  |
A 52-year-old black male was referred by his pulmonary transplant team for persistent redness that had plagued his left eye for nearly two months. The patient was asymptomatic for pain, discharge, itching and vision loss.
Ocular history was significant for remote trauma of the right eye nearly 10 years prior, which had resulted in globe rupture and subsequent enucleation. He presented for his annual exams initially but was lost to follow-up for five years. Medical history was significant for pulmonary fibrosis that led to a double lung transplant four years ago. He was taking chronic tacrolimus and low-dose prednisone.
On examination, the right lids and visible conjunctiva appeared normal, and the prosthetic was in a good position. The patient refused prosthesis removal to view the remainder of the conjunctiva and ensure no orbital implant exposure.
In the left eye, vision was 20/20 and intraocular pressure was 17mm Hg. Pupillary function and extraocular motilities were normal. The posterior segment was also unremarkable. On slit lamp exam, there were scattered, thickened leukoplakic lesions over the nasal and inferior bulbar conjunctiva with attendant moderate injection. Near the limbus, the lesions became more gelatinous in appearance and involved nearly six clock hours, from 6:00 to 12:00. There were flat, opalescent lesions peripherally with fimbriated extension onto the cornea, which stained positively with rose bengal.
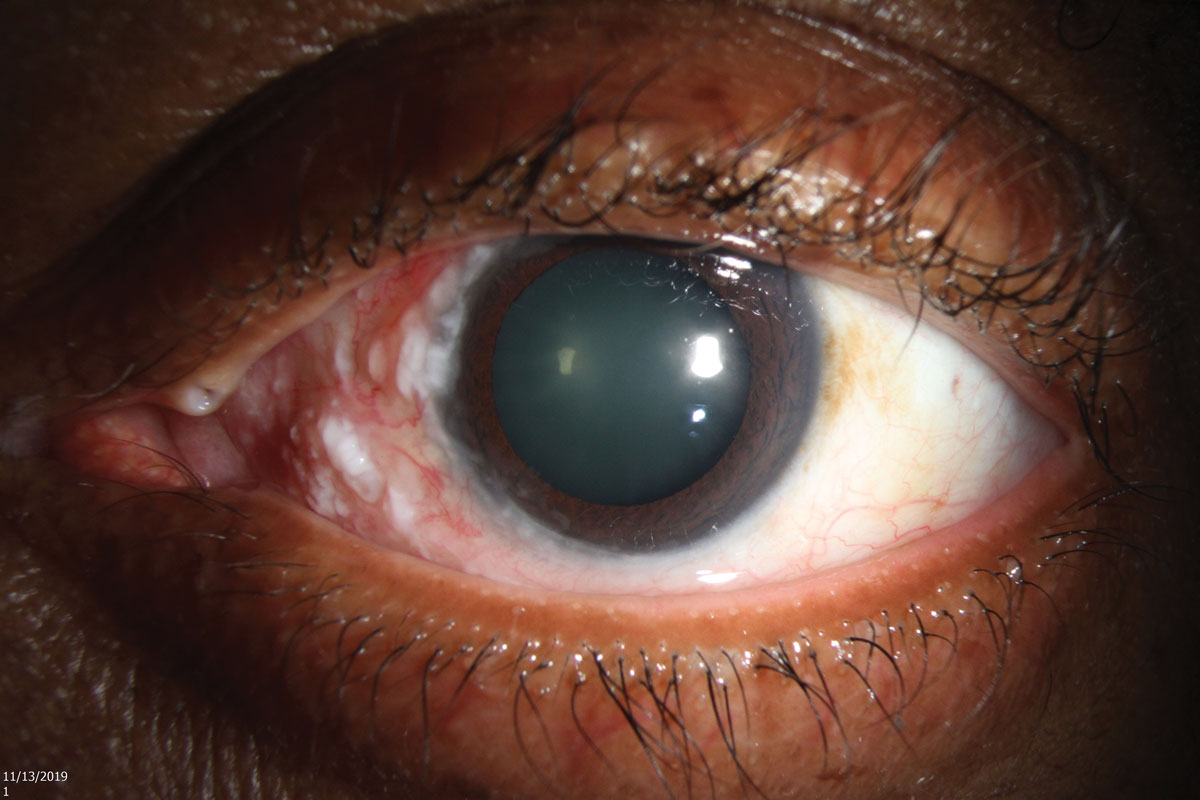 |
| Fig. 1. Slit lamp photo of the ocular surface lesion involving the nasal conjunctiva and limbus. Click image to enlarge. |
The concern for ocular surface squamous neoplasia (OSSN) prompted further questioning. The patient was immunosuppressed but also reported a history of significant UV exposure after living in southern Florida his entire life. He denied any history of skin cancer, human immunodeficiency virus or cutaneous human papillomavirus.1
Imaging helps determine lesion progression or therapeutic response in cases of suspected neoplasm. Slit lamp photography and ultra-high-res OCT (UHR-OCT) shed light on baseline findings, including a diffusely thickened and hyper-reflective epithelium with an abrupt transition zone consistent with OSSN (Figures 1, 2 and 3).
