While the world and the way we practice have changed since COVID-19, our patients’ vision needs still persist. Many individuals require ophthalmic devices to correct their refractive errors, and some rely on advanced ophthalmic products, such as scleral lenses, that can provide better visual outcomes and greatly improve a patient’s quality of life.
Sclerals hold the title as the first contact lens modality to enter the market. The lens was developed in 1887, and early designs were used to manage ocular surface disease.
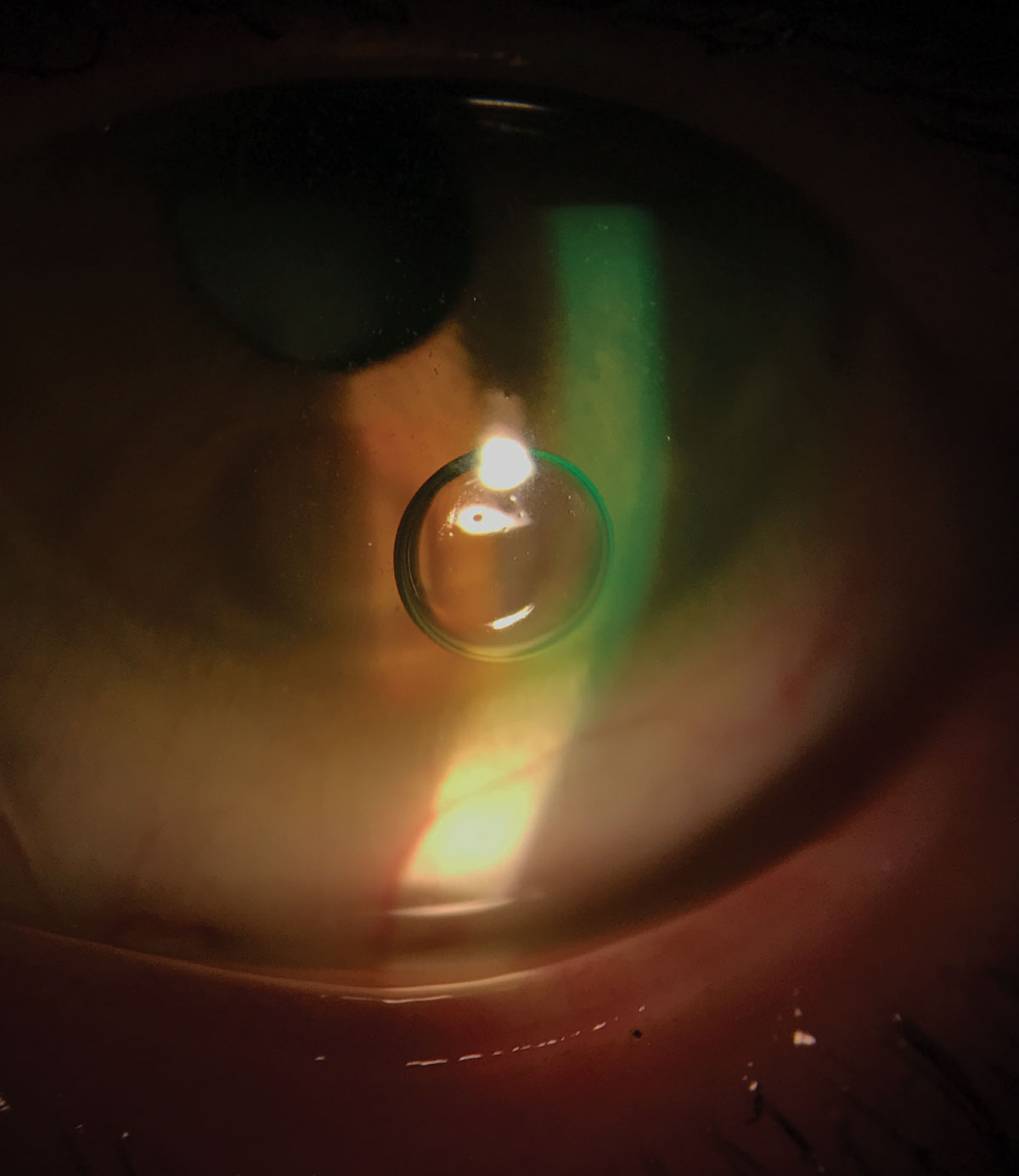 |
| Fig. 1. One common problem associated with scleral lens application is application bubbles. Photo: Melissa Barnett, OD. Click image to enlarge. |
Despite sclerals’ evolution through the decades, this modality didn’t become popular until the early 2000s due to problems mainly centered on technology. Older generations were impermeable to oxygen, designs were limited and little attention was given to this technology in the optometric curriculum, which made scleral lenses either unsafe or challenging to fit.1,2
Today’s sclerals have come a long way. Modern designs are gas permeable, highly customizable and are now commonly fit in nearly every mode of practice.1 Despite the advancements in this specialty lens category, clinicians still need to closely monitor a number of issues to ensure their patients have a safe and comfortable wearing experience.
