The standard approach to correcting irregular astigmatism is reaching for a specialty lens design that incorporates gas permeable (GP) optics, whether that be a corneal GP, a piggyback system, a hybrid design or a scleral lens. Each option provides superior optics and visual acuity in cases of corneal irregularity. While these designs might seem like an obvious “go-to” for the practitioner, they may not be the optimal choice for every patient. Perhaps the patient doesn’t like the performance of the lens, they find aspects of the handling/care inconvenient or there are additional barriers at play. Soft contact lenses can be an alternative for select patients, despite the presence of irregular astigmatism. While custom soft lens options exist, often commercially available standard options can suffice, as they come in a wide array of materials and refractive powers.
 |
|
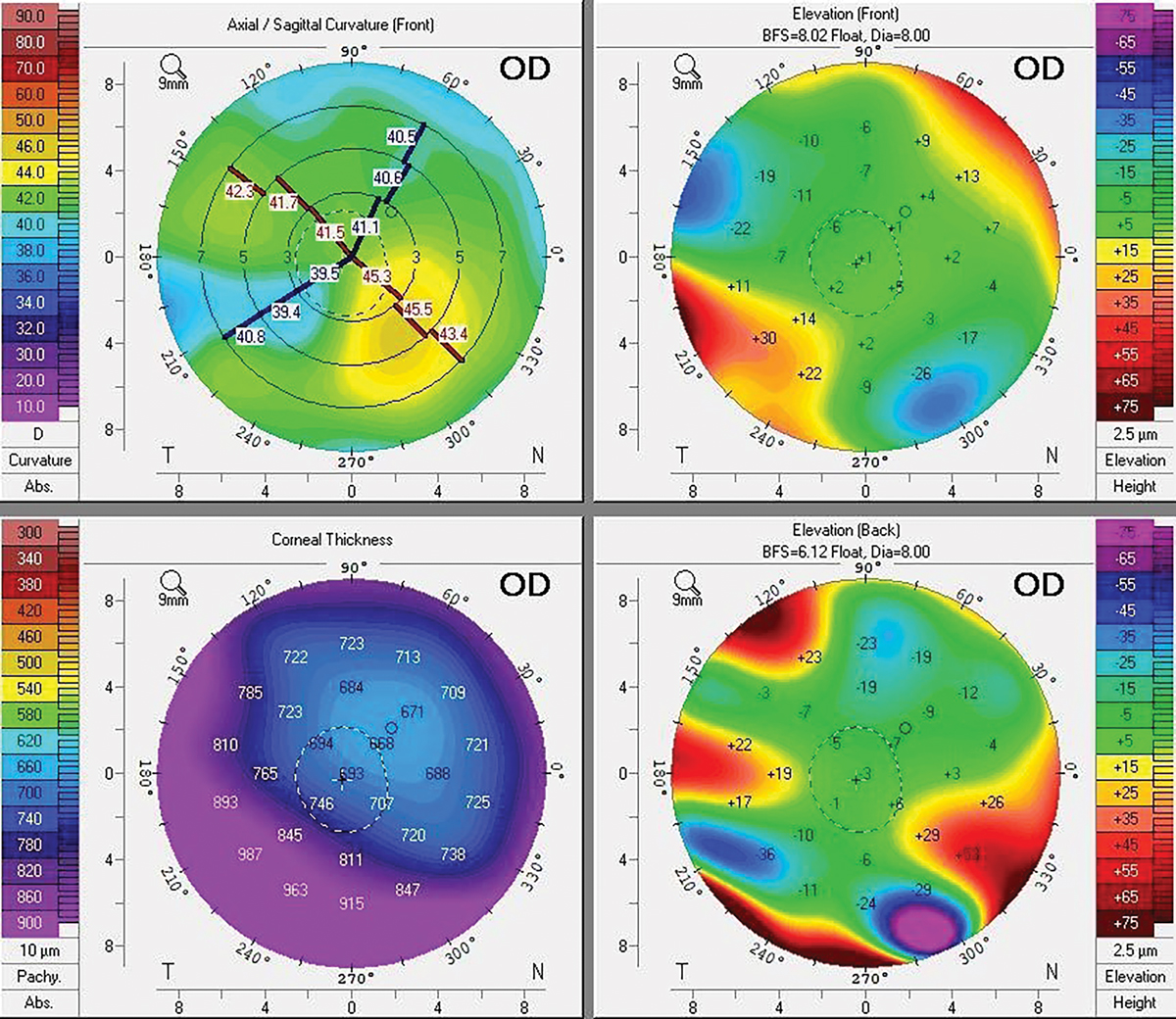
Pentacam of patient in Case #1 with traumatic aphakia. Click image to enlarge. |
The key questions that arise are: (1) when should practitioners opt for a soft lens fitting over a different specialty lens with GP optics, and (2) when is a custom soft lens indicated over a standard design?
