Fitting a customized contact lens can be a rewarding experience. By combining empirical data and clinical expertise, specialty lenses can be designed for nearly any refractive state or ocular condition. However, the fitting process is not without challenges. Fortunately, contact lens manufacturers are armed with highly trained consultation teams available to offer their assistance when needed.
We reached out to consultants from multiple gas permeable (GP) lens manufacturers to seek their advice and perspectives on how to cultivate a relationship and maximize their expertise. We have also assembled a consensus of their suggestions for how to best streamline the contact lens fitting process.
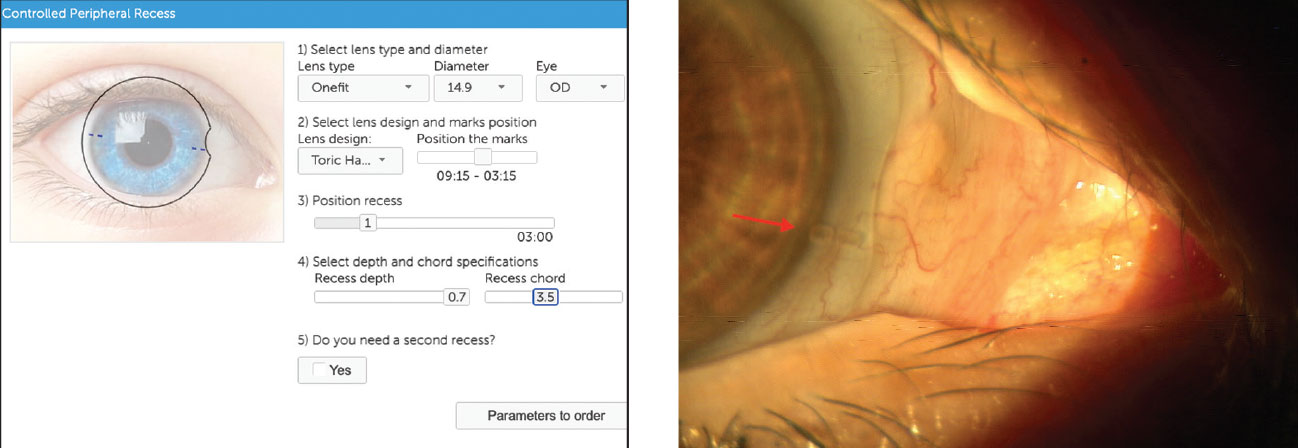 |
| Blanchard’s CPR tool helps visualize the lens and can be used to populate lens parameters (left). At right, the ordered lens displays toric markings, which are important to note prior to making any haptic changes. Click image to enlarge. |
Same Old Story
When polling the labs regarding their interactions with optometric practices, many had similar responses. Below we have included some commonly asked questions, along with answers provided by various consultants from different lens manufacturers.
What do ODs ask labs about the most and how do the design consultants help them?
- Advice on selecting designs and materials. “What designs work best for a particular disease? Lid anatomy, topography, the patient’s lens history and motivations are very helpful before making a suggestion. Wearing habits, occupational visual needs and patient history can also be very valuable. Knowing the problem helps design lenses that will work the best. However, ECPs also need to understand that there is no single lens design that will magically provide the optimum outcome for every situation.”
- How to handle limbal zone changes. “They usually need to increase the limbal clearance in some areas without getting excessive limbal clearance in other areas. With quadrant-specific designs, this allows us to design and customize lenses accordingly. Also, incorporating oval optic zones into the lens design to accommodate for the asymmetrical nature of the limbal zones has provided great improvement.”
What are common problems labs face when they don’t get good feedback from an OD?
- Lack of and/or low quality information. “Many times consultants only receive Ks and refraction—not enough information to design a specialty lens. Having complete and accurate information will allow consultants to design the best lenses for the patient.”
- Note locating lens marking.“When doctors place an order and need adjustments in some areas, they often forget. We either must guess it or, in some cases, they must get the patient back in the office for an accurate assessment.”
- Only relying on one diagnostic modality. “They can rely too much on optical coherence tomography (OCT) alone and fail to assess the lens under a slit lamp.”
- Not having good quality mappings. “Better and more complete maps give us the information needed to make an educated decision on what design will work best for the patient and what parameters are appropriate.”
