 |
The available technology for fine-tuning scleral lens fits has become more advanced throughout the years. As someone who has been fitting a high volume of scleral lenses since the beginning of my career in 2011, seeing this evolution has been exciting. In the beginning, all we had to base our fits on were spherical diagnostic sets and fluorescein patterns. Now, we have anterior segment optical coherence tomography, scleral topographers, the ability to take impressions of a patient’s eye and newer designs that incorporate our increasing knowledge of the scleral shape.
The following case highlights a patient whose initial scleral lens fitting required multiple visits to ensure the right lens parameters were ordered. She returns a few years later and, with innovative, new technologies, is refit with new lenses in significantly less chair time.
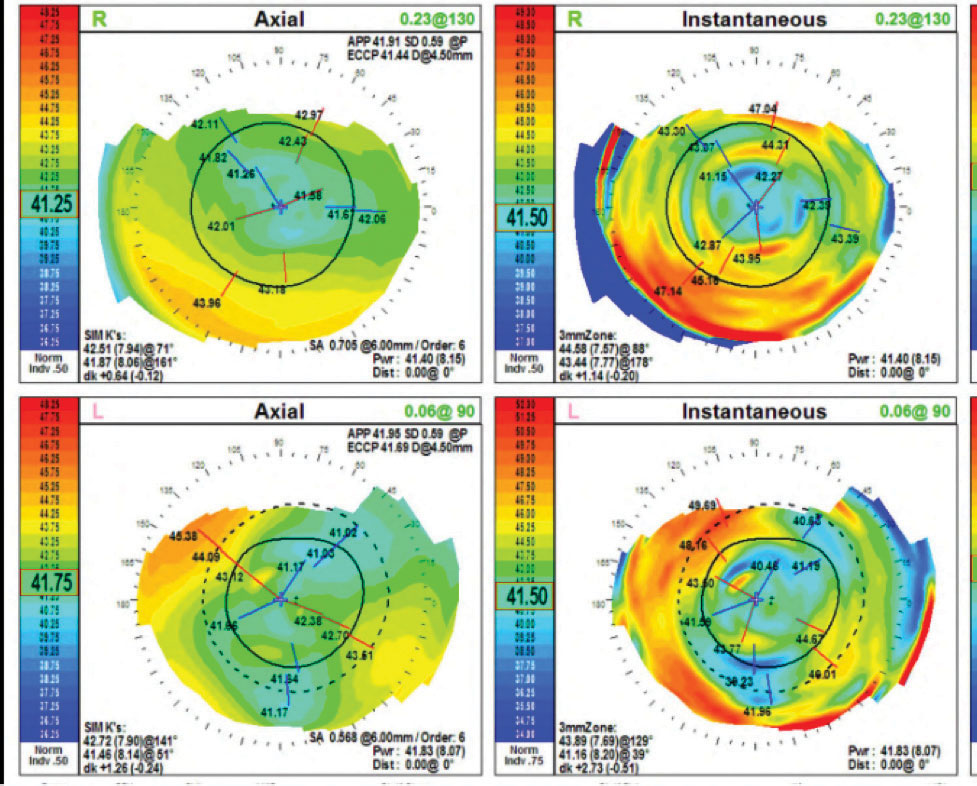 |
| Fig. 1. Pictured here is a plateau-shaped corneal topography OU. |
The Case
A 62-year-old female with corneal ectasia OU secondary to LASIK surgery presented complaining she did not want to have to wear glasses over her contact lenses at the same time to correct her residual astigmatism. She had not had an eye exam in three years and was wearing the same lenses that had been prescribed for her previously. The lenses were comfortable, and her vision was clear, but wearing both scleral lenses and glasses to correct her astigmatism was frustrating for her.
Three years ago, we went through many iterations of scleral lenses with front surface toric optics that were weighted with prism ballast. However, her vision was constantly fluctuating, and her over-refraction was inconsistent. My lab at the time was unable to make back surface toric haptics to stabilize the lens, so the toric markers were at different locations during each of the patient’s visits, regardless of the amount of prism ballast that was added. Eventually, I ended up ordering spherical lenses and forward spectacles to correct the patient’s astigmatism.