How do I know when to choose a soft lens for the irregular cornea?
• Assess the corneal profile. When examining the eye from the side view, is the cornea prolate or oblate? If it’s not too extreme, a soft lens may work out.
• Examine the topography. If there is a mild to moderate level of irregular astigmatism, the chances are better. You also want to focus on the visual axis/pupillary region—if astigmatism is fairly regular in that area, that bodes well for a soft lens design.
• Consider the refraction. If the vision through a new refraction is fairly good (20/40 or better), there is a better chance that vision in a soft lens will be adequate. Conversely, if the refractive result yields poor VA, this option is less likely to markedly improve that acuity.
• Ensure the expectations are realistic. The patient needs to understand what they will realistically receive in terms of comfort, handling and vision.
 |
|
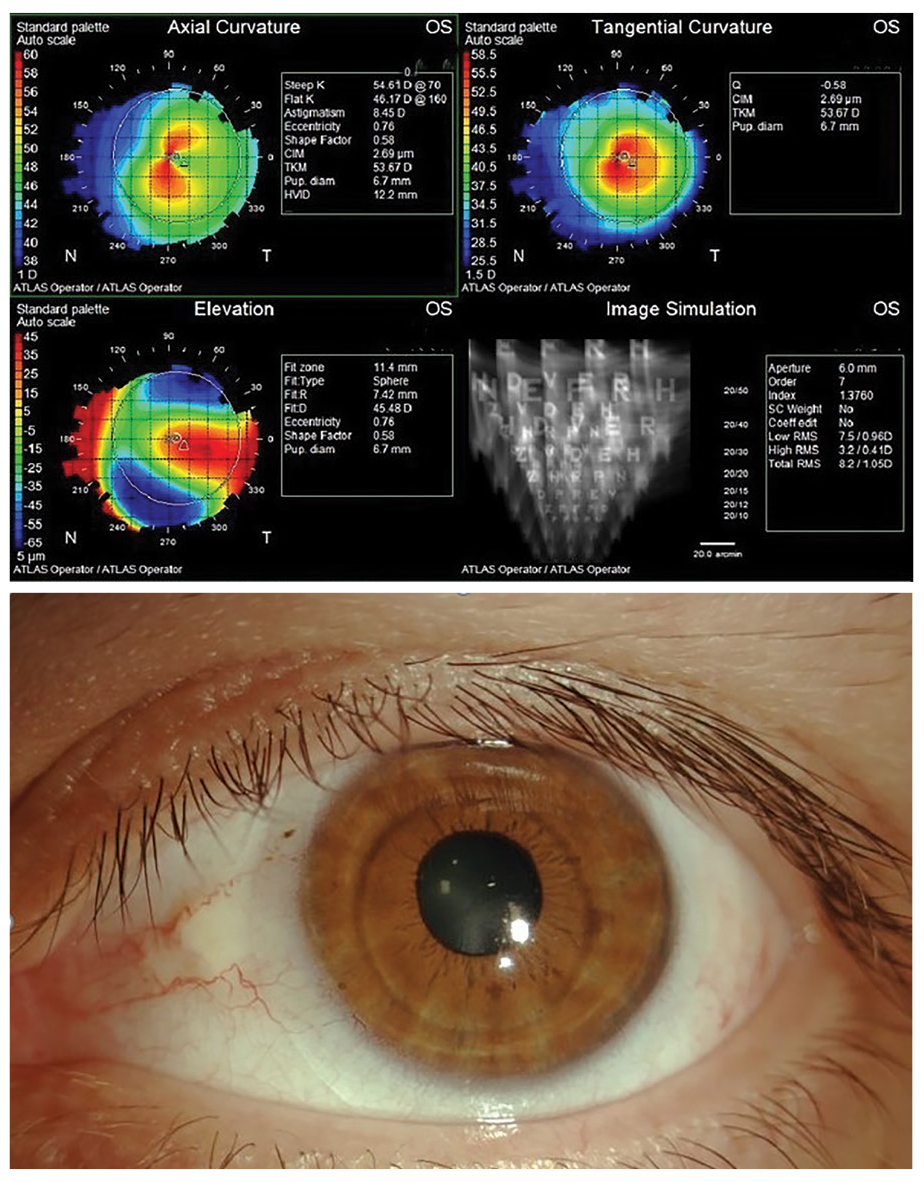
Case #2’s topography map showing skewed radial axes on the axial map, and an oval cone on the tangential map (top). The final FlexLens ARC fit (bottom). Click image to enlarge. |
The Standard
These lenses cannot mask or hide any corneal irregularity. Their best application is in cases of mild corneal irregularity, where the topography is somewhat symmetrical centrally and patients are satisfied with their acuity after manifest refraction. Standard soft lenses benefit the patient and practitioner by providing a readily available product that is comfortable and carries a lower cost burden than a specialty lens. Due to the availability of extended-range refractive parameters, this can be a convenient and viable option.
Case #1: A 29-year-old woman with a history of traumatic aphakia and a corneal scar from a laceration that occurred in her right eye at the age of 12 had been unable to tolerate wearing glasses due to high anisometropia and failed in the past with a unilateral corneal GP lens due to discomfort. She desired a simple yet cost-effective option that provides comfortable wear from the outset.
Manifest refraction:
OD: +9.00D -1.50 x 060 VA 20/30
OS Plano VA 20/20
