 |
A 39-year-old male presented with tearing, redness and pain in his right eye. He denied any trauma or previous injury to his eye but did report irritation and dryness about two to three days prior. After a detailed history, he did not report having a similar incident in the past and noted that the foreign body sensation and irritation was not alleviated with use of OTC Visine (tetrahydrozoline, Johnson & Johnson) drops.
Upon examination, a linear abrasion was found inferiorly on the cornea outside the visual axis. The patient was diagnosed with a corneal abrasion and instructed to use antibiotic drops (ofloxacin 0.3%) TID to prevent infection of the open wound and lubricants for any irritation or discomfort. He was asked to follow-up one week or sooner with any worsening of symptoms. He returned in one week with a clear and healed cornea with no epithelial defect noted. He discontinued the antibiotic and was instructed to continue using lubricants as needed.
Two months later he presented with similar symptoms of pain, redness, tearing and areas of negative staining with minor breaks in the epithelium, consistent with epithelial microcysts, in the inferior region of the cornea. He was diagnosed with recurrent corneal erosion; flare-ups continued to occur over several weeks. Treatments included bandage contact lens (BCL) placement, Acuvue Oasys (8.8/14.0) (Johnson & Johnson) with the antibiotic ofloxacin 0.3% QID during the acute phase to prevent infection and again, lubricants throughout the day for comfort. The patient was asked to follow-up in three days. Once the epithelium was healed and the BCL was removed, he was instructed to start Muro 128 5% ointment (Bausch + Lomb) at night and to use Lotemax (loteprednol etabonate, Bausch + Lomb) BID OD.
Recurrences took place over the course of several weeks and months. A longer-term treatment of a BCL was tried with antibiotic ciprofloxacin QID for three weeks with close monitoring and weekly follow-ups. Two weeks later, another recurrence happened. Conservative therapy options proved ineffective and discussion regarding other treatment options, including amniotic membrane placement, superficial keratectomy Diamond burr debridement and phototherapeutic keratectomy, was had, before ultimately deciding on undergoing phototherapeutic keratectomy, which occurred without complications.
After treatment at his one month follow-up, the patient was doing well without any further complications or recurrences.
Recurrent Corneal Erosions (RCEs)
These are frequently encountered in practice and characterized by basal epithelial cells that do not attach to the basement membrane, resulting in abrasions. Damage to the epithelium or epithelial basement membrane can result from previous instances of trauma or abrasions (e.g., sharp abrasion from a fingernail, tree branches or paper edge cuts), corneal dystrophies and degenerations or prior surgeries where the corneal epithelium has been removed (i.e., corneal transplantation, epi-off crosslinking, cataract surgery and keratorefractive surgery).
In healthy patients, the injuries usually heal quickly if they are superficial enough, leaving the cornea without evidence of damage during clinical examination. Symptoms tend to recur over the course of days but can even persist for years, resulting in chronicity. These include acute ocular pain, foreign body sensation, tearing and photophobia.
Diagnosing an RCE requires a detailed history and careful slit lamp exam. There is often a history of prior abrasion of the involved eye and pain usually occurs immediately upon waking or in the middle of the night. Clinical presentation may not correlate to the exam findings, thus it is important to look for subtle corneal changes, like areas of negative staining that highlight loose epithelial adhesion. Other changes could take the form of epithelial microcysts, visible with retroillumination, areas of sodium fluorescein pooling around the affected area or use of a Weck-Cel spear to confirm areas of loose adhesion. Shahinian’s sign (corneal valance) is noted in epithelial basement membrane dystrophy, which is described as a “scalloped line of tear film thinning” seen in the slit lamp with use of NaFl dye and cobalt blue filter.1
Episodes can vary in duration and intensity of pain associated with the epithelial defect. Some can last as little as 30 minutes and improve with use of artificial tears, while larger abrasions can leave the patient with intense pain, eyelid edema and decreased vision.
