Corneal infections continue to trouble patients of all ages and lifestyles worldwide. Infectious keratitis occurs in 20 to 50 people per 100,000 in the United States, and the risk increases following any compromise to the corneal epithelium.1 These infections resist conventional therapies and can be difficult to differentiate clinically, adding to the challenges posed by this already sight-threatening group of pathologies. If you were to create an ideal treatment for corneal ulcers, you’d probably want something like this:
- The treatment should be safe to the patient’s own tissue.
- Its efficacy should cover a broad spectrum of pathogens, eliminating the need to differentiate clinically or with cultures prior to treating.
- The treatment’s dosage should allow patients to have a relatively normal schedule compared with hourly, or more frequent, administration of topical antimicrobials.
- Cost should be affordable to allow use as needed, without worry of reimbursement or patient finances.
On paper, corneal collagen crosslinking (CXL) for microbial keratitis, a treatment known as photo-activated chromophore for infectious keratitis (PACK-CXL), checks all of these boxes. In application, PACK-CXL, vaguely recognized by optometry as a treatment option for infectious keratitis, has several limitations that stymie its widespread use.
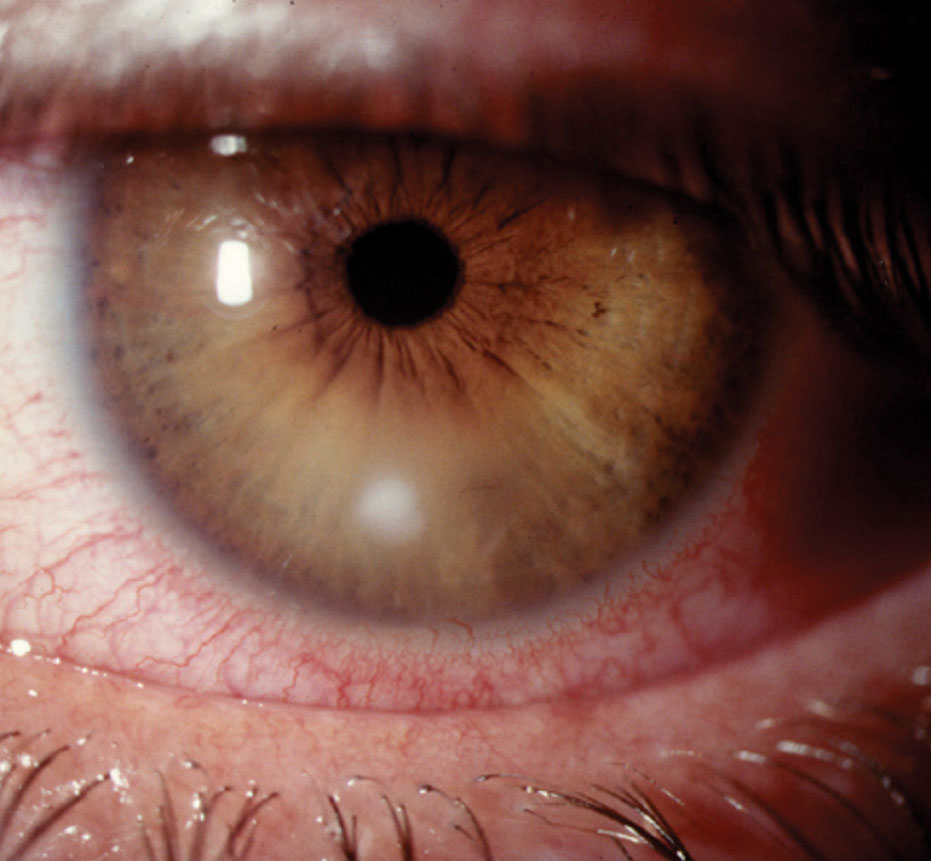 |
| PACK-CXL may be more successful for early corneal ulcers such as this, rather than more severe presentations. Photo: Joseph W. Sowka, OD, and Alan G. Kabat, OD |
The Hype
PACK-CXL follows the same general protocol as crosslinking for keratoconus. The cornea is saturated with riboflavin, a UVA source of 365µm is applied to the cornea for a period of time and then the patient recovers at home. More so than with traditional crosslinking, the exact protocol for PACK-CXL varies from center to center and relies on surgeon preferences, fluences of the UV lamp and the exact topical riboflavin concentration. Case-dependent features such as ulcer depth and degree of thinning also play a part.