To determine if a standard soft toric lens would be sufficient, the closest power available from a silicone hydrogel toric diagnostic fitting set was placed on the eye: +4.00D -1.75 x 060. The lens decentered slightly inferior-temporally but with full corneal coverage and 0.5mm of movement. The toric marking was rotated 10º to the right but the rotation was stable. The patient was comfortable and pleased with the vision achieved through a +5.50DS over-refraction. A diagnostic lens with the appropriate resultant power: +10.00D -1.75 x 050 was ordered and dispensed yielding 20/25-3 final BCVA. The patient was happy that she was able to see clearly and comfortably.
In this case, if the standard soft lens was severely decentered yielding corneal exposure, or if there had been excessive or unstable lens rotation, then a custom soft lens may be a superior choice. Remember that standard soft lenses are a “one-size-fits-all” approach and may not always work because irregular corneas are just that, irregular. Fortunately, this was not such a case.
 |
|
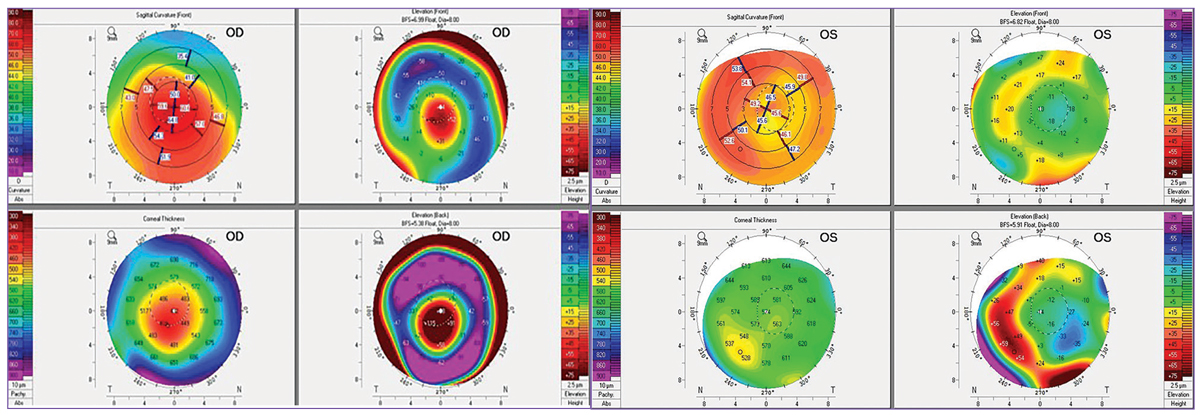
Pentacam maps of patient in Case #3 showing keratoconus OD and a corneal transplant OS. Click image to enlarge. |
Custom Options
Standard soft lenses usually come in one or two base curve (BC) options, one diameter option and a finite range of powers. These lenses are manufactured with a sagittal height range that fits the average ocular sagittal height and horizontal visible iris diameter (HVID) of 11.8mm to 12.0mm, which applies to approximately 77% of eyes.1 It follows, then, that the remaining 23% (almost a quarter of your patient base) are outliers for standard SCLs based on corneal size alone, absent any additional irregularities.1
This is where custom options can help, as they can be manufactured with a wide range of parameters, allowing the practitioner to customize the diameter, BC, optic zone, center thickness (CT) and lens power for each patient. Power options cover almost any conceivable sphere (in 0.12D steps), cylinder (in 0.25D steps) and axis (down to 1° steps) combination independently of one another to maximize both patient and practitioner success.
