For many eyecare providers, corneal topography is never given a thought. To be a contact lens fitter, I had to have a corneal topographer—a good one! My practice would not be complete without it. The first new piece of equipment I purchased was a mighty, small placido disc topographer. Technology has improved by leaps and bounds since those early days, as has the role that these devices can play.
Topography platforms today incorporate software that expands the technology’s capabilities to include design assistance for custom gas permeable (GP) lenses, myopia management platforms, higher-order aberration assessment, meibography, anterior segment cameras and dry eye suites.
Let’s discuss the types of images we collect, the most important measurements to consider as well as how to put the data to use in contact lens fitting.
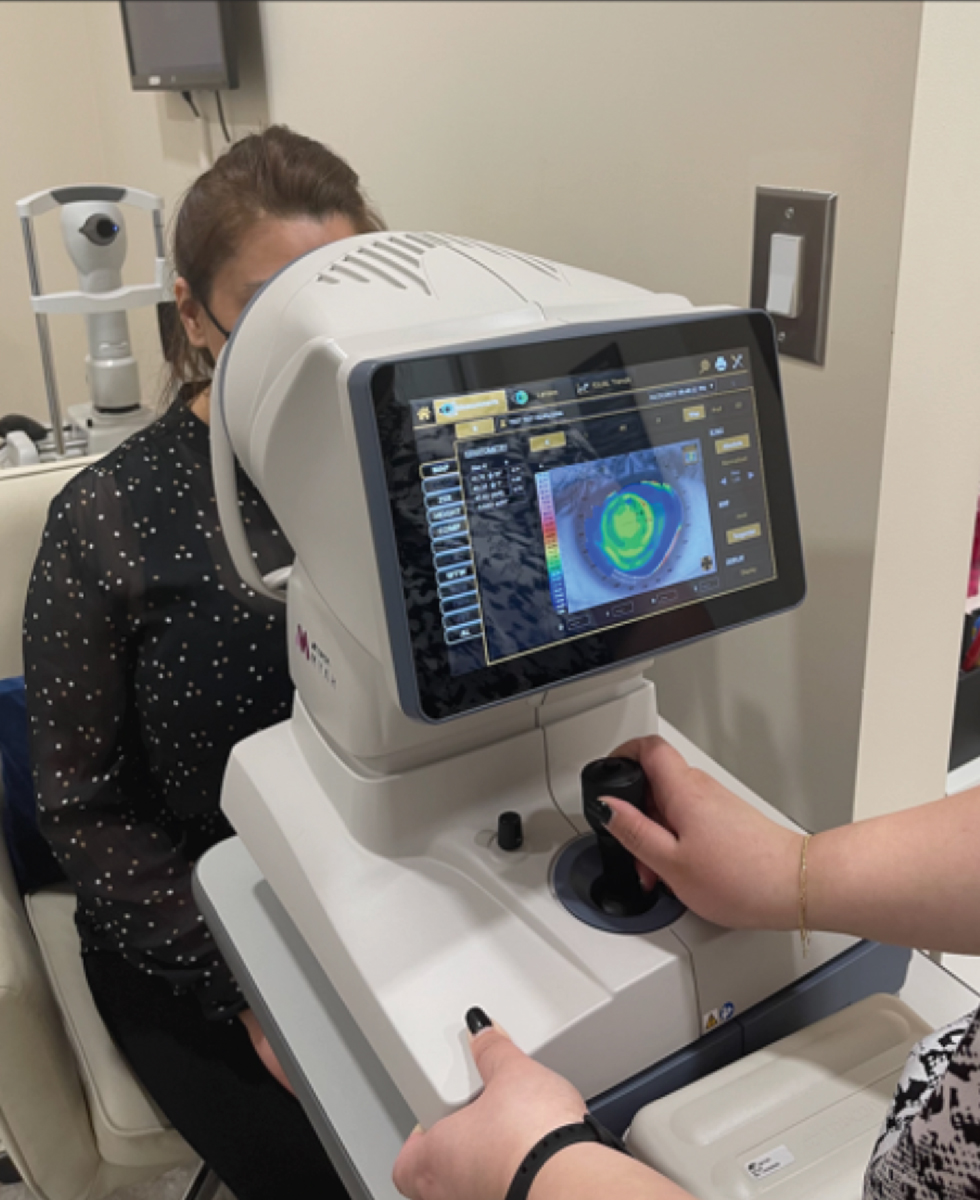 |
|
A Topcon Myah in use. The device combines axial length, dry eye testing, meibography and corneal topography in a single machine. Click image to enlarge. |
Reflection vs. Projection
There are two categories of topographer: placido disc (reflection)-based and elevation (projection)-based.
