 |
A 43-year-old female presented with blurry vision through her habitual glasses. A previous GP lens wearer, she had self-discontinued as she felt glasses met her visual needs better and were easier to use. Her entering distance visual acuity with glasses was 20/30-1 OD and 20/30 OS. Her new refraction was OD -10.00-5.50x005 and OS -10.25-5.25x176. Entrance testing and slit-lamp exam were within normal limits.
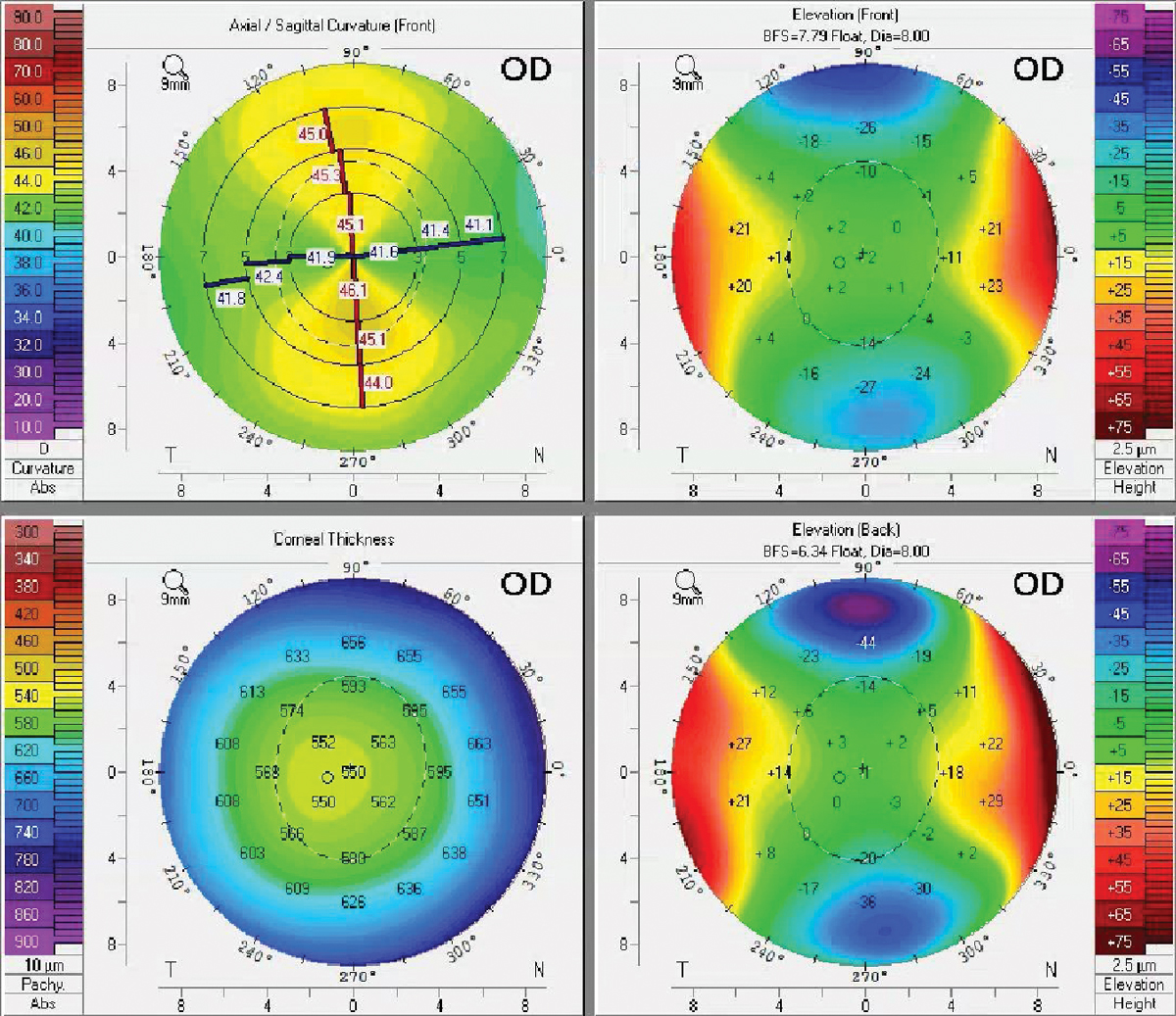
Corneal tomography was obtained to rule out corneal ectasia due to the high ametropia and astigmatism. The scans revealed limbus-to-limbus, WTR astigmatism in each eye with no signs of ectasia (Figure 1). Simulated K results were OD: 41.6/45.6@090 and OS: 42.2/45.5@078. Pupil size in bright illumination was 4.0mm OD, OS.