For the irregular cornea, fitting soft lenses often requires reaching for a specialty soft design that incorporates one of two fitting premises: 1) an aspheric design limits aberrations or 2) an increased CT masks irregular astigmatism. These specialty soft lenses are custom-manufactured but are generally fit using a diagnostic fitting set. In cases where the practitioner has advanced imaging technology and profilometry, they may be fit empirically.2 For each specialty soft design, it is recommended to follow the manufacturer’s fitting guide for initial lens selection, evaluation and troubleshooting.
The specialty soft lens modality for the irregular cornea encompasses 15 different designs (Table 1), available in hydrogel or silicone hydrogel materials. A specialty soft lens can offer better initial comfort than a corneal GP, along with good centration and adequate vision if, or when, standard SCLs fail. However, they are not without drawbacks: more time to fit and manufacture, while also carrying a higher annual supply cost. They typically have a less frequent replacement schedule than standard soft lenses, and in some instances, patients experience reduced comfort due to the increased CT of a specialty soft lens design.
The initial specialty soft lens is selected based on sagittal depth, not on BC, as the goal is to match the sagittal depth of the lens to the ocular sagittal height to ensure adequate draping of the soft lens and also enhance on-eye stability and comfort.3
The lens should typically be 3mm larger than the patient’s HVID so that it extends 1.0mm to 1.5mm beyond the limbus in both directions to allow for complete corneal coverage and stability. The HVID can be measured manually with a ruler or obtained from a topography map. Since the corneal diameter/HVID is the most important factor affecting sagittal depth, measure this prior to fitting any custom lens.3 This is important to consider because for the same corneal curvature, a larger HVID will carry a higher sagittal depth and vice versa, a smaller HVID will carry a shallower sagittal depth.
In addition to assessing the sagittal depth of the eye, observe the corneal profile and whether it is prolate (as in corneal ectasia) or oblate (as in post-refractive surgery). The corneal profile can be crucial to initial diagnostic lens selection as some specialty soft lenses have separate prolate or oblate designs. If the corneal apex is within the central 4mm, a standard prolate lens will often give a superior result; however, if the apex is outside the central 4mm, an oblate (reverse geometry) design may be superior. In these reverse geometry specialty soft lenses, the central BC is flatter than the secondary curve, allowing the lens to more closely align to an oblate cornea profile. This advantage is useful in post-transplant, pellucid marginal degeneration or previously myopic refractive surgery patients.
