 |  |
Since 2005, the annual number of penetrating keratoplasty (PK) procedures performed in the United States has decreased by 56%.1 When transplantation is required, more selective procedures, such as anterior lamellar keratoplasty and endothelial keratoplasty, have contributed to the reduced need for full-thickness grafts. However, PKs are still performed in cases of advanced corneal disease or opacification.
A full-thickness PK replaces all layers of the cornea with a donor button, typically 7.5mm to 8.5mm in diameter, sutured in place to the host tissue.2 Newer surgical techniques such as using a femtosecond laser to create the donor button have improved postoperative wound stability and reduced healing time.3 However, refractive outcomes are still variable, and are largely impacted by the amount of astigmatism that the graft produces. High amounts of astigmatism are not uncommon, with one large cohort study reporting at least five diopters of astigmatism in 20% of grafts.4 If spectacles do not provide a successful visual outcome, contact lenses, specifically gas permeable (GP) lenses, may be required for vision rehabilitation.
Lens Considerations
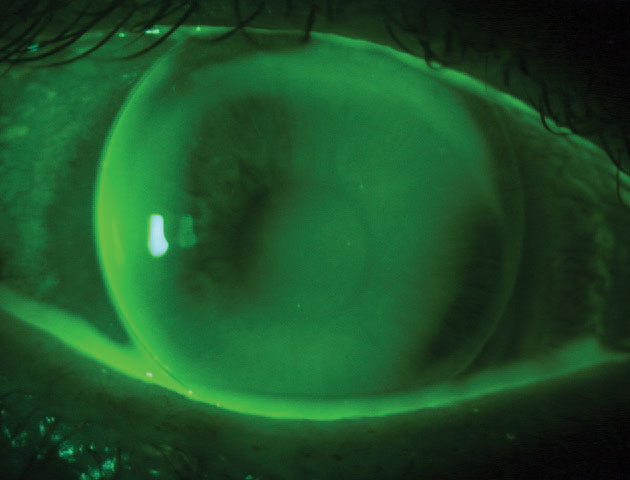
Because of their ability to vault over the corneal surface, scleral lenses are becoming an increasingly popular lens choice for post PK patients. While mechanical stress may be minimized, careful observation for signs of hypoxia is critical. Scleral lenses are made with highly oxygen permeable (DK) materials, but they must also take into account the diffusion of oxygen through the post-lens tear layer. If excessive hypoxic stress is placed on the endothelium, corneal edema may occur and increase the risk of rejection. Smaller-diameter corneal GP lenses use the same high DK materials and also benefit from a greater tear exchange beneath the lens. This improves oxygen tension and is suggested to play a role in the lower risk of microbial keratitis with GP lenses.5,6
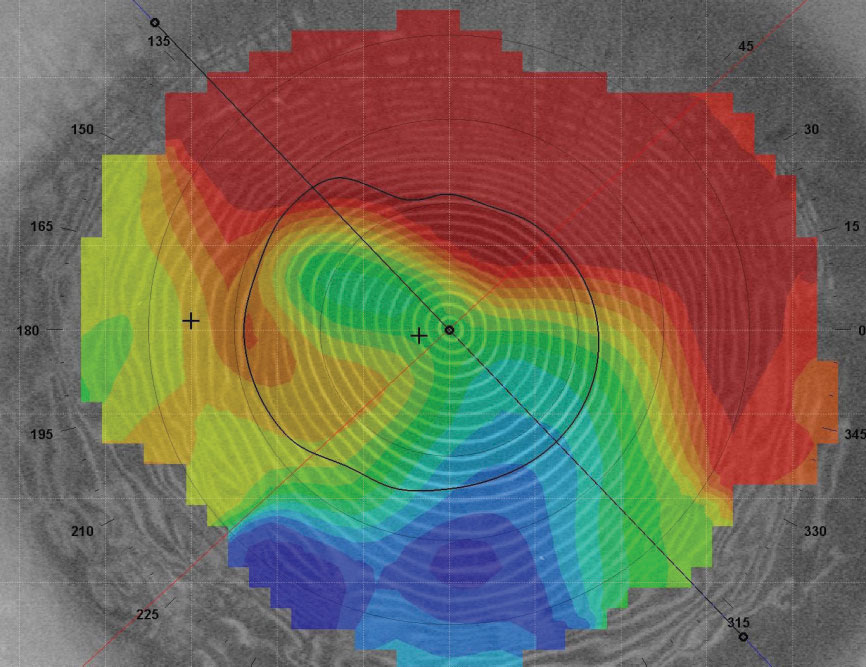 |
| Post-PK, the cornea can take on a steep-to-flat pattern where the graft is tilted. |
The Corneal Profile
The goal of fitting GP lenses is to align the lens’s back surface to the anterior curvature of the cornea. With a normal cornea, eyelid positioning and keratometry measurements are used to select diameter and base curve. For PK patients, analyzing astigmatism and corneal shape with the aid of corneal topography will help dictate the proper contact lens fit.Regular astigmatism has two principal meridians perpendicular to each other in a bowtie pattern. Depending on the power of each half of the bowtie, regular astigmatism can be classified further as symmetrical or asymmetrical. When the cornea is non-uniform or principal meridians are not 90 degrees apart, the astigmatism is considered irregular, with several pattern subtypes.7 Irregular astigmatism is the most common indication for fitting GP lenses post-transplantation.8
Corneal shape is typically classified into three basic patterns: prolate, oblate and mixed. Prolate-shaped corneas are steeper centrally and flatter in the periphery, while oblate-shaped corneas are flatter centrally and steeper in the periphery. Mixed-shape features both prolate and oblate areas of the cornea. Post-PK, the cornea can also take on a steep-to-flat pattern where the graft is tilted, steep on one side and flatter towards the other side.7,9
Fitting Strategy
A well-fit GP lens will minimize mechanical trauma to the graft, optimize vision and be comfortable to the patient. Maintaining proper centration and distributing weight equally on the cornea can achieve these objectives.