Reflection-based topographers project a series of rings on the cornea. The image of the reflected rings on the tear film is captured, the distance between the rings is measured and the slope is calculated, from which the height is extrapolated. This is the most widely and commonly used type of topographer. When rings are close together, it indicates that there is a high rate of change in curvature in that area.
Rings that are further apart have a slow rate of change. Small-cone systems collect more data points and are more accurate than large-cone placido disc systems. Both iterations depend on alignment during capture and a robust ocular surface to capture a complete ring set image. If the patient is off-axis or the cornea is dry, the data collected and extrapolated will be inaccurate.1,2
Examples of these topographers include the Medmont E300 and Meridia, the Oculus Keratograph and the Zeiss Atlas.
Elevation-based topographers evaluate specific points on the cornea and measure the height of the cornea at those points. Highly irregular corneas and distorted surfaces can be analyzed. These topographers image through the cornea, using off-axis light to provide details of both the front and the back surfaces of the cornea.
The analysis of the posterior cornea is a key difference between placido disc- and elevation-based topographers, as it allows for earlier detection of ectatic changes than was previously possible. This technology also allows for global pachymetry calculations, axial length, anterior vault and surgical measurements for LASIK and cataract extractions.3 Examples of elevation-based topographers are the Oculus Pentacam and the Bausch + Lomb Orbscan.
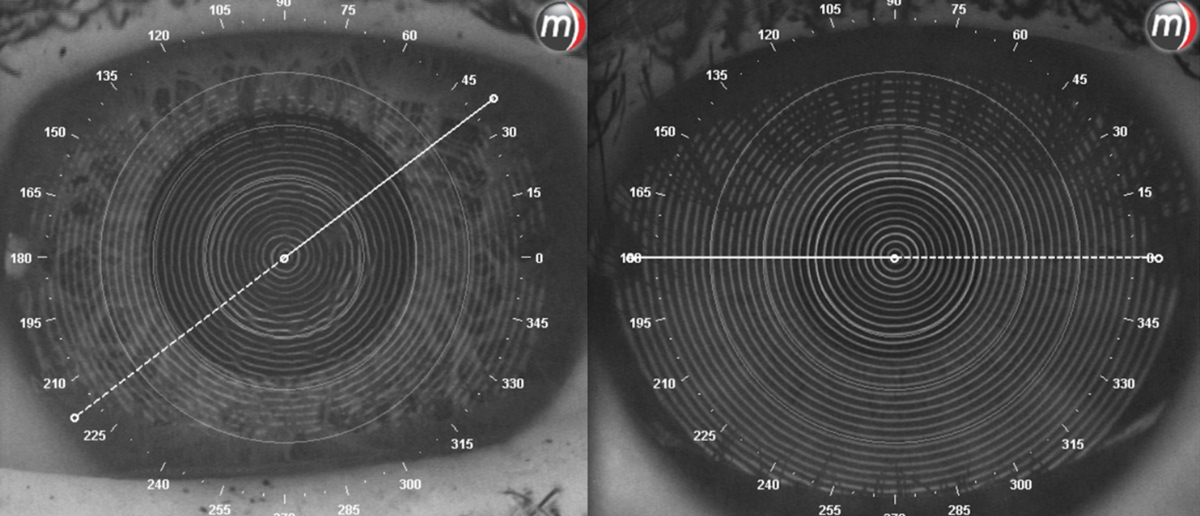 |
|
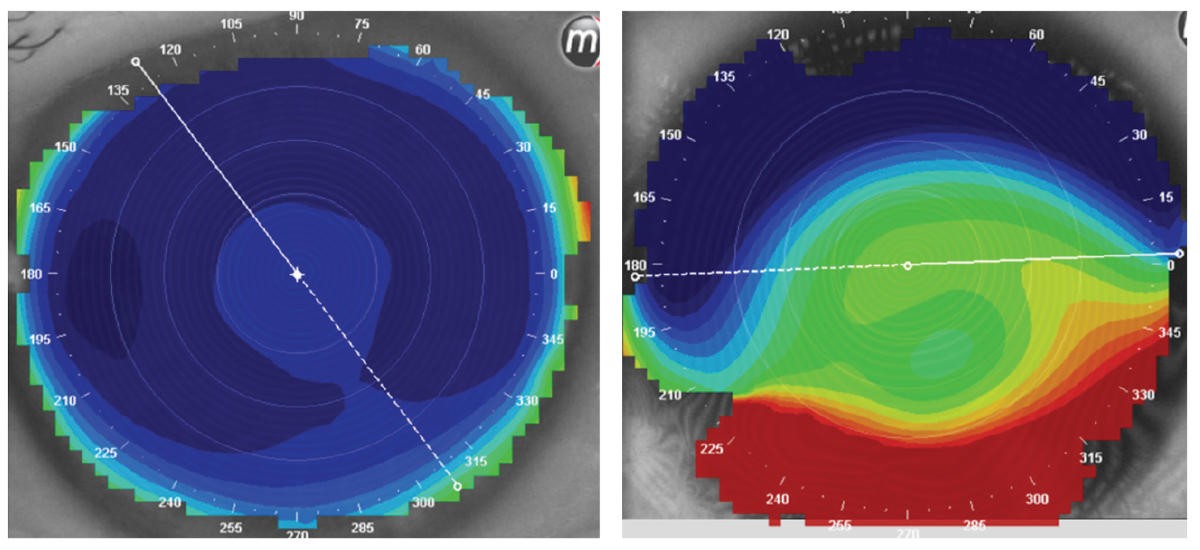
At left, a comparison of an eye with a poor ocular surface due to dry eyes. The mires are incomplete and distorted. At right, clean ocular surface with no dryness present. Click image to enlarge. |
Image Capture
The only way to get a great topographic map with accurate data is to take a good image. In order to do that, a patient must be comfortable, properly aligned within the instrument and looking in a direction that allows for proper alignment of the mires onto the cornea. A good ocular surface is helpful as well.1 The use of preservative-free saline on a dry eye will help clear up distorted mires, if present.
Topographic Maps
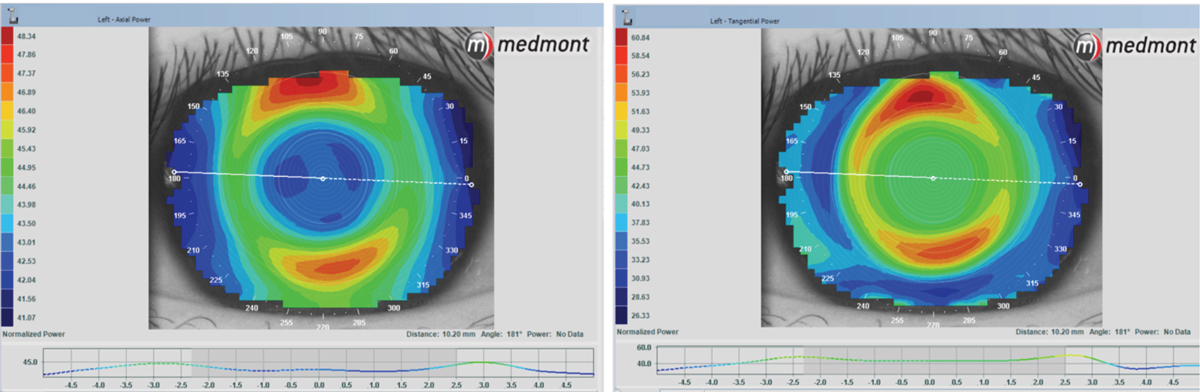
There are many ways to visualize the data collected from a topographer. A few of the most common and useful maps include the axial map, the elevation map and the tangential map.