 |
|
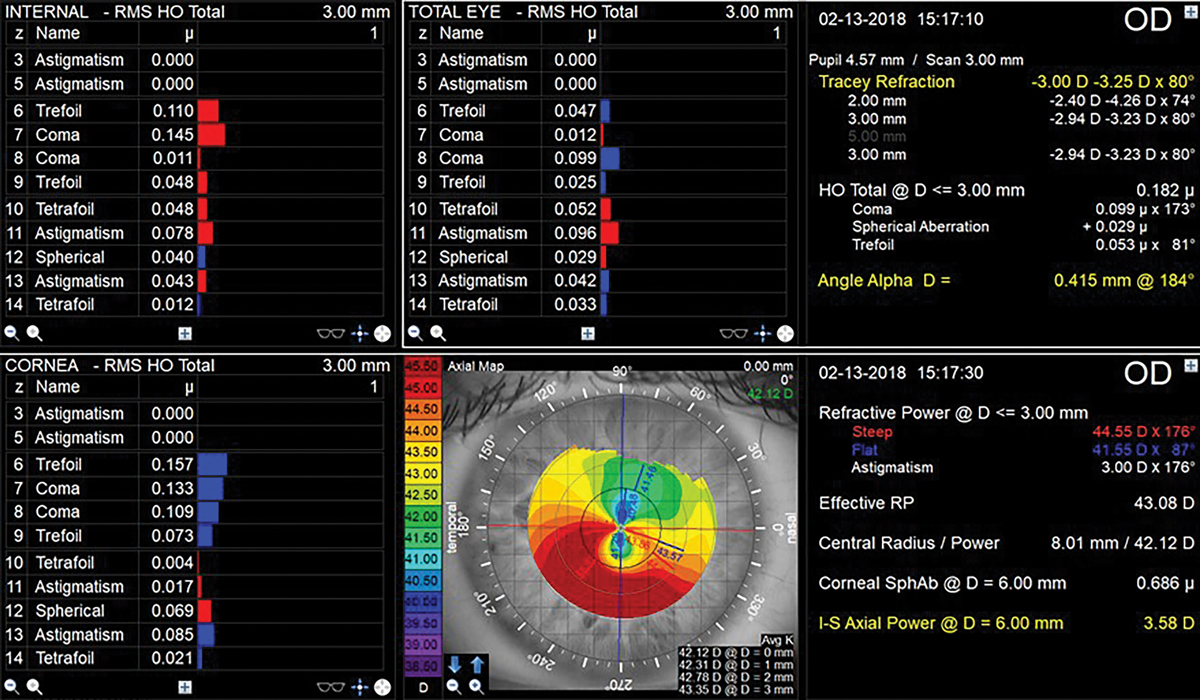
Topography and aberrometry readings from the right eye of the patient in Case #4. Click image to enlarge. |
Patients with a higher degree of corneal irregularity also typically have higher amounts of astigmatism that need correction with lenses. To aid in correcting irregular astigmatism, some specialty soft lens designs allow the CT to be customized with a range from 0.30mm to 0.60mm thickness. This provides some level of “pseudo-rigidity” and a smoothing effect of the irregularity, thus improving vision. The downside of this increased thickness is reduced oxygen transmission. With these designs, choose a silicone hydrogel material where available to aid in oxygen transmission. If only a hydrogel material is available, it is crucial to ensure adequate lens movement (sometimes 1.0mm to 2.0mm worth) to facilitate tear exchange and reduce the risk of cornea hypoxia.
The designs are all unique. They’re available in double slab-off or prism-ballast for the stabilization of front toric optics, full-diameter or central thick zones, and either variable BC or dual-curve (BC and separate peripheral curve) designs.4
In a dual-curve design, the BC and the peripheral curves can be adjusted independently with the central BC impacting vision while the periphery impacts the fit, centration and movement of the lens. If the BC is too steep, the patient will note that their vision is clearest immediately following a blink and then is worse. If the BC is too flat, the patient will report vision gets worse right after the blink and improves with staring. The vision can also fluctuate significantly due to excessive movement and/or unstable lens rotation. In dual-curve designs, the periphery of the lens can be modified to help eliminate the presence of air bubbles or fluting as well as to achieve the appropriate amount of lens movement to facilitate tear exchange.5 In a few designs, the peripheral curve can incorporate a quadrant-specific modification to ensure proper lens centration.5
Higher amounts of cylinder correction in soft lenses make patients more sensitive to visual fluctuations and excessive rotation can yield a higher cross-cylinder effect. Therefore, assessing the stability of vision and lens movement/rotation on the blink is imperative for success with both custom soft and specialty soft lens designs. Informing patients about this potential hurdle prior to starting the fitting process can set appropriate expectations for visual success and the number of visits it will take to complete the fitting process. If your patient has a history of GP lens wear, additional discussion of the visual limitations of specialty soft designs may be warranted.