 |
|
Fig. 1. Maps show regular WTR astigmatism OD. The OS had a similar appearance. Click image to enlarge. |
Consider GP Lenses
Since the patient was a previous corneal GP wearer and astigmatism is a common indication for GP lenses, we proceeded with an empirical GP lens fit. We evaluated the corneal astigmatism amount and location. When there is little peripheral corneal toricity, one may be able to fit the patient into a spherical or aspheric design (especially with low amounts of astigmatism). This patient had high WTR corneal astigmatism (OD 4.00D and OS 3.30D) that was limbus-to-limbus in nature. Thus, a bitoric corneal GP design will provide the best lens-cornea fitting relationship and minimize rotation (as there is a large amount of toricity).2
Bitoric and back toric lenses are most successful when the keratometric axis differs from the spectacle cylinder axis by less than 15°; this was indeed the case for this patient.1 Topography maps can be useful not only for evaluation of astigmatism but also to look for a large sagittal height differential (more than 30µm) or a large eccentricity differential (>0.20e), either of which may signal the need for a toric lens design.3
The majority of corneal astigmatism occurs with the steeper curve in the vertical meridian (with-the-rule). If fit with a spherical corneal GP, there will typically be heavy bearing along the flatter (horizontal) meridian. As a result, poor centration, physical discomfort and poor vision are likely.4
Typically, the lower limit for a well-stabilized toric lens is 2.00 to 2.50D of corneal astigmatism.4 When designing a lens, the toricity of the base curve will ideally be at least two-thirds of the full amount of corneal toricity (it does not always need to be equal). Without this amount of toricity matching, there can be induced over-refraction, resulting in reduced best-corrected visual acuity (BCVA).
 |
|
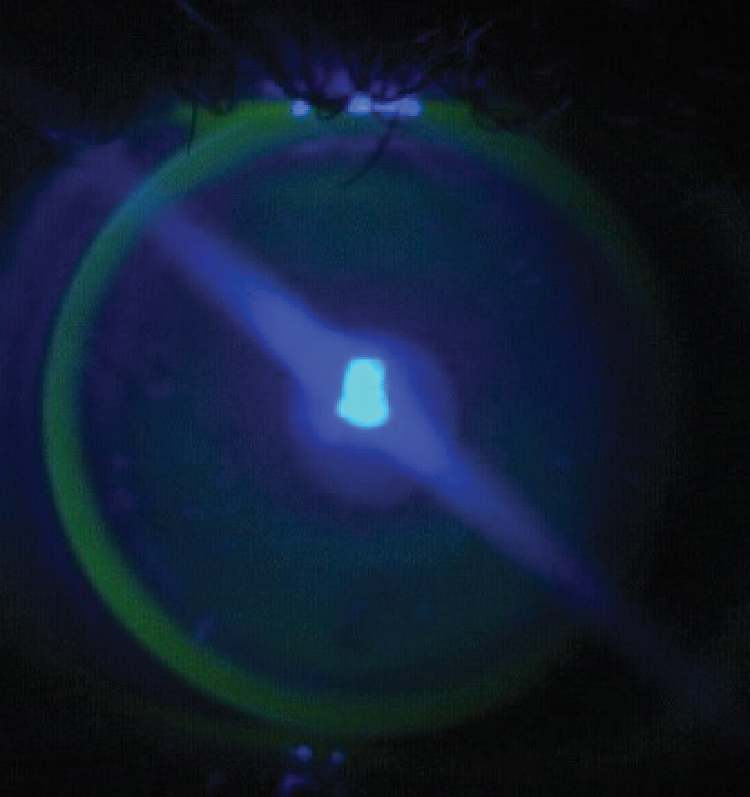
Fig. 2. A well-fit bitoric lens on an astigmatic cornea demonstrates an appropriate fit with central alignment, mid-peripheral bearing and adequate edge lift. Click image to enlarge. |
The initial lens parameters were configured for this patient using the Mandell-Moore Bitoric Lens Guide. Because she was returning to lens wear after a long hiatus and since the upper lid was positioned below the upper limbus, our goal was a lid-attached fit. Because of this goal and the high minus lens power necessary due to her refraction, we chose a 9.6mm OAD lens. This resulted in an initial optic zone size of 8.2mm (as determined by the lab). The initial lens order was OD BC 8.16/7.53, power -9.00/-12.25 and OS BC 8.04/7.54, power -9.12/-13.00. The peripheral curves were spherical and the edge thickness was optimized to 0.10mm by the laboratory.