1. Train Early and Often to Curb Contact Lens Dropouts
For new scleral lens wearers, the early adaption period can be challenging. One recent study found 27.4% of neophyte scleral lens wearers dropped out of their lenses within the first year mainly because of lens handling issues.3 In contrast, new soft contact lens wearers most frequently drop out of lenses due to poor vision.4,5 The difference between the two groups is likely due to sclerals’ unique designs. Scleral lenses typically have a larger diameter and are made of rigid materials. These attributes, combined with the lenses’ large size, often require the aid of devices, such as DMV inserters, for application.6
Despite these early challenges, clinicians can help their new scleral wearers adapt by closely monitoring them during the initial fitting period.6 Additionally, scleral lens training can help ensure patients will become successful wearers.
While scleral lens application may be easy for some, it can pose challenges for others, especially in individuals with dexterity limitations (e.g., motor issues secondary to a stroke or Parkinson’s disease).7
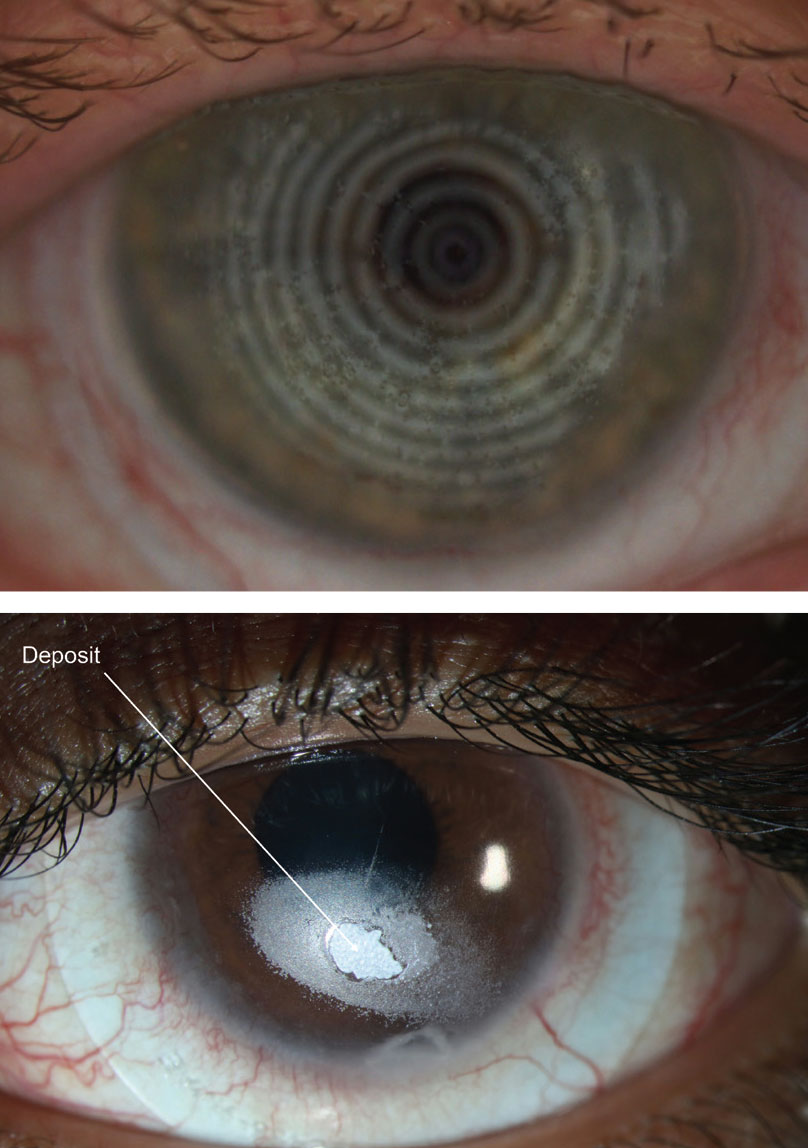 |
| Figs. 2 and 3. Deposits (distorted spots) might appear on a compromised scleral lens surface. Photos: Maria Walker, OD, and Gloria B. Chiu, OD. Click image to enlarge. |
One common problem associated with scleral lens application is application bubbles, especially when patients are first learning how to apply the lenses (Figure 1).7 While very small bubbles may not be cause for concern, larger bubbles can result in visual disturbance or ocular discomfort in the event the bubbles get trapped in the lens fluid reservoir. If a bubble begins to form after lens application, a peripheral lens adjustment (e.g., steeper peripheral edge, quadrant-specific lens, freeform lens) is likely needed to better align the lens edge with the sclera. A smaller lens may be needed to avoid the surface toricity associated with the peripheral sclera. Applying a non-preserved artificial tear to the lens bowl prior to lens application can also help avoid bubbles that form throughout the day.