In general, larger-diameter intralimbal lenses (10mm to 12mm) are preferred because their back optical zone diameter will extend beyond the graft-host junction.9,10 If small-diameter lenses must be used, care must be taken to avoid heavy bearing, especially on the junction.
Choosing a back surface design for the lens is dependent on the corneal profile. Prolate corneas with regular astigmatism and a normal eccentricity can often still be fit in a conventional spherical lens. If the regular astigmatism is 2.5D or more, a bitoric design can be fit to avoid lens rocking and areas of heavy touch. When the graft is steeper, a keratoconic design, which typically has a steeper base curve and smaller optic zone size, can be used. Proud grafts that protrude more from the host cornea may require a quadrant specific peripheral curve design if there is excessive edge lift. A reverse geometry lens, in which one or more peripheral curves are steeper than the optical zone curvature, can also reduce peripheral edge lift.9
Reverse geometry lenses are also useful for oblate corneas. A conventional GP would exhibit excessive central clearance, at risk for bubble formation, mid-peripheral bearing and edge lift. Flattening the base curve to match the central cornea and steepening the peripheral curves will better match corneal contour, with a fluorescein pattern appearing to be in alignment. If the graft is tilted, a GP lens will tend to center over the steepest part of the cornea. Larger-diameter lenses help with centration, although in these cases scleral lenses may indeed be the preferred choice.
 |
| A mini-scleral lens may be the option for your patient with high corneal astigmatism. |
Other Options
Discomfort and decentration can potentially derail the success of GP lenses. A piggyback system may be an effective option to correct both complications. A soft silicone hydrogel (SiHy) lens can be placed under the GP lens to reduce friction on the cornea. The power profile of the soft lens can help manipulate centration. A high myopic powered soft lens will act as a carrier for the GP lens to rest on, while a high plus lens may “fill in” an oblate cornea.10 In a piggyback design, the soft lens will provide only 20% of the total optical power of the system.11 Because oxygen must now diffuse through two lenses, careful monitoring for corneal hypoxia is warranted.
Contemporary hybrid lens designs are also available for post-surgical corneas. The SynergEyes UltraHealth lens is designed using a hyper DK reverse geometry GP lens and a high DK SiHy skirt. The GP lens vaults over the cornea with minimal touch and the soft skirt maintains centration with minimal movement.
The versatility of scleral lenses makes them a popular choice for the post-PK patient; however, they are not without risk. If a graft patient cannot tolerate or afford a scleral lens, they have options. Don’t be afraid to put your GP fitting skills to the test!
1. Eye Bank Association of America. 2016 Eye Banking Statistical Report. restoresight.org/wp-content/uploads/2017/04/2016_Statistical_Report-Final-040717.pdf. Accessed December 23, 2018. 2. Richard JM, Paton D, Gasset AR. A Comparison of penetrating keratoplasty and lamellar keratoplasty in the surgical management of keratoconus. AM J Ophthalmol. 1978;86(6):807-11. 3.Farid M, Pirouzian A, Steinert RF. Femtosecond laser keratoplasty. Int Ophthalomol Clin. 2013;53(1):55-64. 4. Kelly TL, Williams KA, Coster DJ. Corneal transplantation for keratoconus: A registry study. Arch Ophthalmol. 2011; 129(6):691-7. 5. Weissman BA. Corneal oxygen: 2015. CL Spectrum. 2015;30:25-29,55. 6. Fleiszig SM. The pathogenesis of contact lens-related keratitis. Optom Vis Sci. 2006;83:E866-73. 7. Karabatsas CH, Cook SD, Sparrow JM. Proosed classification for topographic patterns seen after penetrating keratoplasty. BR J Ophthalmol. 1999;83:403-9 8. Wietharn BE, Driebe WT Jr. Fitting contact lenses for visual rehabilitation after penetrating keratoplasty. Eye & Contact Lens 2004; 30(1):31–33. 9. Szczotka LB, Lindsay RG. Contact lens fitting following corneal graft surgery. Clin Exp Optom. 2003;86(4):244-9. 10. Louie DJ, Kawulok E, Kauffman M, Epstein A. Postsurgical contact lens fitting. In: Bennett ES, Henry VA, eds. Clinical Manual of Contact Lenses. 4th Ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2014:578-608. 11. Woo M, Weissman B. Effective optics of piggyback soft contact lenses. CL Spectrum. 2011;26(11):50. |


