 General consensus in GP lens fitting is that you shouldn’t prescribe toric GPs for eyes that are post-penetrating keratoplasty. I always assumed this was because the corneal toricity is often irregular in these conditions. However, as anyone who fits irregular corneas can tell you, each patient must be treated individually. From the flat central/steep mid-peripheral topography of some grafts to the decentered or tilted grafts we encounter, corneal transplants certainly have wide variations in shape and curve. Approaching each eye as a unique case and taking the time to consider the lens options available can help provide patients with an optimal outcome. Over the next two columns, I will compare two highly toric post-graft patients and discuss how they differed in corneal shape and outcome.
General consensus in GP lens fitting is that you shouldn’t prescribe toric GPs for eyes that are post-penetrating keratoplasty. I always assumed this was because the corneal toricity is often irregular in these conditions. However, as anyone who fits irregular corneas can tell you, each patient must be treated individually. From the flat central/steep mid-peripheral topography of some grafts to the decentered or tilted grafts we encounter, corneal transplants certainly have wide variations in shape and curve. Approaching each eye as a unique case and taking the time to consider the lens options available can help provide patients with an optimal outcome. Over the next two columns, I will compare two highly toric post-graft patients and discuss how they differed in corneal shape and outcome.
A Case Study
To start, let me introduce you to a 59-year-old female who presented for a right eye contact lens fitting. She had a history of penetrating keratoplasty several years prior for keratoconus, and had worn a corneal GP lens in her left eye for many years. She reported that her right eye had good near vision since her surgery and she enjoyed the monovision effect, but recently the near vision was getting increasingly blurry. She had previously seen a doctor who had recommended a scleral lens fitting. This patient came to my office in hopes of finding an alternative solution.
Her uncorrected vision in the right eye was 20/600. With a refraction of -2.50D—7.00D x 040, her vision improved to 20/40. Her corneal topography demonstrated high with-the-rule astigmatism that appeared to extend beyond the borders of the graft to the host cornea. The graft was otherwise clear. The left eye graft was also clear and was well fitted with a 10.0mm spherical intralimbal lens.
After discussing all of the options with her—including a wide variety of contact lenses (sclerals, hybrids, soft torics, corneal GPs, etc.), laser vision correction for the astigmatism, and limbal relaxing incisions (LRI)—she favored the idea of trying to fit the right eye in a corneal lens design similar to the left eye, as she had good comfort and vision with that lens. I agreed and we attempted a trial lens fitting using a spherical intralimbal lens design.
But, after a few attempts with the fitting set lenses, it became obvious that the astigmatism was regular enough—and extensive enough—that we were not going to get an optimal fit with a spherical lens. It appeared that a toric base curve design would be indicated (figure 1).
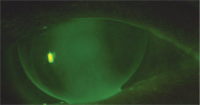
1. Post PK with spherical base curve lens.
A lens was ordered empirically, using the information that the attempted spherical lens fit provided. Her corneal topography measured 8.9D of astigmatism. The initial lens was ordered in a bitoric design with 5.75D of toricity and a diameter of 10.2mm (figure 2). This lens demonstrated an exceptionally aligned fluorescein pattern and good patient comfort and stability. With a slight over-refraction, the patient achieved 20/25+2 acuity in her right eye. The final lens was reordered with the same fit parameters, as well as an Rx to provide near vision as she wished to maintain her monovision set up. The patient continues to use this lens design two years later.
The point of this case report is to suggest that there are times when a toric base curve lens is the best choice for a post-penetrating keratoplasty cornea. How do you decide? The first indication would be finding a fluorescein pattern that looks like a truly regular astigmatic cornea during the trial lens fitting. Another indication that you might need a toric base curve is when the corneal astigmatism is highly regular and extends beyond the borders of the graft. The opposite is true as well—when the astigmatism is contained within the graft, a toric lens is usually not the best choice. We will talk more about this scenario in the April column.
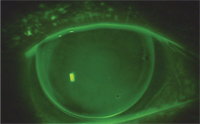
2. Post PK with bitoric base curve lens.