2. Preach Proper Lens Care from the Get-Go
For inexperienced scleral wearers, improper lens care can also pose problems, including corneal toxicity caused by products such as hydrogen peroxide–based solutions.8,9Therefore, clinicians should regularly educate patients on how to correctly use their care regimens.9 Commonly prescribed care systems for sclerals include Clear Care (Alcon), Boston Simplus Multi-Action Solution (Bausch + Lomb), Boston Advance (Bausch + Lomb), Advanced Comfort Formula System (Bausch +Lomb) and Tangible Clean Multipurpose Solution (Tangible Science).
Poor lens wetting is a problem for both new and veteran wearers.10 The Scleral Lens Assessment by Patients and Practitioners (SLAPP) study group found poor lens wetting was one of the main issues practitioners noticed in their scleral lens patients.10 When poor lens wetting occurs, practitioners should instruct the patients to remove, clean and then reapply their lenses.10
Clinicians can also tackle this problem by recommending a Tangible Hydra-PEG (Tangible Science) lens coating.11 Hydra-PEG consists of a 90% water polyethylene glycol-based polymer mixture that permanently encapsulates the lens and helps with wettability issues.
If a patient is wearing a lens coated with Hydra-PEG, practitioners should advise them to only use care products approved for this specific technology since rinsing them in water or using non-approved brands may prematurely remove the coating.11 In addition to improving wettability, Hydra-PEG may also reduce deposits on the scleral lens (Figures 2 and 3).11
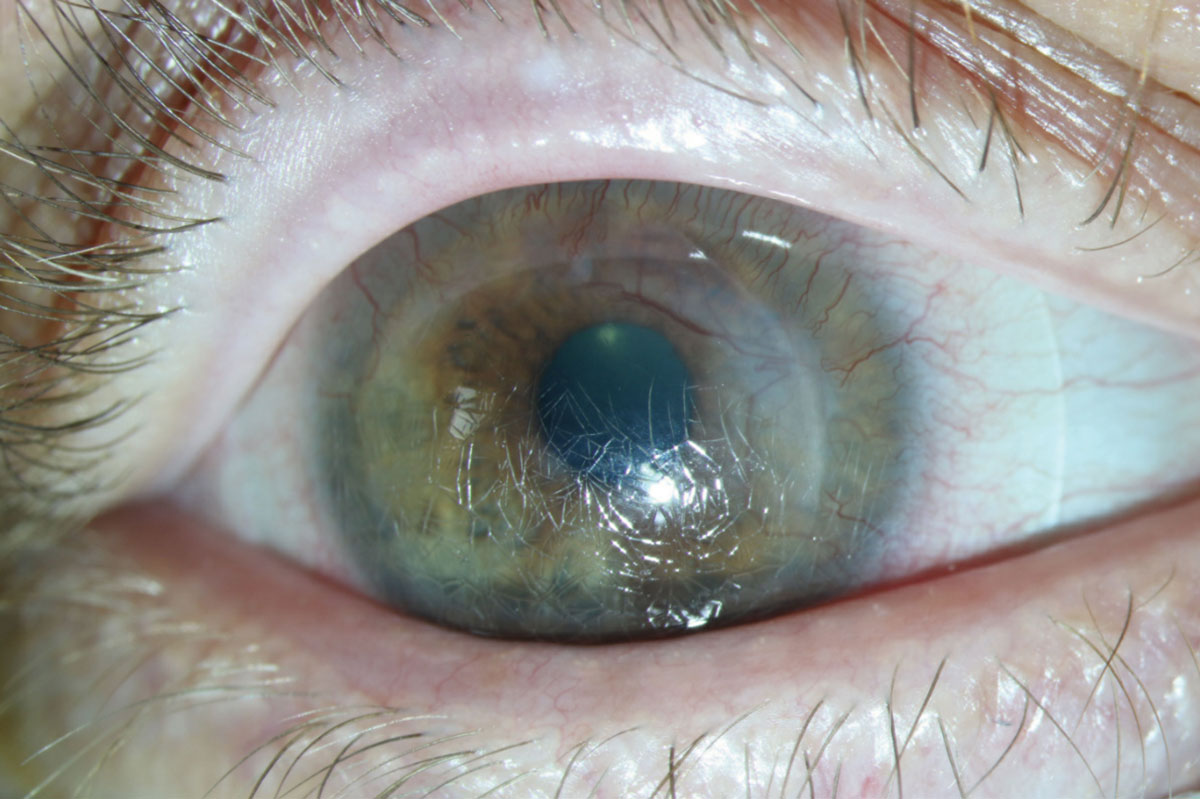 |
| Fig. 4. Over time, a scleral lens might get severely scratched and damaged. Photo: Gloria B Chiu, OD. Click image to enlarge. |