At dispensing, the patient’s BCVA through the new bitoric lenses improved to 20/25+ OD and OS (compared with 20/30 in spectacles). Both lenses were lid attached and sitting slightly superiorly. Each demonstrated ideal apical alignment, adequate mid-peripheral bearing and acceptable edge lift, similar to what is seen with a well-fit spherical lens on a spherical cornea (Figure 2). The flat meridian marking on both lenses was stable (i.e., no lens rotation and therefore no induced astigmatism).
At the next visit two weeks later, she was happy with her vision overall, but noticed glare and halos when driving at night. Acuity through the lenses was 20/25 OD and OS. An over-refraction of +0.50DS OU improved vision to 20/20- in each eye. The fit and fluorescein pattern were identical to the dispensing visit, with slight superior decentration and a stable lens marking (Figure 3). The glare and haloes were exacerbated by the lid-attached fit causing superior decentration and her increased pupil size in dim illumination.
Ideally, the optic zone diameter (OZD) should be greater than the pupil size in dim light to prevent flare symptoms. Additionally, when contact lenses are decentered, the peripheral curves can enter the visual axis, causing flare symptoms.1 To combat the impact of these factors, the optic zone size was increased in each eye from 8.2mm to 8.4mm and the over-refraction was incorporated. The patient was happy with her vision and comfort from these new lenses and appreciated the resolution of the haloes and glare.
Another GP lens adjustment that would reduce the glare/flare in this case would be to incorporate peripheral curve toricity. When a spherical secondary curve is applied to a toric base curve lens, the result is an oval optic zone, which can induce flare symptoms. Other options to assist with centration would include steepening the base curve, increasing the lens center thickness or further thinning the lens edge.
