 As we see patients daily, we remain on the quest to provide greater comfort to our contact lens wearers. For a successful contact lens wearing experience, the health of the tear film and ocular surface that will support the contact lens needs to be balanced with the lens design, material and care systems that are created to care for the lenses. A patient who has little to no symptoms of dry eye when not wearing contact lenses may, for example, complain of dry eye symptoms when contact lenses are worn—likely manifested by a tear film that becomes inadequate to sustain comfortable wear.
As we see patients daily, we remain on the quest to provide greater comfort to our contact lens wearers. For a successful contact lens wearing experience, the health of the tear film and ocular surface that will support the contact lens needs to be balanced with the lens design, material and care systems that are created to care for the lenses. A patient who has little to no symptoms of dry eye when not wearing contact lenses may, for example, complain of dry eye symptoms when contact lenses are worn—likely manifested by a tear film that becomes inadequate to sustain comfortable wear.
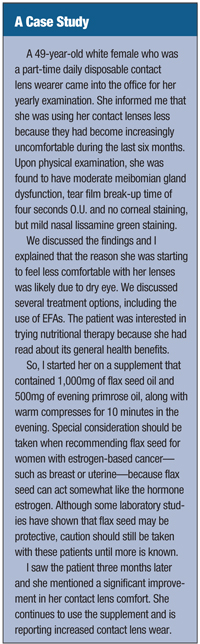
Several factors, such as nutrition, can affect the quality of the tear film and the health of the ocular surface. Nutrition is a growing area in healthcare, particularly for conditions like diabetes, hypertension and heart disease. Large-scale studies in eye care, such as the Age-Related Eye Disease Study (AREDS) and the Blue Mountain Eye Study, have demonstrated the benefits of nutrition in patients with macular degeneration.1,2 Similarly, nutrition can also have a role in optimizing the ocular surface by helping to promote a healthy tear film that can support comfortable lens wear.
Breaking Down EFAs
 Essential fatty acids (EFAs) have commanded much attention in health care because of their general health benefits. EFAs have a potent anti-inflammatory effect, which provides much of the health benefits seen with these nutrients.3,4 The ocular surface also benefits from their anti-inflammatory actions.
Essential fatty acids (EFAs) have commanded much attention in health care because of their general health benefits. EFAs have a potent anti-inflammatory effect, which provides much of the health benefits seen with these nutrients.3,4 The ocular surface also benefits from their anti-inflammatory actions.
Alpha linolenic acid (ALA)—commonly found in flax seed and black currants—can be converted to eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). EPA and DHA, long chain omega-3 fatty acids, are naturally found in fresh water fish. EPA and DHA can be converted to prostaglandin E3 (PGE3) by the enzyme cyclooxygenase (COX). PGE3 is a subclass of prostaglandins that has anti-inflammatory activity and helps inflamed tissues like the ocular surface. EPA can also be converted to leukotriene B5 (LTB5) via lipooxygenase; LTB5 has anti-inflammatory activity.5-8
Many omega-6 fatty acids—a large part of the typical North American diet—can create inflammation. However, when the proper type of omega-6 fatty acid in the appropriate quantity is consumed, it can provide beneficial anti-inflammatory properties. Linoleic Acid (LA), for example, is a type of omega-6 that can be converted to gamma-linolenic acid (GLA). GLA is then converted to dihomo-gamma-linolenic acid (DGLA). DGLA will enter one of two metabolic pathways. It may be converted directly to a subclass of prostaglandin that has potent anti-inflammatory activity, prostaglandin E1 (PGE1). It may be converted to arachidonic acid (AA) by delta-5-desaturase; AA is then readily converted to prostaglandin E2 (PGE2) by cyclooxygenase and leukotriene B4 (LTB4) by lipoxygenase. Both PGE2 and LTB4 are pro-inflammatory.9,10
The conversion of omega-3s and omega-6s to their eventual end products is a well coordinated event where byproducts of one pathway will interact with the other. As an example, EPA—a byproduct of omega-3 metabolism—will inhibit the enzyme delta-5-desaturase. This enzyme converts DGLA into AA, which is the precursor to pro-inflammatory prostaglandins and leukotrienes.11,12 Thus, EPA is a precursor to the production of anti-inflammatory mediators via omega-3 metabolism. It also promotes the inhibition of pro-inflammatory products via one of the pathways of omega-6 metabolism.13
What the Research Tells Us
In a one month randomized, double-masked, controlled clinical trial, 40 patients with Sjögren’s syndrome were randomized to either receive 112mg LA and 15mg GLA b.i.d. p.o., or a placebo. Patients using the LA and GLA showed a significant increase in PGE1 with its anti-inflammatory properties, reduced ocular symptoms and a reduction of corneal fluorescein staining.14
In another study, 26 patients with aqueous deficient keratoconjunctivitis sicca were randomized to either 28.5mg of LA and 15mg of GLA twice a day, or a placebo. After 45 days, the treatment group showed significant improvements in ocular symptoms, lissamine green staining and ocular surface inflammation.15
Meibomian gland function is imperative for proper ocular surface health as well as a healthy tear film. Compromised meibomian gland function may lead to evaporative dry eye. A study randomized 57 patients to one of three groups: patients taking tablets that contained 28.5mg of LA and 15.1mg of GLA once a day; patients who performed eyelid hygiene once a day; and patients who received both treatments. The subjects who received both treatments showed improved symptoms and signs of eyelid margin inflammation more than subjects who received either treatment alone.16
In another study, 36 dry eye patients were randomized to either receive a daily dose of fish oil—containing 450mg of EPA, 300mg of DHA and 1,000 mg of flaxseed oil—or a placebo for 90 days. Interestingly, 70% of the patients receiving the treatment became asymptomatic, whereas just 7% of those receiving placebo became asymptomatic at the study end.17
EFAs are beneficial in improving the signs and symptoms of dry eye. One study involved 76 females who reported contact lens-related discomfort. They were randomized to receive either 50mg of GLA from evening primrose oil (EPO) per day or a placebo. The researchers found significant improvements in dryness symptoms and lens comfort, as well as an increase in tear meniscus height in the treatment group.18
This research indicates that nutrition plays a significant role in tear film health, the management of dryness symptoms and the comfort of contact lens wear. Ocular nutrition for dry eye is available in a number of commercially available forms that are designed to optimize tear film health and, ideally, improve contact lens comfort. A good resource on ocular nutrition can be found at:
www.dryeyezone.com/encyclopedia/omega3.html. Discuss nutrition options and their benefits when talking to contact lens patients complaining of dry eye.
1. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001 Oct;119(10):1417-36.
2. Kaushik S, Wang JJ, Flood V, et al. Dietary glycemic index and the risk of age-related macular degeneration. Am J Clin Nutr. 2008 Oct;88(4):1104-10.
3. Belch JJ, Ansell D, Madhok R, et al. Effects of altering dietary essential fatty acids on requirements for non-steroidal anti-inflammatory drugs in patients with rheumatoid arthritis: a double blind placebo controlled study. Ann Rheum Dis. 1988 Feb;47(2):96-104.
4. Odabasoglu F, Halici Z, Aygun H, et al. a-Lipoic acid has anti-inflammatory and anti-oxidative properties: an experimental study in rats with carrageenan-induced acute and cotton pellet-induced chronic inflammations. Br J Nutr. 2011 Jan;105(1):31-43.
5. Calder PC, Yaqoob P. Understanding omega-3 polyunsaturated fatty acids. Postgrad Med. 2009 Nov;121(6):148-57.
6. Brenna JT, Salem N Jr, Sinclair AJ, Cunnane SC. Alpha-Linolenic acid supplementation and conversion to n-3 long-chain polyunsaturated fatty acids in humans. Prostaglandins Leukot Essent Fatty Acids. 2009 Feb-Mar;80(2-3):85-91.
7. Shapiro AC, Wu D, Meydani SN. Eicosanoids derived from arachidonic and eicosapentaenoic acids inhibit T cell proliferative response. Prostaglandins. 1993 Mar;45(3):229-40.
8. Hawkes JS, James MJ, Cleland LG. Separation and quantification of PGE3 following derivatization with panacyl bromide by high pressure liquid chromatography with fluorometric detection. Prostaglandins. 1991 Oct;42(4):355-68.
9. Quoc KP, Pascaud M. Effects of dietary gamma-linolenic acid on the tissue phospholipid fatty acid composition and the synthesis of eicosanoids in rats. Ann Nutr Metab. 1996;40(2):99-108.
10. Bray MA. Leukotriene B4: an inflammatory mediator with vascular actions in vivo. Agents Actions Suppl. 1982;11:51-61.
11. Hurst S, Rees SG, Randerson PF, et al. Contrasting effects of n-3 and n-6 fatty acids on cyclooxygenase-2 in model systems for arthritis. Lipids. 2009 Oct;44(10):889-96.
12. Antueno RJ, de Bravo MG, Toledo J, et al. In vitro effect of eicosapentaenoic and docosahexaenoic acids on prostaglandin E2 synthesis in a human lung carcinoma. Biochem Int. 1989 Sep;19(3):489-96.
13. Relief for Dry Eye: BioTears First. Available at:
www.biosyntrx.com/products/biotears.php (Accessed January 2010).
14. Aragona P, Bucolo C, Spinella R, et al. Systemic Omega-6 Essential Fatty Acid Treatment and PGE1 Tear Content in Sjogren’s Syndrome Patients. Invest Ophthal & Vis Sci. 2005 Dec;46(12):4474-9.
15. Barabino S, Rolando M, Camicione P, et al. Systemic linoleic and gamma-linolenic acid therapy in dry eye syndrome with an inflammatory component. Cornea. 2003 Mar;22(2):97-101.
16. Pinna A, Piccinni P, Carta F. Effect of oral linoleic and gamma-linolenic acid on meibomian gland dysfunction. Cornea. 2007 Apr;26(3):260-4.
17. Wojtowicz JC, Butovich I, Uchiyama E, et al. Pilot, Prospective, Randomized, Double-masked, Placebo-controlled Clinical Trial of an Omega-3 Supplement for Dry Eye. Cornea. 2010 Oct 28. [Epub ahead of print]
18. Kokke KH, Morris JA, Lawrenson JG. Oral omega-6 essential fatty acid treatment in contact lens associated dry eye. Cont Lens Anterior Eye. 2008 Jun;31(3):141-6.