What would lab design consultants like ODs to know when they put in an order?
- The more information we have, the better the lenses will fit. “Previous orders, K reading, maps, photos, trial lenses—all can help us to design a better lens for their patient.”
- Take time and navigate through the trial set if the first lens did not work well. “The other trial lenses might have the perfect fit or might have been a much better starting point if they had only tried them on.”
When ODs are doing their initial design, what do labs emphasize not to forget?
- Lens parameters. NaFl patterns, horizontal visible iris diameter (HVID) or any pertinent information that is available.
- The location of any laser markings on the lens. “Toric markings are important for haptic changes and astigmatism correction and helps the consultant make changes to the lens’s fit and power.”
- Trial lens. “Document which trial lens was used to assess the fit.”
What can ODs do so that the lab can ensure adequate fit and eliminate as many initial issues from their end?
- Manipulate the lens on the patient eye with their thumb. “Scleral lenses tend to decenter down and out, and if the OD is able to move the lens and center it better, that will be important information to give to the consultant in order to suggest the proper change.”
- Submit a comprehensive list of items with order. This should include:
- Accurate K readings and refraction
- Topographies, when available
- Patient history, e.g., Is the patient post-surgery? Do they have an IOL?
- Previous lens history
- Patient expectations
- Slit lamp photos, when available
- OCT images, when available
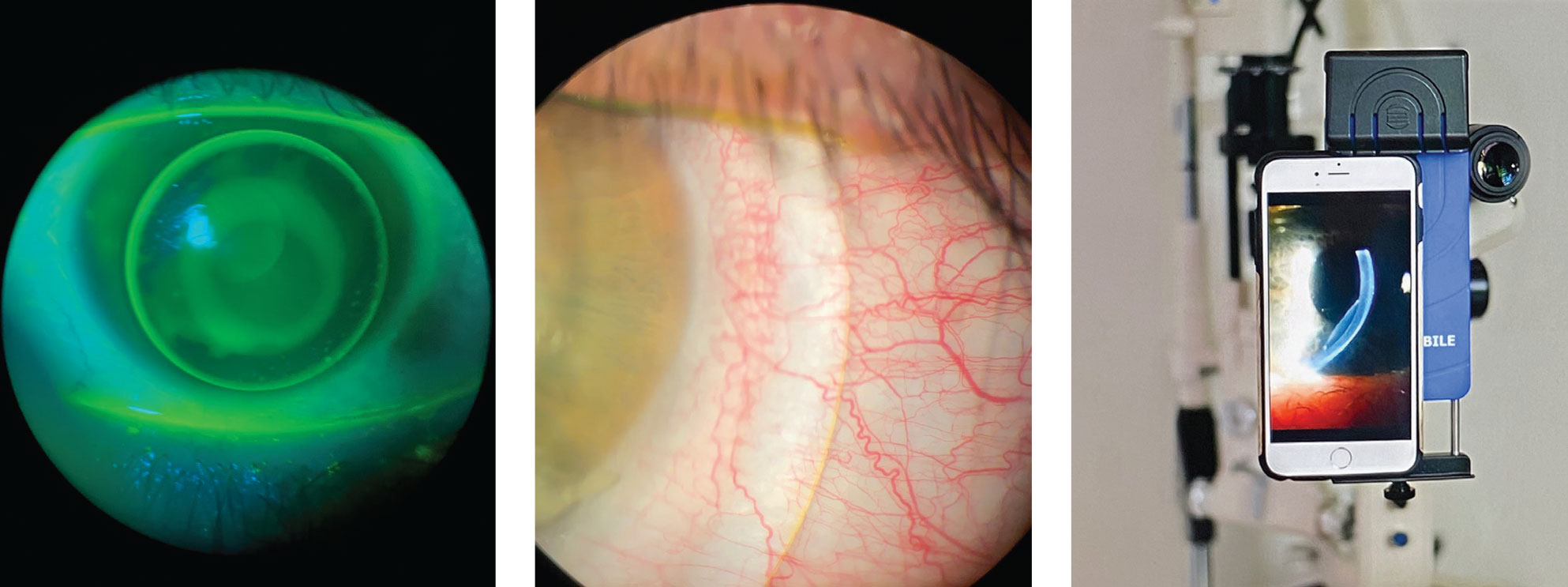 |
| An iPhone and adapter at the slit lamp (right) is an option when taking images of troubleshooting issues. This is an easy way for doctors to send photos and videos to consultants directly. Click image to enlarge. |
Open Communication
Whether you are a recent graduate or a seasoned contact lens fitter, there should be no hesitation to reach out to the laboratories when necessary. Besides the traditional fax and phone options, many laboratories now have online portals and encourage the use of email communication. This allows for greater flexibility to work around clinic and office hours.