The patient was referred to an anterior segment surgeon who specializes in ocular surface tumors. He was prescribed 5-fluorouracil (5-FU) QID for one week and advised to then take three weeks off treatment. It was expected that he would need eight one-month cycles of treatment. Unfortunately, at his six-week follow up, he had not yet obtained the topical chemotherapeutic agent and his lesion had progressed (Figure 4).
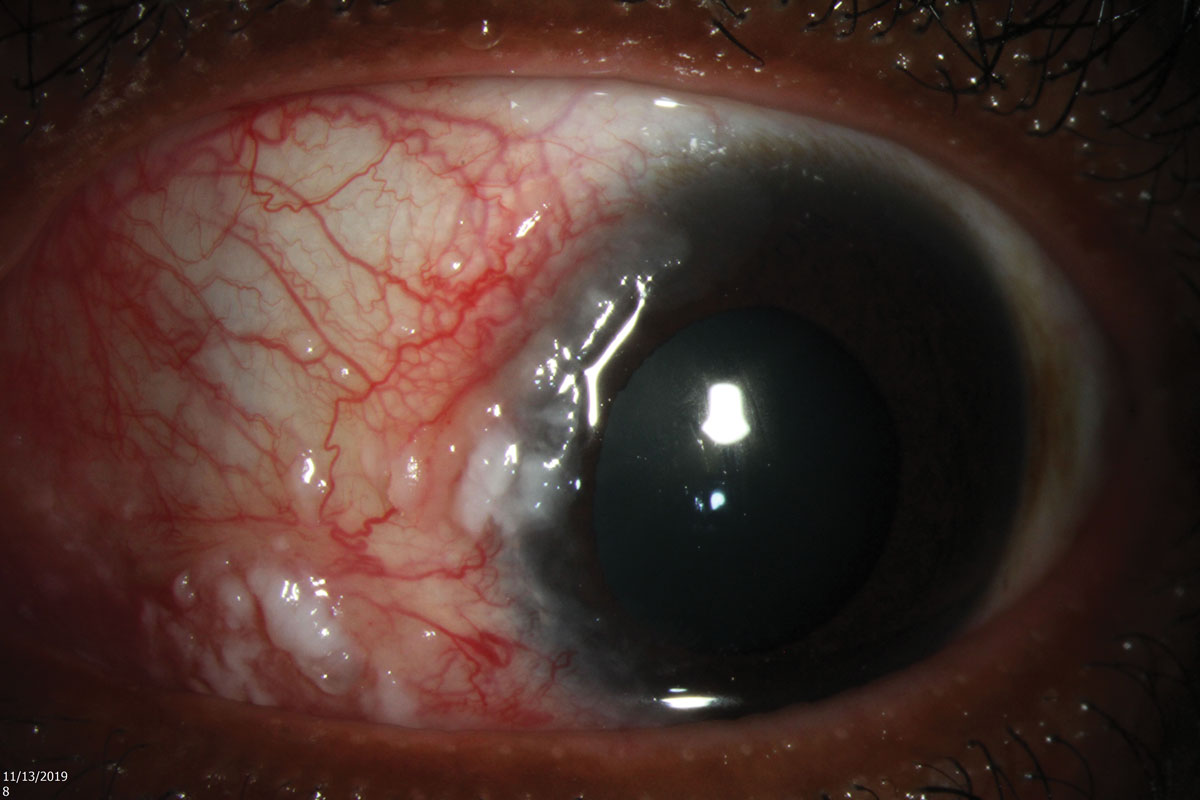 |
| Fig. 2. Gelatinous and leukoplakic features of the lesion, with attendant vascular engorgement. Click image to enlarge. |
Ocular Surface Lesions
Ocular surface lesions can vary widely in presentation and morphology. When evaluating any conjunctival or corneal lesion, our list of potential diagnoses should remain broad initially. Common lesions include pinguecula, pterygium, nevus, papilloma and pyogenic granuloma. When we begin to suspect neoplastic cells, we should become familiar with OSSN.