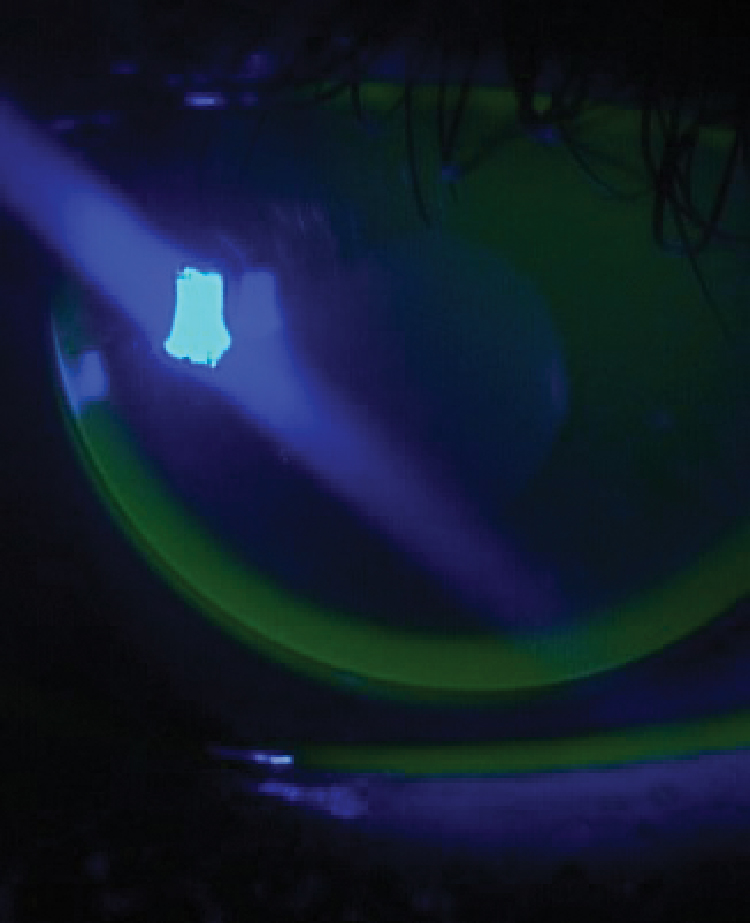 |
Fig. 3. Bitorics often have markings to denote the flat meridian (see approximately nine o’clock). This can help determine if the lens is stable or if vision fluctuations are being caused by unwanted lens rotation. Click image to enlarge. |
Perfect the Bitoric Fit
In patients with ≥ 2.50D of corneal astigmatism, a bitoric or back toric GP lens should always be considered. On highly toric corneas, toric lenses provide better stability and centration compared to spherical GP lenses. Bitoric lenses have both a toric back and toric front surface (whereas a back toric would only have a toric back surface), thereby correcting for any residual astigmatism present.
The base curve and power in each meridian can be determined by many methods, including using a standard fit factor (e.g., Mandell-Moore or Remba) or a low toric simulation. Alternatively, diagnostic fitting is streamlined by using a spherical power effect bitoric lens fitting set.
The Mandell-Moore Bitoric Lens Guide is an empirical fitting strategy that uses keratometry measurements and refraction to determine the appropriate GP lens power and base curve radius in each meridian.1 This method produces comparable fitting success to that seen with diagnostic fitting of bitoric lenses.1 The lens is fit 0.25D flatter than the flat keratometry reading in one meridian and 0.75D flatter than the steep keratometry reading in the opposite meridian. Fitting flatter in the steep meridian allows for tear exchange, and that flatter edge allows for lid attachment and added stabilization.
OZD Adjustments
Ideally, a GP’s OZD should be as large as possible to facilitate centration and minimize glare. The OZD typically encompasses 65% to 80% of the overall diameter of the lens.1 The initial OZD for this patient was 8.2mm based on the 9.6mm OAD. Due to the glare and haloes, OZD was further increased to 8.4mm with resolution. Making such changes can affect the overall lens fit. Thus, one should flatten the base curve by 0.25D for every 0.5mm OZD increase.1 Other cautions with a larger OZD include limited lateral lens movement and the potential for corneal desiccation, as the lens does not move as much over the periphery.5
Consider bitoric GPs in patients with high corneal and refractive astigmatism. Watch the lens fit for centration and stability and don’t be afraid to consider fit and/or OZD changes to alleviate glare.
1. Bennett ES, Henry VA. Clinical manual of contact lenses. 3rd ed. Lippincott Williams & Wilkins. 2019;336-44. 2. Hom MM, Bruce AS. Manual of contact lens prescribing and fitting. Elsevier Health Sciences. 2006. 3. Lampa M, Fujimoto MJ, Caroline PJ. Topography and contemporary corneal GP lens fitting. Continuing Education Lecture. Amer Acad Optom. 2020. 4. Phillips AJ, Speedwell L. Toric contact lens fitting. Contact lenses. 5th ed. Butterworth-Heinemann. 2006. 5. Bennett ES, Weissman BA. Clinical contact lens practice. 2nd ed. Lippincott Williams & Wilkins. 2005. |