Regardless of the precise protocol, the mixture of UV radiation, riboflavin and oxygen creates reactive oxygen species (ROS). In conventional crosslinking, these ROS lead to the activation of the lysyl oxidase pathway and the development of “crosslinks.” This activation also takes place with PACK-CXL, and the result is a stiffer cornea.2-4 This bolsters it against proteolytic melts common with infectious keratitis.
The “photo-activated riboflavin” in PACK-CXL disrupts base pairing of both pathogenic RNA and DNA, thereby inhibiting replication. In addition, oxidative destruction of the pathogen occurs via the ROS.2-4 PACK-CXL therefore theoretically kills the pathogen, blocks its replication and makes the cornea more resistant to further tissue destruction.
In addition, effectiveness of PACK-CXL should be independent of the specific pathogen, as all ulcers are going to benefit from increased tectonics, and all free-living pathogens (i.e., non-viral), in theory, would be susceptible to the massive quantities of ROS. One meta-analysis of the available literature shows good susceptibility to the ROS across bacterial, fungal and protozoan sources of corneal infection. In this analysis, 85.7% of bacterial keratitis cases, 91.7% of Acanthamoeba cases and 78.1% of fungal cases healed.3 Both cases of herpes simplex virus (HSV) keratitis in this review went on to melt and required a therapeutic keratoplasty, so PACK-CXL is probably best avoided in HSV cases.3
Ignoring the terrible outcomes reported with HSV, this review indicates that PACK-CXL actually has a broad spectrum of activity that isn’t affected by the pathogenic group (fungal, Acanthamoeba or bacterial) or its antimicrobial resistance profile, meaning, it should work on methicillin-resistant Staphylococcus aureus (MRSA) just as effectively as on Methicillin-susceptible Staphylococcus aureus (MSSA). These attributes and strengths could present a significant benefit to the clinician who, in theory, would no longer be required to accurately differentiate based on clinical features or culture results. As an effective one-size-fits-all treatment, PACK-CXL could possibly take the guesswork out of selecting the initial management.
If PACK-CXL were effective as a standalone treatment, patients could avoid the need to adhere to the challenging drop regimen characteristic of microbial treatment. Regimens that require some level of continuous therapy are standard in the early management of microbial keratitis and can stretch on for several weeks. In all cases, those treatments create a significant burden to the patient regarding both quality of life and compliance. If a single in-office treatment with PACK-CXL could eliminate or at least reduce the frequency of topical antimicrobial use, it would present a tangible benefit to the patient management.
The potential to reduce or eliminate an extensive eye drop regimen is the theoretic impact on cost. Treatments often take several weeks, and occasionally months, with frequent follow-up. In addition to cost of clinic care, the expense of conventional antimicrobial treatment can be high and, in certain parts of the world, cost prohibitive. For PACK-CXL, on the other hand, riboflavin is inexpensive and UV lamps are widely available. For most of the world, PACK-CXL as a standalone therapy would represent a significant improvement in average cost of therapy compared with conventional treatment. In fact, Farhad Hafezi, MD, past chair of Ophthalmology at University of Geneva and a primary proponent of PACK-CXL, has pointed out that the benefit of CXL as a treatment for infectious keratitis to impoverished parts of the world is potentially greater than CXL’s global benefit in treating keratoconus.