When no assistance is required, online portals are simple and convenient enough for either the practitioner or trained staff to input lens data or upload files. In other cases, the lab’s feedback may be desired, and an email may be more appropriate. If possible, reach out to a specific consultant with whom you have a comfortable working relationship.
When emailing, we highly encourage providing account numbers, previous invoice numbers and shipping information to save time. Laboratories aren’t responsible for your record-keeping; rather, it’s incumbent upon you to maintain a careful log of your previous orders to help prevent any ordering errors.
Concise, consistent communication makes it easier for consultants to determine what is needed. If ordering for both eyes, start with the right eye and provide the pertinent information before moving to the left eye. A lens evaluation is welcomed, but terms like “tight” or “loose” may lack context. For example, describe a “tight” scleral lens by detailing where the conjunctival compression is located and if there is heel or toe blanching.
Units of measurement can be helpful, but keep them consistent along with the formatting for providing lens parameters. For instance, describing a lens’s sagittal depth as “good” and limbal clearance as “adequate” is not as useful as stating there is 200µm of apical clearance and 50µm of limbal clearance.
Of course there’s no such thing as too much information when it comes to providing data to the laboratory. Corneal topographies provide more information regarding corneal curvature and condition than Ks alone. Pictures or video of the lenses on the eye can help as well.
If you don’t have an imaging system at hand, most phone cameras have high enough resolution to take quality photos for the lab with the aid of an adapter. These options allow the consultant to remotely view the lens even while the patient is in the chair. Anterior segment OCT can also supplement a lens evaluation, showing both the sagittal depth of the lens as well as the lens edge in order to provide a better visual of just how much or how little change is required.
Gathering Data
As one lab consultant told us, “ODs need to treat the patient as an individual and gather both clinical and lifestyle information as well as the patient’s expectations in order for consultants to be able to effectively assist in optimizing the design process.”
Before ordering any specialty contact lenses, learning more about the patient and their objectives is a critical factor for success. What are their needs and goals? Are there any lifestyle considerations? How often will they wear them? Do they need to be wearing them for their job? Do they have any history of contact lens wear that was either successful or a failure?
For example, if a patient desires crisp, stable optics at both distance and near but has not had success with an aspheric GP multifocal, it makes sense to consider a translating design. Although these lenses may be best fit diagnostically, empirical fitting is possible. However, sending only keratometry measurements and refraction to the laboratory will result in guesswork during lens design. Clarifying lens design as well as providing data such as pupil size, HVID), aperture size and eyelid position are pertinent for initial lens design.
Of course, careful evaluation of the ocular anatomy is also important when considering different lens designs. For GP lenses, upper eyelid position is a primary consideration for choosing lens diameter. If lid attachment is not possible, then consider a smaller interpalpebral fit. Similarly, lower eyelid position is critical for the success of translating GP multifocals.
When considering larger design lenses, like sclerals, evaluate aperture size and eyelid laxity. Small aperture or tight eyelids might make application and removal difficult. Tight or heavy eyelids can also contribute to lens decentration. Conjunctival abnormalities like cysts or pterygia can make scleral lens fitting more complex, often requiring higher levels of peripheral customization. Knowing the availability and limits of the design options for your scleral lens of choice is essential before starting a fitting.
Topographical analysis, especially for irregular corneas, can be used to understand size and shape of the cornea. Although not its primary use, most topography systems measure HVID, which plays a role in determining scleral lens diameter and hybrid lens skirt curves. Identifying the steepest and flattest points on the cornea will help you choose between prolate or oblate design lenses. Location of the steepest point of an ectatic cornea can also help you choose lens designs and diameters. Corneas with large elevation differences may also be difficult to fit with corneal GPs and require a scleral lens.