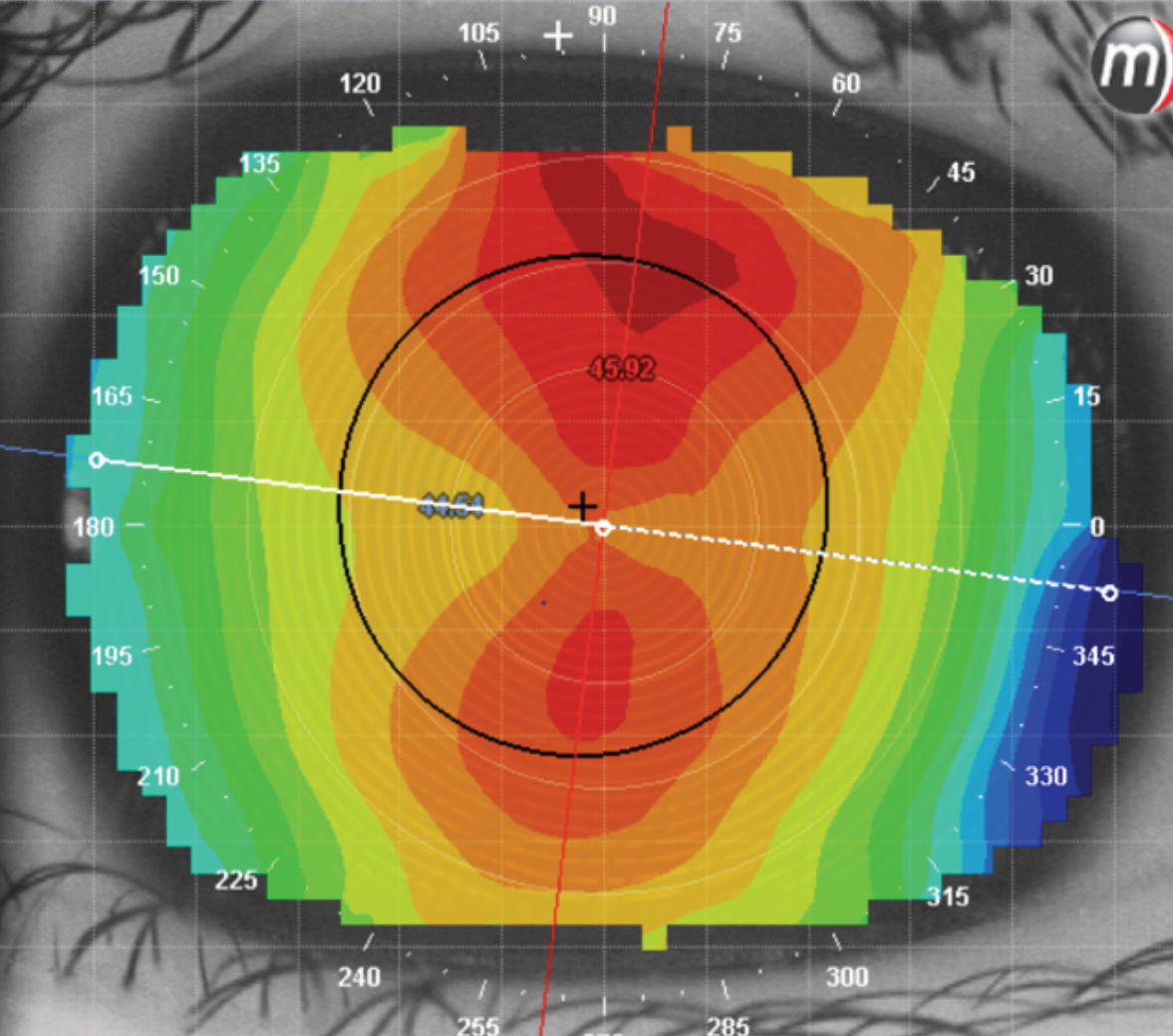
The axial map shows the corneal curvature in diopters; as such, think of it as a representation of how the refractive power is distributed across the corneal surface. The reference point for these maps is the central axis, from which changes in curvatures are measured.4 Red indicates a high rate of change in curvature, whereas blue denotes a slow rate of change in curvature. The center of this map—closest to the central axis— is more detailed and accurate than the edges of these maps. The data at the edges of the map are averaged and extrapolated to create a smooth image for us to view—the “airbrushed map,” if you will. The downside to this extrapolation is that it yields a map that misses important blips and blemishes, which can be critical for assessing true corneal shape.5
Despite this, axial maps continue to be the most used map by practitioners. My clinical experience has guided me to uses these maps to determine the base curve of soft and GP lenses using the most detailed central curvature data.