More Cases: How To Choose?
As practitioners, we must look at our exam data and the patient’s visual demands when deciding which lens modality to fit. We often primarily consider that which we can measure: the patient’s incoming acuity, visual potential, refractive data, corneal profile, HVID, topography, the severity of irregularity, and ocular health; however, we can’t neglect the rest of the patient’s story. To provide patient-centered care, ask about the patient’s occupation, hobbies, visual symptoms, visual goals, and past CL history, while also considering their level of manual dexterity when making lens recommendations.
Case #2: A 32-year-old man with bilateral keratoconus presented complaining of visual distortion OU in his habitual spectacles. He last wore GP lenses four years prior and discontinued wear due to discomfort. He works as a butcher and enjoys watching professional soccer. At work, he is mostly focused on near and intermediate tasks but wants freedom from spectacles in that environment.
The patient’s anterior segment exam was remarkable for signs of keratoconus and allergic conjunctivitis, along with a nasal pinguecula in each eye.
Refraction:
OD: -1.50D -7.00 x 027 VA 20/30
OS: -1.25D -10.50 x 150 VA 20/60
The patient was fit in a specialty soft lens. For the right eye, a FlexLens ARC Toric 6.9/14.5/0.50T was trialed with an over-refraction of plano -5.00 x 025 and a BCVA of 20/25+. For the left eye, a FlexLens ARC Toric 6.6/14.5/0.50T was trialed with an over-refraction of -4.25 -1.50 x 150 and a BCVA of 20/50. Frankly, we expected more cylinder and a better best-corrected acuity. Since the acuity improvement OS was minimal at only one line better than the spectacle acuity through a diagnostic specialty soft lens, we trialed a scleral lens OS. Through an Atlantis scleral 7.67/15.0/-3.00/std periphery and an over-refraction of +4.00 -0.75 x 060, the patient’s vision improved to 20/30-2 OS.
After discussing the options, the patient opted for the soft lens despite better visual potential with the scleral lens OS. At the dispensing visit, the OD specialty soft lens fit well and achieved the expected acuity. The OS lens was well centered with 1.0mm movement and no rotation but only gave VA of 20/70; however, a careful over-refraction yielded +1.25D -3.75 x 160 and a BCVA of 20/40+2. The cross-cylinder result was calculated and ordered giving a final specialty soft contact lens power of -3.00D -5.25 x 157 OS.
At the dispensing visit, the patient’s vision improved to 20/30- OS and he was thrilled (our more careful over-refraction here paid off). He denied any issues with lens handling and only had mild dryness while at work, which was relieved with the use of artificial tears.
Table 1. Specialty Soft Contact Lens Designs for the Irregular Cornea
ABB Optical Group (www.abboptical.com) | Concise K, Kerasoft IC, Kerasoft Thin |
Art Optical (www.artoptical.com) | Kerasoft IC Thin |
AVT (www.avtlens.com) | Soft K, SH Soft K II, Naturasoft, Continential Soft |
Bausch + Lomb Specialty Vision Products (www.bauschsvp.com) | NovaKone |
Gelflex (www.gelflex.com) | Gelflex Reverse Geometry Post-Surgical |
Metro Optics (www.metro-optics.com) | RevitalEyes Post-Surgical, Kerasoft IC Thin |
United Contact Lens (www.unitedcontactlens.net) | UCL-55 Keratoconus |
X-Cel (www.xcelspecialtycontacts.com) | Flexlens ARC, Flexlens TriCurve, Flexlens Piggyback, Flexlens PRS |
Case #3: A 48-year-old man with keratoconus and INTACs OD, s/p PKP OS presented wearing no correction OD and a Proclear Toric XR OS. He is a firefighter who works overnight shifts and needs the flexibility to fall asleep in his lenses. He was previously fit with a corneal GP OD that he was unable to tolerate. He was refit into a scleral OD but cannot wear it to work because he cannot sleep in it, but he loves the vision and comfort of the scleral when not at work. At work, he’s not been wearing any corrective lenses OD and habitually wears a Proclear Toric XR 8.4BC/14.4/-2.25-3.75x075 OS, but that lens had been shifting more than once a day for the last six months. Upon slit lamp evaluation there was significant fluting nasally and unstable rotation of 40º to 60° to the right.