 |
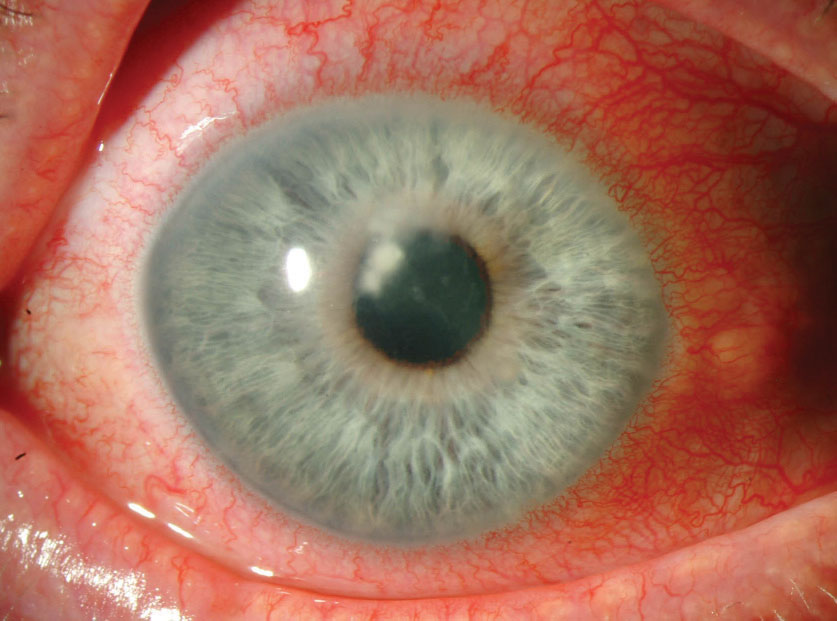
| While research suggests good efficacy for AK, seen here, animal studies are less promising. Photo: Christine W. Sindt, OD |
The Reality
On a cursory review and ignoring the details, PACK-CXL seems like an amazing treatment option that could address nearly all of the shortcomings and headaches associated with modern antimicrobial regimens for corneal infections. But as is often the case, the devil is in the details, and significant limitations exist with what exactly the research of PACK-CXL is suggesting in regards to efficacy, protocol and practical hurdles practitioners face—all of which may be barriers to its widespread use.
Protocol. There has been little formal standardization of the actual treatment protocol of the PACK-CXL procedure. “Dresden protocol” CXL (UVA fluence of 3mW/mm2 for 30 minutes) has been the most common published approach, but others have advocated for accelerated treatments with greater fluences, as well as longer treatments with standard fluences but a lower concentration of riboflavin.3 The postoperative course for PACK-CXL has also yet to be defined as well. Clinicians often use corticosteroids in the early postoperative period with conventional CXL to control inflammation, but given their potentially confounding effects on microbial keratitis, corticosteroids aren’t used in studies on PACK-CXL, which may have led to unnecessary, untreated exacerbations of sterile inflammatory problems. In fact, one large study found a transient increase in the size of hypopyon following PACK-CXL in some patients, likely indicating not a worsening of infectious inflammation but a sterile inflammation.2
Efficacy. While most research of PACK-CXL has been positive for the most part, there are some important holes in the research. Probably most important for understanding reports of the procedure’s efficacy is that the majority of available research has not directly compared PACK-CXL with conventional topical antimicrobial treatment. Instead, the bulk of the research compares the combination of PACK-CXL plus antimicrobials with topical antimicrobials alone. In one large meta-analysis, only 16 of the 175 eyes received PACK-CXL alone; all others continued with combined typical antimicrobials and PACK-CXL.3 With this in mind, the most we can say about these eyes is the addition of PACK-CXL to conventional therapy did not worsen outcomes compared with conventional therapy alone. This is starkly different than suggesting that PACK-CXL alone is equivalent to conventional therapy. So if a center uses PACK-CXL, the patient should still expect to use topical antimicrobials (with all the associated cost and inconvenience), selection of appropriate antimicrobials is still important, and clinical- and culture-based differentiation of infectious etiologies is still necessary. Obviously, this reduces some of the appeal of PACK-CXL.