If lens deposits are a problem, the clinician should also investigate their origin, and if they are found to be due to foreign matter, such as makeup or improper cleaning, the patient should be reeducated to ensure proper lens handling.12 Handwashing may also help avoid the introduction of unwanted deposits.
After a scleral lens has been fit and finalized, keep in mind the lens will likely accumulate damage over time, such as scratches or warpage, which may result in a slight fit or vision change (Figure 4). In these instances, it may be best to replicate the last lens before attempting to make lens adjustments, especially if the lenses are more than a year old.
3. Keep Midday Fogging at Bay
It’s estimated that up to one-third of scleral lens patients experience midday fogging (Figures 5 and 6).13 This phenomenon results from either a lens that is fit too loosely or too tightly in the periphery, which may cause poor peripheral alignment with the sclera/episclera.14,15
A loose lens may subsequently result in too much tear exchange, which may trap debris or biomolecules between the cornea and lens. This may lead to a buildup of material within the tear reservoir and cause the lens to fog.
A tight peripheral lens may also trap debris or biomolecules between the cornea and lens, preventing the material from washing off the ocular surface. While the exact nature of these biomolecules is still not fully understood, some evidence suggests this material may be comprised of proteins or lipids.13
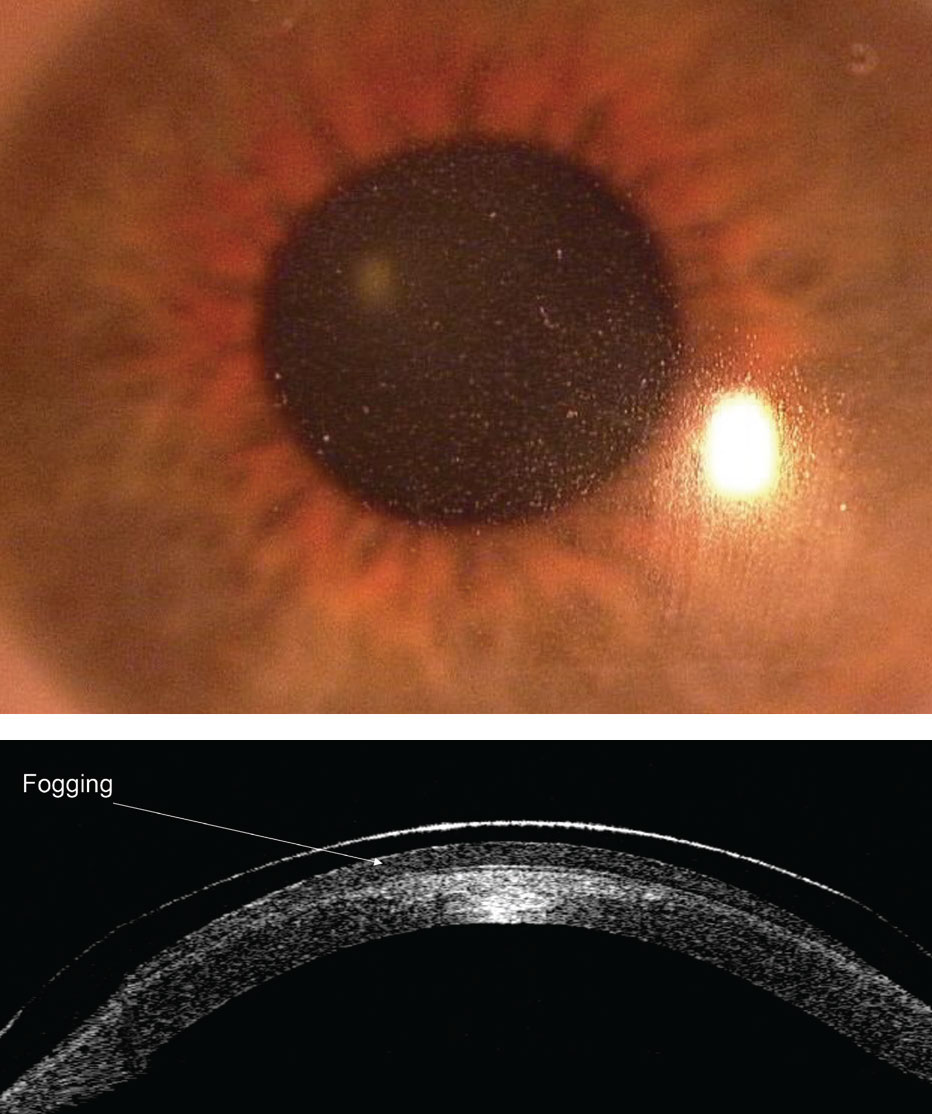 |
| Figs. 5 and 6. Midday fogging results from either a lens that is fit too loosely or too tightly in the periphery. Photos: Maria Walker, OD. Click image to enlarge. |