OSSN lesions are associated with a thickened epithelium near the limbus and may possess certain qualities, such as “feeder” vessels, local injection and overlying keratinization. Compared to conjunctival intraepithelial neoplasia (CIN), the term OSSN may be more favorable clinically due to our inability to assess the lesion’s depth and define it by its extension without an invasive biopsy. For example, if a neoplasia is contained within the epithelium and has not penetrated the basement membrane, it is termed CIN. Full-thickness epithelial involvement with significant cellular atypia on histopathology but an intact basement membrane is considered squamous carcinoma in situ. If the basement membrane is not intact and there is invasion of underlying tissue, it is considered invasive squamous cell carcinoma.
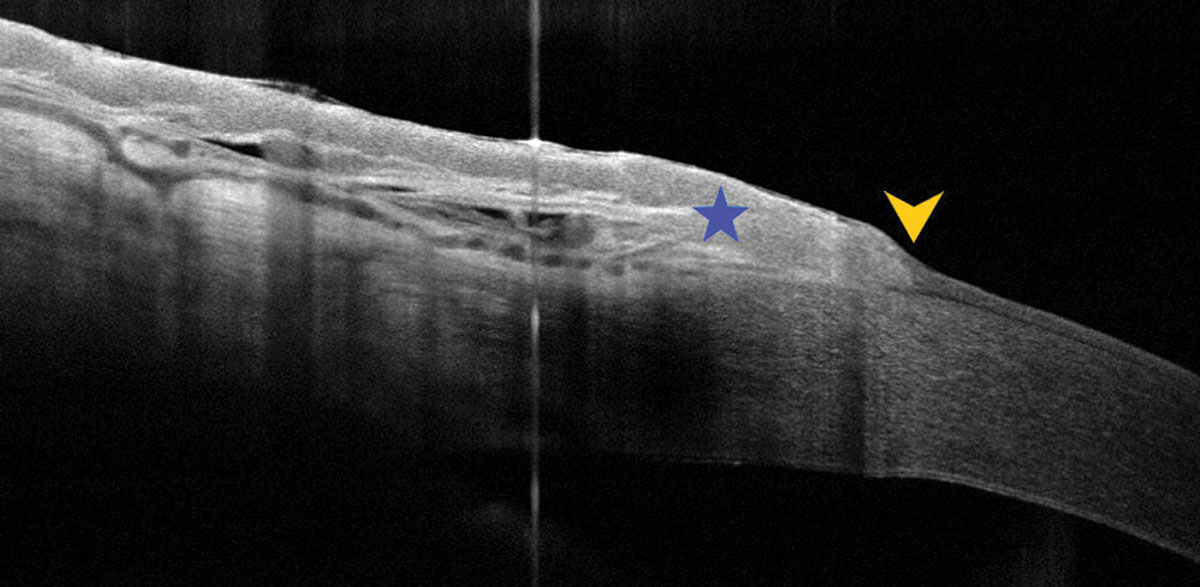 |
| Fig. 3. UHR-OCT captured the thickened, hyper-reflective epithelium (star) and the abrupt reflectivity change (arrow), both of which are consistent with OSSN. Click image to enlarge. |
Diagnosis
Differentiation of lesions may include the use of clinically available dyes, such as rose bengal, methylene blue and toluidine blue. Each dye will stain devitalized or degenerated epithelial cells, which are commonly seen in epithelial neoplasms. The dye uptake is not specific to neoplasms, however, and may be seen in some benign lesions or severe dry eye syndrome.2
In recent years, UHR-OCT has garnered attention as a noninvasive, in vivo imaging technique for ocular surface neoplasms. It is a specially designed anterior segment OCT instrument with a resolution of 3μm that can reveal abnormal characteristics. In cases of OSSN, UHR-OCT shows a thickened, highly hyper-reflective epithelium (>120μm) that abruptly transitions to a normal epithelium.3,4
Pterygia imaging demonstrates a normal to mildly thickened epithelium with moderate hyper-reflectivity and a hyper-reflective fibrillary layer under the conjunctival or corneal epithelium. An amelanotic melanoma is associated with a normal to slightly thick epithelium over a significantly hyper-reflective subepithelial lesion with posterior shadowing.5,6 Though UHR-OCT is not adapted for mainstream use, there are commercially available instruments with resolutions of 5μm to 7μm that may provide diagnostic data to help differentiate lesions.5
Surgical excision and histopathologic evaluation remain useful in the diagnosis of suspicious lesions. Biopsies carry inherent risks of bleeding, scarring, incomplete excision, recurrence, further seeding of neoplastic cells, limbal stem cell deficiency and inadequate sampling in cases of incisional biopsy. Excisional biopsy of a suspected neoplastic lesion uses a “no-touch” technique, in which conjunctival lesions are completely excised with 3mm to 4mm margins and cryotherapy is applied to the edges of excision.7 Absolute alcohol is often applied, and an amniotic membrane may also be used.