Entering VA with correction:
OD: 20/500; OS CL: 20/50-2
Refraction:
OD: -10.25D -3.00x045 VA 20/80-2
OS: -4.75D -1.75x120 VA 20/30
For a simplistic approach, a standard soft toric diagnostic trial was placed on each eye with the closest power available to the vertex converted prescription; however, both lenses exhibited excessive fluting indicating a custom soft toric contact lens would be needed. Silicone hydrogel custom soft toric lenses were empirically ordered based off of manifest refraction, HVID and tomography:
OD: 7.10BC/15.0/-9.25-2.25x045 with a CT of 0.2mm VA 20/70-2
Over-refraction: Plano, no rotation
OS: 7.60BC/15.0/-4.50-1.50x030 with a CT of 0.2mm VA 20/30+2
Over-refraction: -0.25-1.00x045, no rotation
Cross-cylinder calculation OS yielded a final resultant power of: -4.75-2.50x036 and VA of 20/20-3
Custom soft lenses proved to be a suitable alternative for the demands of his occupation.
Case #4: A 28-year-old man with keratoconus OS>OD and a history of crosslinking presented wearing scleral lenses OU. He didn’t like the right lens, as he feels like his vision is worse in the scleral than in his glasses. The lenses were two years old, and he would like to get them updated, in hopes of improving vision OD.
VA (in scleral) OD: 20/30+2
VA (in scleral) OS: 20/25
Refraction:
OD: -4.25-2.75x080 VA 20/20
OS: -3.00-4.50x080 VA 20/40
The patient’s total higher-order aberrations (HOAs) were less than those of the corneal and internal HOAs, making him a poor candidate for a scleral or specialty soft lens with any rigidity; these designs will cause the residual internal aberrations to become more apparent. This explains what he’s been experiencing with his scleral for his right eye. When this eye was refit into an aspheric custom soft contact lens, the BCVA improved to 20/15.
It may be tempting to offer a universal solution by fitting every patient with corneal irregularity into a GP lens; however, clinicians must carefully assess the unique needs of each patient. Soft lenses really can and do have a place in vision rehabilitation for patients with irregular corneas and can improve their quality of life.6 As with any lens modality, it’s about choosing the appropriate candidate and counseling them about expectations. Furthermore, keeping up-to-date with diagnostic instrumentation and advancements in contact lens designs and materials is also important in order to continue to provide the best care to these patients.
Dr. Andrzejewski practices at Chicago Cornea Consultants and serves as an adjunct assistant professor of optometry at the Illinois College Optometry (ICO) as well as the Chicago College of Optometry. She is a consultant/speaker for Bausch + Lomb Specialty Vision Products, Contamac, CooperVision Specialty EyeCare and Essilor Contacts.
Dr. Sicks is an associate professor at ICO and serves as a clinical attending in the Cornea and Contact Lens Center for Clinical Excellence at the Illinois Eye Institute. She is a consultant/speaker for Alcon Laboratories.
1. Caroline P, André M. The effect of corneal diameter on soft lens fitting, part 1. Contact Lens Spectrum 2002;17(4)56. 2. Chang C, DeNaeyer GW. Specialty contact lenses: treat your keratoconus patients right. RCCL. 2017;154(2):14-7. 3. Young G. Ocular sagittal height and soft contact lens fit. Cont Lens Anterior Eye. 1992;15(1):45-9. 4. Gelles J. Specialty lenses for irregular cornea and ocular surface disease. Contact Lens Spectrum. 2020;35(2):20-5;49. 5. Andrzejewski T. Managing irregular corneas with soft lenses. RCCL. 2020;157(1):12-6. 6. Yildiz EH, Erdurmus M, Elibol ES, Acar B, et al. Contact lens impact on quality of life in keratoconus patients: rigid gas permeable vs. soft silicone-hydrogel keratoconus lenses. Int J Ophthalmol. 2015;8(5):1074-7. |