Alternatively, a scleral lens may induce a mild hypoxia situation that results in mild corneal swelling.16,17 Although modern materials are highly gas permeable, hypoxia may occur because tears are an oxygen barrier.16,17 Therefore, the greater the clearance between the cornea and the lens (thicker tear reservoir), the less oxygen will reach the cornea. This situation may subsequently result in a mild hypoxic situation that could cause white blood cells to infiltrate into the tear reservoir, which may also be a source of fogging.18 One study found that for every 50µm increase in tear reservoir thickness, there was a 1.72x increase in scleral lens fogging.18
With these issues in mind, especially when dealing with compromised corneas (e.g., post-surgical, Fuch’s endothelial dystrophy), practitioners should try to fit the lens as close to the cornea as possible while still avoiding corneal touch (~200µm after settling). Clinicians should also consider a quadrant-specific or fully customizable scleral lens periphery to allow for the best fit and to avoid seal-off or excessive tear exchange.10,19
In addition to these options, the SLAPP study group reported the top treatment for scleral lens fogging was to simply have patients remove, clean and reapply their lenses.10
By using these options, patients could avoid other complications commonly associated with cornea hypoxia, such as corneal neovascularization (growth of blood vessels from the limbal region into the cornea) and corneal edema (Figures 7 and 8).
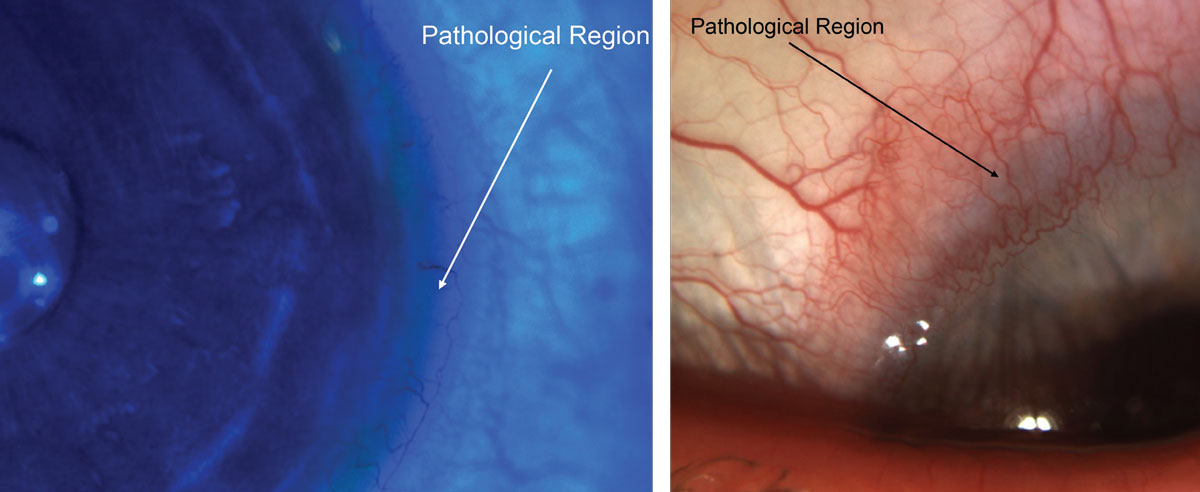 |
| Figs. 7 and 8. If neovascularization and corneal edema secondary to limbal touch, as seen here, occurs, a lens change would be needed. Photos: Maria Walker, OD. Click image to enlarge. |
4. Poorly Fit Lenses Lead to Ocular Trouble
Other issues that may stem from a poorly fit scleral lens include conjunctival prolapse, conjunctival redness and ocular discomfort.
