A Review of Contact Lens Dropout. Clin Optom (Auckl). 2020 Jun 25;12:85-94. |