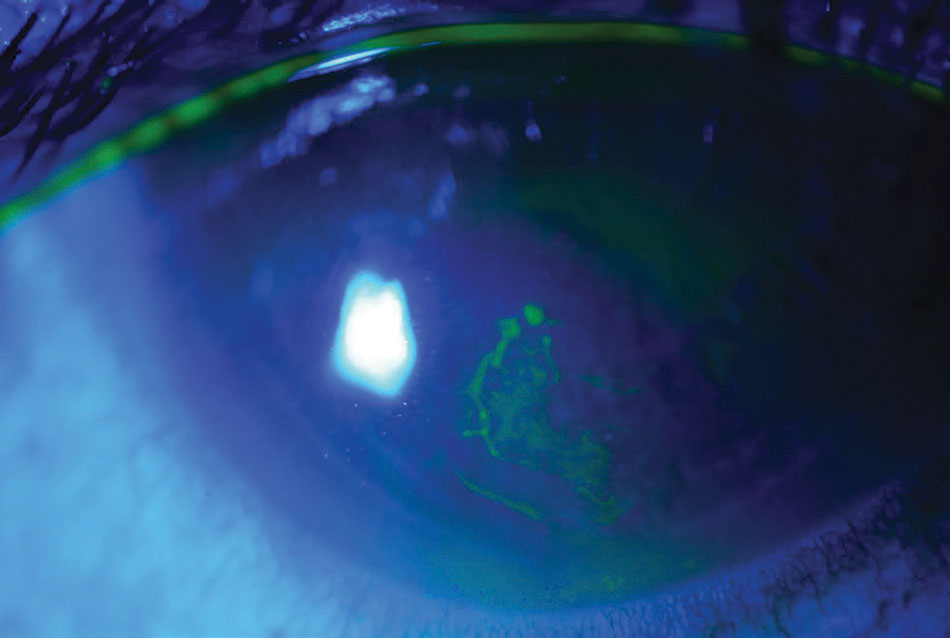 |
| A macroform erosion with loosely adherent epithelium is highlighted with NaFl staining. Photo: Rebecca Rojas, OD. Click image to enlarge. |
Differential diagnosis of RCEs include herpes simplex virus, epithelial keratitis, neurotrophic keratitis, exposure keratopathy, infectious corneal ulcers, trauma and scratches, leading to corneal abrasions and ocular graft-versus-host disease.2
Topical Therapeutics
Treatment for RCEs varies depending on the severity of the erosion and symptoms experienced. The primary goal is to relieve pain and provide re-epithelialization, while the long-term goal is to prevent recurrences. Conservative treatment includes topical lubricant gel or ointment at night with topical cycloplegics and oral analgesics for pain control. A BCL helps smooth out epithelial areas with corneal irregularities and allows for better cell adherence, while antibiotic drops help reduce the risk of secondary infection. When using BCLs, make sure there is high DK (oxygen transmissibility) and adequate fit and movement of the lens. Long-term use of antibiotics should be monitored carefully and not used for extended periods of time.
Patients with ocular rosacea or meibomian gland dysfunction (MGD) causing chronic dry eye are more at risk for erosions and improper healing because of free fatty acids found in their tear secretions. They may benefit from punctal plug occlusion for either temporary or long-term prophylactic treatment, effectively increasing the lacrimal lake and aiding in dry eye.1
Patients with diabetes also suffer from corneal complications impacted by trauma and delayed wound healing, resulting in recurrent erosions to neurotrophic keratopathy. Recovery time varies and should incorporate comanagement with the patient’s endocrinologist.3
Other forms of treatment include a combination of topical steroids with a dose of oral doxycycline.4 Increased levels of matrix metalloproteinase (i.e., MMP2 and MMP9) have been found in tears of patients with RCEs. These enzymes cause a separation in the epithelial layer by dissolving the basement membrane and fibrils from hemidesmosomes. Therefore, the use of MMPase inhibitors has been studied as another form of treatment. Doxycycline is an MMP9 inhibitor which, along with corticosteroids, is effective in reducing frequency of RCEs.5 This combination therapy has been specifically helpful to patients with associated MGD because it helps lower the production of lipase, which affects the healing and quality of epithelial membranes.4
Autologous serum tears have been effective by providing lubrication along with essential nutrients and growth factors to help promote epithelial healing, including cytokines, vitamin A, epithelial growth factor, vitamin C and fibronectin.4,6 Studies have confirmed successful treatment of RCEs for 12 to 24 month periods without recurrences after use of autologous serum tears.7
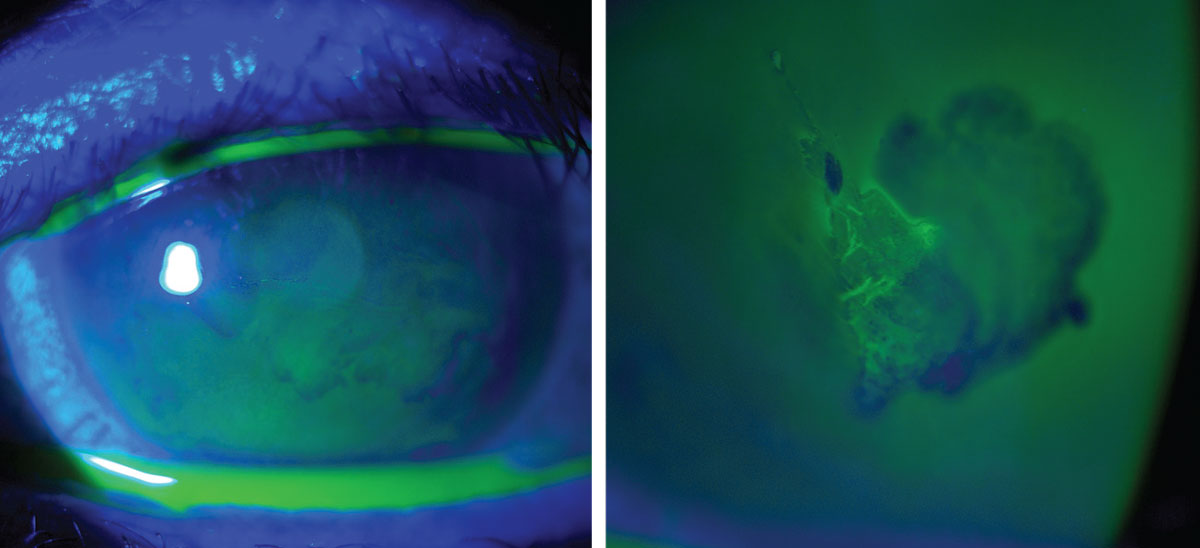
Amniotic membrane placement over debridement of loose epithelial tissue results in epithelialization within four to seven days, as it reduces inflammation and promotes healing.8 Areas of loose epithelial tissue benefit from mechanical debridement to provide a smooth area for re-adherence. One of the quickest and most effective ways is to debride loose tissue at the slit lamp. This is done with use of one drop of topical proparacaine and ophthalmic instruments or sponges to debride and remove excess debris. Tools used range from Weck-Cel spears, shaped methylcellulose surgical sponges, blunt spatulas and jeweler’s forceps.9
 |
|
An erosion that is healing after a successful use of a Prokera graft. Photo: Suzanne Sherman, OD. Click image to enlarge. |
Surgical Interventions