Further, the available research on PACK-CXL seems to suggest that the procedure works best with early superficial ulcers that are bacterial in nature and works poorly in severe ulcers, most particularly with those that are fungal in nature—not surprising given the expected depth of treatment with conventional CXL. One article makes a compelling argument about the expected efficacy of PACK-CXL being relative to the depth of the ulcer. Pointing to previously determined depth of irradiance studies, the authors remind clinicians that 50% of irradiance is absorbed in the anterior 100µm of the cornea, 25% in the second 100µm and the remaining 25% irradiates the remaining cornea at increasingly low levels, and it could be expected that dense ulcers may reduce the penetrance of UV energy even further.2 The authors note that the procedure could produce better results for early and anterior ulcers and worse results with increasing depth of involvement. This concept corresponds with results of other studies that suggest the procedure’s efficacy diminishes with increasingly severe ulcers.3,5
Compounding its greater efficacy with superficial ulcers is the fact that it seems to perform differently among pathogen groups. For bacterial sources, most agree that PACK-CXL produces a bacteriocidal and bacteriostatic effect.2-4 This concept supports the clinical outcomes seen with PACK-CXL for bacterial keratitis. For fungal keratitis, both lab and animal models appear split on UVA+riboflavin producing any antifungal effect, and it is worth noting that a study of eyes with deep fungal keratitis treated with PACK-CXL was halted due to an increasing rate of perforation in the treatment arm.6 In addition, we also know that fungal keratitis treated with PACK-CXL is less likely to resolve than bacterial keratitis.3
For Acanthamoeba keratitis (AK), the 10 out of 11 successfully treated eyes mentioned in the meta-analysis contradict animal studies of the disease. One rabbit study of AK marked worsening of keratitis after CXL with riboflavin and UVA compared with those that did not receive treatment.6 These discrepancies between clinical- and lab-based research should give pause to those widely embracing the procedure for these more uncommon forms of keratitis.
Practice hurdles. In the US, the only FDA-approved platform for crosslinking is the Avedro KXL System with Photrexa riboflavin drops. While PACK-CXL is an off-label application of the device, most US centers offering CXL use the Avedro system. Recently, the cost of Photrexa drops has increased significantly, a material cost to a center that is then passed on to the patient. Because of this, PACK-CXL, in the United States at least, is almost certainly not going to offer a cost savings compared with conventional antimicrobials. However, with the availability of lower-cost systems across the globe, PACK-CXL still may offer savings in other countries.
 |
| PACK-CXL is least effective for severe cases of fungal keratitis, seen here secondary to Fusarium. Photo: Christine W. Sindt, OD |
The Verdict
Based on the current research, PACK-CXL might fit in nicely to the therapeutic algorithm for microbial keratitis treatment in well-chosen cases (namely, superficial bacterial ulcers). Its efficacy and wide spectrum of activity against bacteria (regardless of antibiotic resistance) and lesser activity against fungus and AK makes it not a one-size-fits-all treatment, but perhaps the next best thing. That said, it is not currently advocated as a replacement of conventional therapy but as an adjunct treatment. Further, the exact place of PACK-CXL in the therapeutic paradigm is hard to pin down. The procedure seems to perform better with early ulcers, making it more of a first-line therapy. However, its cost, off-label and experimental status and poorly defined protocol all serve to undermine its use as a first-line treatment. As costs come down and the protocol becomes more defined, this may change. Currently, however, the dissemination of PACK-CXL in the United States will probably remain a secondary treatment option, likely to the detriment of its effectiveness.
Dr. Bronner is a staff optometrist at Pacific Cataract and Laser Institute in Kennewick, WA.
1. Pepose J, Wilhelmus K. Divergent approaches to the management of corneal ulcers. Am J Ophthalmol. 1992;114:630-2. 2. Said DG, Elalfy MS, Gatzioufas Z, et al. Collagen cross-linking with photoactivated riboflavin (PACK-CXL) for the treatment of advanced infectious keratitis with corneal melting. Ophthalmology. 2014;121:1377-82. 3. Papaioannou L. Corneal collagen cross-linking for infectious keratitis: a systemic review and meta analysis. Cornea. 2015;0:1-10. 4. Price MO, Price FW. Corneal cross-linking in the treatment of corneal ulcers. Curr Opin Ophthalmol. 2015;26:1-6. 5. Uddaraja M, Mascarenhas J, Das MR, et al. Corneal cross-linking as an adjuvant therapy in the management of recalcitrant deep stromal fungal keratitis: a randomized trial. Am J Ophthalmol. 2015;160:131-4. 7. Berra M, Galperín G, Boscaro G, et al. Treat6ent of Acanthamoeba keratitis by corneal cross-linking. Cornea. 2013;32:174-8. |