Conjunctival prolapse is a condition wherein a small or large region of the conjunctiva is pulled within the lens chamber.13 While the Scleral Lenses in Current Ophthalmic Practice Evaluation (SCOPE) study group found that some contact lens practitioners were comfortable with less than 30º of conjunctival prolapse, few practitioners in the investigation said they were comfortable with more than 30 degrees of prolapse.20
If conjunctival prolapse occurs, it may likely deprive the limbus of oxygen, which could result in limbal stem cell death and, subsequently, a decreased ability to regenerate the cornea.
While one may think that enlarging the scleral lens chamber would resolve this issue, larger chambers may actually make the condition worse due to greater suctions.13 When you encounter conjunctival prolapse, make the lens chamber smaller. Quadrant-specific lens changes may likewise alleviate prolapse. Also, while a small amount of conjunctival prolapse is acceptable to some practitioners, try to at least mitigate prolapse for the listed reasons.20
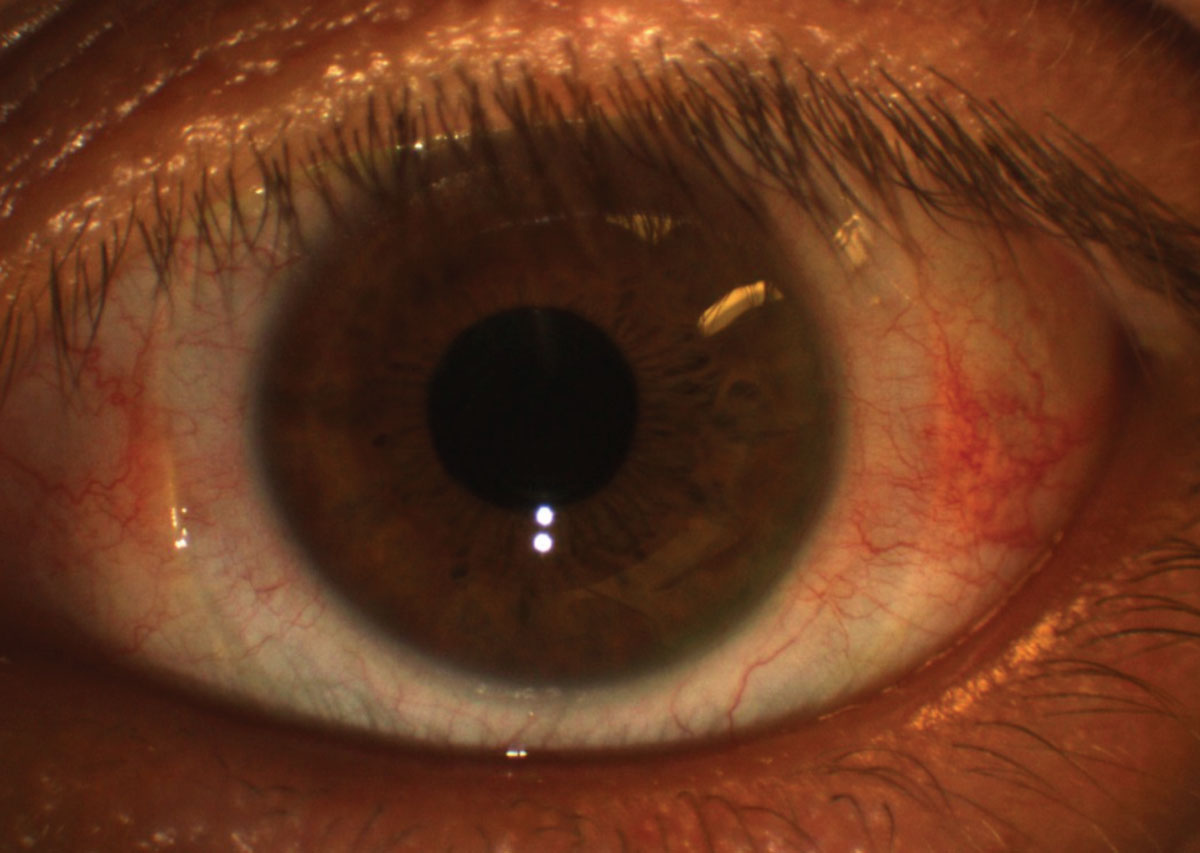 |
| Fig. 9. Conjunctival redness (3 o’clock and 9 o’clock regions) after scleral lens removal might be due to a lens that is too tight in the periphery. Photo: Maria Walker, OD. Click image to enlarge. |
Conjunctival redness is a primary sign of ocular inflammation, and when noted in an otherwise normal scleral lens wearer, it suggests the lens periphery may be too tight in the red region (Figure 9).21-26 This redness may occur near the limbus, which suggests that the lens periphery may be too flat, or near the lens edge, which suggests that the lens periphery may be too steep. This scenario can be likened to the toe (peripheral edge) and heel (limbal region) of a shoe.
This issue may first present as conjunctival blanching (blood vessel seal-off from the lens being too tight). The SLAPP study group found that optimizing the peripheral lens edge was the best treatment for ocular redness.10 Ocular discomfort is often a frequent complaint when poor peripheral edge fit occurs.
An alternative form of ocular redness, giant papillary conjunctivitis (GPC), has been reported to occur in 0.16% of scleral lens patients.8 While GPC is uncommon in scleral lens wearers, ODs should treat it similarly to an occurrence in a soft contact lens wearer, and should also address any underlying allergy issues.27 An effort should be made to remove potential allergens by cleaning the lenses with a product such as an enzymatic protein remover. GPC may also stem from mechanical issues, though this may be less of an issue with scleral lenses due to limited lens movement.