When sending refractive data for especially higher-powered lens orders, make sure it is clearly known if the power has already been vertexed. If a spherocylindrical over-refraction is found, lens flexure must be ruled out, and the decision to incorporate front surface toric power may be dependent on lens stability. In these cases, noting the lens markings at every visit is mandatory to ensure the lens is stabilized prior to incorporating the power in the lenses. Discussing subjective quality of vision at all working distances can help determine if zone size or centration should be modified.
Tips for Troubleshooting
Once a lens is ordered, there may be challenges that arise related to vision, lens fit or comfort. When attempting to troubleshoot a concern, it is important that the practitioner helps the lab consultant clearly understand the issue or objective. When describing a lens fit to a consultant, be more descriptive with the exact location of the issue and lens markings.
The capability to easily pass along photos and videos of the lens’s on-eye performance has greatly assisted our troubleshooting efforts. Videos tend to be more helpful than a single image since the movement of the lens is important as well as the lens position. OCT images don’t necessarily show us where there might be blanching.
In some cases, the OCT image of the landing looks ideal, but upon slit lamp examination, we might see mild blanching or redness. In other cases, the edge appears to be digging in, and we might assume there is blanching, but then slit lamp evaluation reveals that the patient has redundant conjunctiva and blanching is not present. This does not mean the landing won’t be altered; it simply means that it might be altered in a different way. Another example is that when a single OCT cross-section is taken along the 180º meridian, it can completely miss the elevated area of a cone in a patient with keratoconus or other ectasia. We recommend, if possible, taking both a 0º to 180º cross-section along with a 270º to 90º cross-section.
Lid structure could be the culprit of poor contact lens performance. Always make sure to retract the eyelids at the microscope to evaluate how a lens is sitting on the cornea in the absence of lid involvement. Verify if the fit is related to the lens or if the lid is creating a difference in lens alignment. Maybe the lens sits central in the absence of eyelid interaction, but interacting with the eyelid pushes the lens or causes it to ride high. Some ways to adjust for this could be changing the center thickness of the lens and modifying the edge profile. A floppy lid might need an increase in lens edge in order to grab the lens upon blinking. You can avoid making excessive parameter changes if you determine that the lid is manipulating lens alignment.
A patient’s description of what they feel is happening can help guide any changes, especially when everything might objectively look great. Comments like, “I feel the lens over here,” “I tip my head up to see better,” “It feels like a pressure or tightness” and “It’s like looking through a tunnel,” all detail the lens fit or the optics of the lens. If a patient reports vision changing with blinking, this could indicate either poor lens alignment or a wetting issue with the lens material. If you look at the lens surface behind the slit lamp and notice the material is not wetting well, tell the lab consultant so they can consider a different lens material with a different wetting angle or add a coating such as Tangible Hydra-PEG for increased lubricity.
Custom specialty contact lenses are a fantastic service to provide for our patients. Using the expertise of consultants from various lens manufacturers is both beneficial and can help streamline the contact lens fitting process. Patient history and thorough data collection is critical during a contact lens exam. So are capturing images and recording videos whenever possible.
Consider setting up a weekly time to discuss patient cases and lens orders with your consultant. Depending on your contact lens volume, setting up a standing appointment for a weekly or biweekly meeting with your laboratory consultant may be beneficial whether it be by phone or video call. Whichever method you choose, ultimately, clear communication is key.
Thank you to our consultants from ABB Optical Group, Valley Contax, Alden Optical, BostonSight, Blanchard, Art Optical and TruForm Optics for contributing to this article and providing valuable insight on how to improve the GP lens ordering experience.
Dr. Miller is a principal optometrist at UC Davis Eye Center in Sacramento, CA. She is president of the Sacramento Valley Optometric Society, a Fellow of the American Academy of Optometry, a Fellow of the Scleral Lens Education Society and an advisory board member of the Gas Permeable Lens Institute.
Dr. Ensley practices at Gaddie Eye Centers in Louisville, KY. He is an advisory board member of the Gas Permeable Lens Institute and serves on the board of the Scleral Lens Education Society.