 |
| Fig. 4. Ten weeks later, the lesion had slightly progressed, as the patient had not obtained his medication. Click image to enlarge. |
Treatment
OSSN treatment has vastly changed over the last 15 to 20 years. While excisional biopsy is still used for ocular surface tumors, topical chemotherapy has increased in popularity due to its less invasive nature, reduced complication rate and ability to treat the entire surface, including areas of subclinical disease that could lead to recurrence. The three most commonly used topical agents are interferon alpha-2b (IFN), 5-FU and mitomycin C (MMC).5,8 Each is efficacious, but there are no randomized controlled trials to compare them directly.
MMC has the highest reported complication rates of epitheliopathy, redness, keratitis, limbal stem cell deficiency and punctal stenosis. Punctal plugs must be used with MMC. While 5-FU’s side effects are similar to MMC, they’re also less profound. IFN is often the treatment of choice due to its improved tolerability and low side effect profile but is often the most costly of the three medications.
In our patient, the clinical suspicion for OSSN was supported by UHR-OCT. This “optical biopsy” can aid in both initial diagnosis and continued management of ocular surface lesions. We hope that our patient responds positively to topical therapy and will follow him on a regular basis with repeat UHR-OCT imaging to monitor for improvement.
1. Carreira H, Coutinho F, Carrilho C, et al. HIV and HPV infections and ocular surface squamous neoplasia: systematic review and meta-analysis. Br J Cancer. 2013;109(7):1981-8. 2. Nanji AA, Mercado C, Galor A, et al. Updates in ocular surface tumor diagnostics. Int Ophthalmol Clin. 2017;57(3):47-62. 3. Sepulveda R, Pe’er J, Midena E, et al. Topical chemotherapy for ocular surface squamous neoplasia: current status. Br J Ophthalmol. 2010;94(5):532-5. 4. Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol. 2013;24(4):336-42. 5. Nanji AA, Sayyad FE, Galor A, et al. High-resolution optical coherence tomography as an adjunctive tool in the diagnosis of corneal and conjunctival pathology. Ocul Surf. 2015;13(3):226-35. 6. Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors: the 1994 Lynn B. McMahan lecture. Arch Ophthalmol. 1997;115(6):808-15. 7. Shousha MA, Karp CL, Canto AP, et al. Diagnosis of ocular surface lesions using ultra-high-resolution optical coherence tomography. Ophthalmology. 2013;120(5):883-91. 8. Kieval JZ, Karp CL, Abou Shousha M, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology. 2012;119(3):481-6. |