Other, more serious complications associated with scleral lens use are corneal infiltrates and microbial keratitis.8
A corneal infiltrate is the accumulation of white blood cells within the cornea. They may or may not be related to an ocular infection.28
Microbial keratitis happens when the cornea is infected with a microbe, such as bacteria, fungus or protozoa (e.g., Acanthamoeba), and it is by far the most serious complication since it can result in permanent vision loss or even the need for a corneal transplant once the condition has resolved.28 Since many scleral lens wearers already have compromised corneas, they may be at a higher risk of developing these two conditions.
While the frequency of corneal infiltrates and microbial keratitis has been estimated to be 0.17% and 0.08%, respectively, well-controlled prospective studies are still needed to fully understand the frequency of these complications.8 If corneal infection or inflammation does arise, suspect poor lens compliance.29 If a corneal complication does occur, lens wear should be ceased until the condition is under control, and these patients should be treated with antibiotic or antibiotic/steroid topical drops.
When they are able to return to lens wear, these patients should be re-educated about how to properly wear their scleral lenses to help avoid any potential reoccurrences. Remind patients that all their care products, including application devices and cases, are potential sources of contamination, and, because of this, these products should be regularly cleaned and replaced.30,31 One way to help ensure this is to provide your patients with a care bag that includes a set of application/removal devices since some patients have trouble finding replacement products.
Scleral lenses have become a mainstay for most practices. These specialty lenses are quickly becoming the standard of care for patients with complex refractive errors and for others who need long-term bandage contact lenses for extreme drying conditions, such as Sjögren’s or Stevens-Johnson syndromes.1 While the literature suggests scleral lenses are safe, especially when patients are correctly caring for them, a number of issues can still arise, so practitioners should regularly monitor their patients to help ensure they are successful and healthy wearers.
Dr. Pucker is an assistant professor at the University of Alabama at Birmingham.