When other treatments fail, surgical intervention is warranted. Diamond burr superficial keratectomy is performed on patients who have erosions that are on or near the visual axis, while anterior stromal puncture is considered for erosions outside the visual axis. This is because anterior stromal puncture has been shown to produce glare, scarring and blurred vision, while only providing moderate efficacy in preventing erosions.9
Anterior stromal puncture can be performed using a needle or laser providing injury to Bowman’s membrane that results in better adherence to epithelium.9 Diamond burr superficial keratectomy has a higher success rate than anterior stromal puncture, with the advantage of avoiding the use of lasers or sophisticated equipment. Other advantages of superficial keratectomy include decreased risk of corneal perforation, scarring or refractive changes and less recurrences than epithelial debridement alone.10
Phototherapeutic keratectomy (PTK) is used on patients who suffer from micro- or macroerosions secondary to ocular trauma when conventional therapy has failed. PTK can also treat areas near the visual axis; however, inducing refractive changes may be more likely to occur than in other treatment modalities, especially with the use of older lasers or deeper ablation.11 Despite this possibility, all surgical interventions are performed with a high success rate because it allows the epithelium to heal and re-epithelialize by adhering to the basement membrane with a stronger bond, preventing recurrences.
Non-surgical Intervention
A newer modality cited in literature is use of scleral contact lenses for RCEs or persistent epithelial defects. These therapeutic lenses are effective in promoting the healing of defects that have failed with topical or surgical intervention. The healing response is attributed to oxygenation of the corneal epithelium and protection of the epithelium during recovery.12
Corneal erosions can be debilitating for the patient when they have recurrent episodes with pain that interrupts their ability to sleep or continue with their daily activities. There are several treatment options available to alleviate discomfort in the acute phase, but patient education is important to impart the necessity of compliance in determining the treatment modality for chronic cases. Advances in treatment have provided relief in reducing recurrences and allowing patients the ability to return to their normal lives. As clinicians, it is vital to closely monitor these patients and provide the proper referral for advanced surgical intervention when necessary.
1. Shahinian L Jr. Corneal valance: a tear film pattern in map-dot-fingerprint corneal dystrophy. Ann Ophthalmol. 1984;16(6):567, 70-1. 2. Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;(13):325-35. 3. Jan RL, Tai MC, Ho CH, et al. Risk of recurrent corneal erosion in patients with diabetes mellitus in Taiwan: a population-based cohort study. BMJ Open. 2020;10(6):e035933. 4. Wang L, Tsang H, Coroneo M. Treatment of recurrent corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clin Exp Ophthalmol. 2008;36(1):8-12. 5. Hope-Ross MW, Chell PB, Kervick GN, et al. Oral tetracycline in the treatment of recurrent corneal erosions. Eye. 1994;8:384-8. 6. Pan Q, Angelina A, Marrone M, et al. Autologous serum eye drops for dry eye. Cochrane Database Syst Rev. 2017;2(2):CD009327. 7. Ziakas NG, Boboridis KG, Terzidou C, et al. Long-term follow up of autologous serum treatment for recurrent corneal erosions. Clin Exp Ophthalmol. 2010;38(7):683-7. 8. Huang Y, Sheha H, Tseng SCG. Self-retained amniotic membrane for recurrent corneal erosion. J Clin Exp Ophthalmol. 2013;4(2):272. 9. Thakrar R, Hemmati HD. Treatment of recurrent corneal erosions. Am Acad of Ophthalmol. 2016;39-41. 10. Soong HK, Farjo Q, Meyer RF, Sugar A. Diamond burr superficial keratectomy for recurrent corneal erosions. Br J Ophthalmol. 2002;86(3):296-8. 11. Maini R, Loughnan MS. Phototherapeutic keratectomy re-treatment for recurrent corneal erosion syndrome. Br J Ophthalmol. 2002;86(3):270-2. 12. Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol. 2000;130(1):33-41. |