Her presenting visual acuities (VA) were 20/20 OD and 20/20 OS. Her scleral lenses had a base curve (BC) of 44mm OU, a sagittal depth (sag) of 4.48mm OU, a diameter of 16mm OU and powers of -2.50D OD and -2.00D OS. Her glasses prescription was -0.75+0.50x175, add +2.50 OD and -1.75+1.25x153, add +2.50 OS.
 |
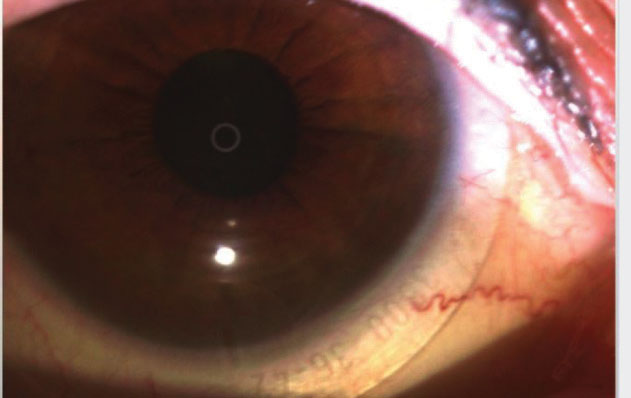
| Fig. 2. The toric marker in this eye is aligned to 7:30 clock hour OS. |
Contact Lens Evaluation
The patient’s pupils were equal, round and reactive to light. I did not note any relative afferent pupillary defects in either eye. Her extraocular movements were full OU. A slit lamp exam revealed clear lashes OU, clear corneas with low tear lakes OU and deep and quiet anterior chambers OU. I noted 1+ nuclear sclerosis OU. The patient’s intraocular pressure was 15mm Hg OU. Topography showed plateau-shaped corneas with mild inferior ectasia OU. Her keratometry readings were 42.51/41.87@071 OD and 44.58/43.44@088 OS (Figure 1). An undilated posterior segment evaluation revealed a healthy fundus OU.
Contact Lens Fitting
The SynergEyes VS is a scleral lens that comes standard with toric haptics to stabilize it. These lenses are non-rotationally symmetrical and use bitangential peripheral landings that rest gently on the sclera and respect the natural contour of the scleral shape. This design also achieves better centration, improving optics and fits.1 A fitting set of this design was chosen to refit the patient with the hopes of stabilizing her forward astigmatism correction.
The initial diagnostic lens was placed on the patient’s eyes with parameters of 3600 sag/plano/16.0 haptics, 36/42 OD and 3600 sag/plano/16.0 haptics, 34/40 OS. Centrally, the sag was adequate with about 250µm of central clearance OU after initial insertion, there was adequate limbal clearance and the haptic sat nicely aligned OD, but the left lens had 360 slight edge lift, causing the patient to feel that lens a lot more.
Over-refraction revealed:
- +0.50 +0.75x170 (VA of 20/20) OD (toric marker line at 5:30 clock hour)
- +0.50 +1.00x155 (VA of 20/20) OS (toric marker line at 7:30 clock hour)
The axis was adjusted to accommodate the position of the toric markers per the lab’s formula, and the following lens parameters were ordered: +1.25-0.75x155 OD and +1.50-1.00x155 OS. The lenses had a sag of 3600, a BC of 8.4mm, a diameter of 16mm and toric haptics of 36/42.
 |
| Fig. 3. The toric marker in this eye is aligned to 5:30 clock hour OD. |
Contact Lens Dispensing
Two weeks later, I placed the lenses on the patient’s eyes. Her vision was 20/20 OU. The fit was optimal with 200µm of central vault upon settling. The toric line was aligned at the expected positions—5:30 OD and 7:30 OS (Figures 2 and 3). Over-refraction was plano OU. The lenses were dispensed.
Follow-up
Two weeks later, the patient presented and reported she was thrilled with her vision. She could clearly see objects further away without her glasses and was able to enjoy a more active lifestyle. The fit was finalized.
Discussion
Stabilizing front surface toric optics with toric haptics is a lot more predictable, comfortable and effective than with prism ballast.2 Allowing the lens to settle in its natural place causes the toric haptic lines to land where they are expected to every time. Toric haptics can also improve centration of lens optics, reducing induced cylinder from a decentered lens.
Prism ballast, on the other hand, can add thickness to the lens, making edge awareness more prevalent in patients. It is also not as secure as a toric haptic. In addition, prism ballast lenses tend to rotate, especially if a patient has a non-spherical sclera, which is true of most patients.3,4
The SynergEyes VS lens design has helped me fit front surface astigmatism scleral lenses more confidently in less chair time, making these scleral lenses valuable in my practice.
1. Hellem A. A lens designed to fit true scleral shape. blog.synergeyes.com/blog/a-lens-designed-to-fit-true-scleral-shape. Accessed October 1, 2018. 2. Johns LK, Barnett M. Contemporary scleral lenses: theory and application. Bentham Science. 2017. 3. Van der Worp E, Graf T, Caroline PJ. Exploring beyond the corneal borders. Contact Lens Spectrum. 2010;6:26-32. 4. Visser ES, Visser R, Van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006;83(4):233-6. |