1. Nau CB, Harthan J, Shorter E, et al. Demographic characteristics and prescribing patterns of scleral lens fitters: The SCOPE Study. Eye Contact Lens. 2018;44 Suppl 1:S265-72. 2. van der Worp E, Barnett M, Johns L. Scleral lenses: history & future. Cont Lens Anterior Eye 2018;41:243-4. 3. Macedo-de-Araujo RJ, van der Worp E, Gonzalez-Meijome JM. A one-year prospective study on scleral lens wear success. Cont Lens Anterior Eye. 2020;40. 4. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017;40:15-24. 5. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-82. 6. Pucker AD, Tichenor AA. A review of contact lens dropout. Clin Optom. 2020;12:85-94. 7. Bickle KM, Jones-Jordan LA, Kuhn J, et al. Initial scleral contact lens wearing experience. Poster presented at Global Specialty Lens Symposium 2019. 8. Schornack M, Harthan J, Barr JT, et al. Complications of scleral lens wear. ARVO 2016. Abstract A0147. 9. Food and Drug Administration. Hydrogen Peroxide Solution. www.fda.gov/medical-devices/contact-lenses/hydrogen-peroxide-solution. 2018. Accessed August 30, 2020. 10. Pucker AD, Bickle KM, Jones-Jordan LA, et al. Assessment of a practitioner’s perception of scleral contact lens complications. Cont Lens Anterior Eye. 2019;42:15-9. 11. Tangible Hydra-PEG. Tangible Science. tangiblescience.com/tangible-hydra-peg-toolkit. 2018. Accessed August 30, 2020. 12. Pucker AD, Nichols JJ. Impact of a rinse step on protein removal from silicone hydrogel contact lenses. Optom Vis Sci. 2009;86(8):943-7. 13. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens Anterior Eye. 2016;39:88-96. 14. McKinney A, Miller WL, Leach N, et al. The cause of midday visual fogging in scleral gas permeable lens wearers. Invest Ophthalmol Vis Sci. 2013;54:5483. 15. Skidmore KV, Walker MK, Marsack JD, et al. A measure of tear inflow in habitual scleral lens wearers with and without midday fogging. Cont Lens Anterior Eye. 2019;42:36-42. 16. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;35:266-71. 17. Kim YH, Tan B, Lin MC, Radke CJ. Central corneal edema with scleral lens wear. Curr Eye Res. 2018;43:1305-15. 18. Postnikoff CK, Pucker AD, Laurent J, et al. Identification of leukocytes associated with midday fogging in the post-lens tear film of scleral contact lens wearers. Invest Ophthalmol Vis Sci. 2019;60:226-33. 19. Consejo A, Llorens-Quintana C, Bartuzel MM, et al. Rotation asymmetry of the human sclera. Acta Ophthalmol. 2019;97:e266-70. 20. Harthan J, Shorter E, Nau C, et al. Scleral lens fitting and assessment strategies. Cont Lens Anterior Eye. 2019;42:9-14. 21. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539-74. 22. Wu S, Hong J, Tian L, et al. Assessment of bulbar redness with a newly developed keratograph. Optom Vis Sci. 2015;92:892-9. 23. Papas EB. Key factors in the subjective and objective assessment of conjunctival erythema. Invest Ophthalmol Vis Sci. 2000;41:687-91. 24. Fieguth P, Simpson T. Automated measurement of bulbar redness. Invest Ophthalmol Vis Sci. 2002;43:340-7. 25. Amparo F, Wang H, Emami-Naeini P, et al. The ocular redness index: a novel automated method for measuring ocular injection. Invest Ophthalmol Vis Sci. 2013;54:4821-6. 26. Peterson RC, Wolffsohn JS. Sensitivity and reliability of objective image analysis compared to subjective grading of bulbar hyperaemia. Br J Ophthalmol. 2007;91:1464-6. 27. Donshik PC, Ehlers WH, Ballow M. Giant papillary conjunctivitis. Immunol Allergy Clin North Am. 2008;28:83-103. 28. Ehlers JP, Shah CP. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. 29. Zimmerman AB, Marks A. Microbial keratitis secondary to unintended poor compliance with scleral gas-permeable contact lenses. Eye Contact Lens. 2014;40:e1-4. 30. Logan AK, Perrigin J. Microbial growth after cleaning scleral DMV devices. Poster presented at Global Specialty Lens Symposium 2017. 31. Wu Y, Carnt N, Willcox M, Stapleton F. Contact lens and lens storage case cleaning instructions: whose advice should we follow? Eye Contact Lens. 2010;36:68-72. |