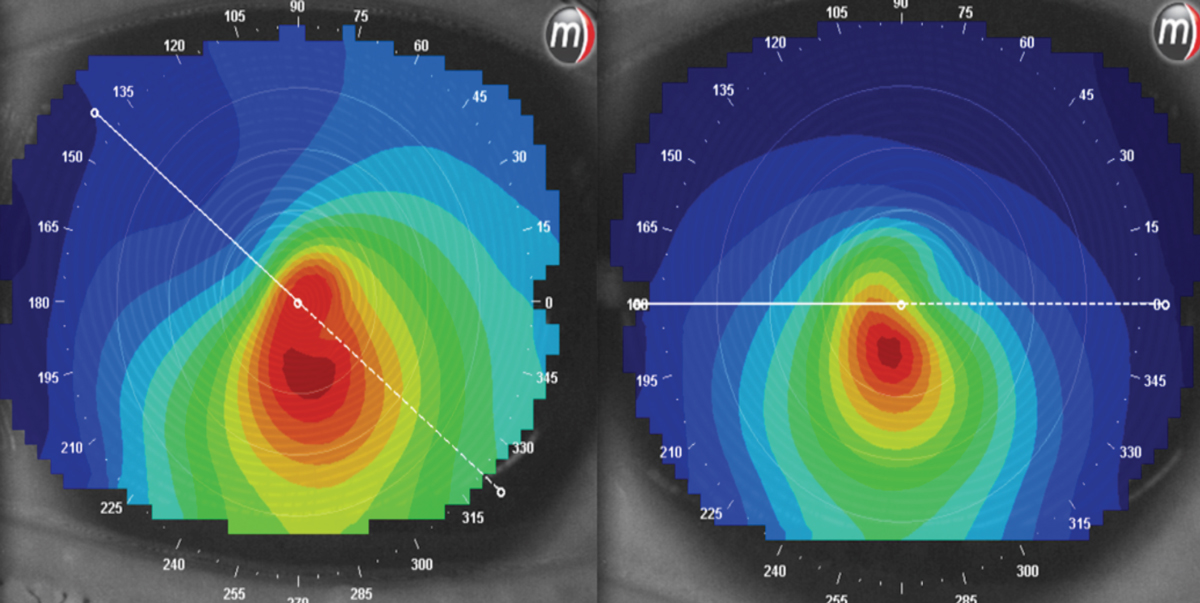 |
|
At left, a patient is looking off center when this image was taken. The right images were taken while looking straight ahead. The patterns are very different between the two. Click image to enlarge. |
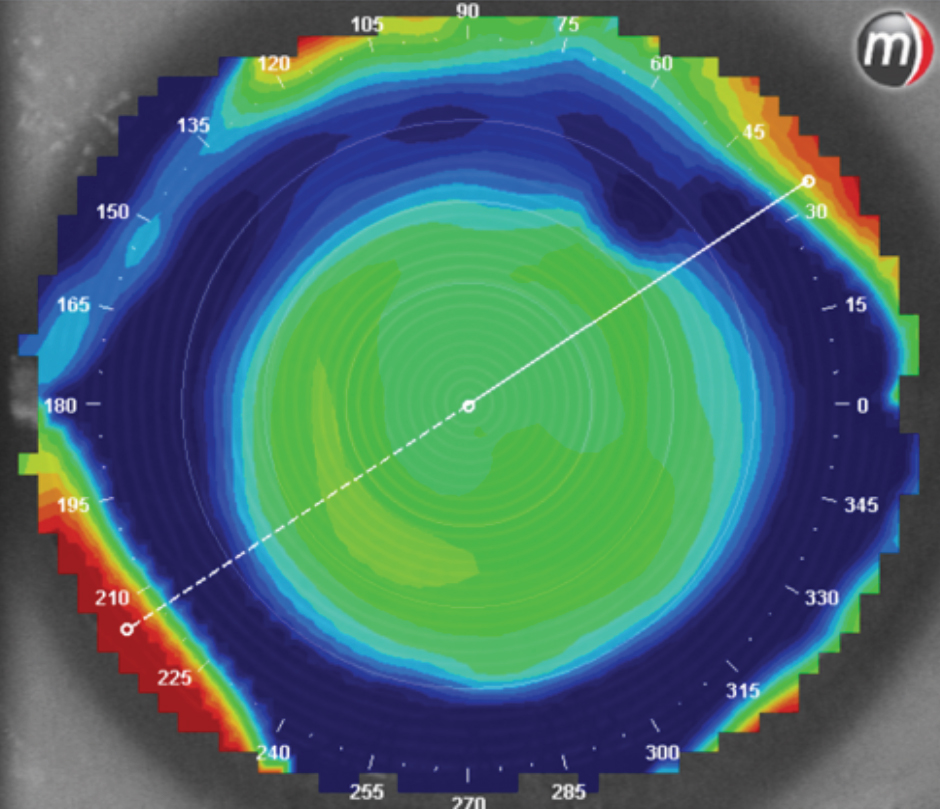
The elevation maps are created based on a reference surface that is placed on the eye, like a spherical GP would be placed on the eye. The heights are measured above and below the reference sphere; red above and blue below. These maps are best used for regular corneas to determine the starting spherical GP to place on the eye and for toric corneas to determine if a sphere, aspheric or toric lens is needed.6
Elevation should not be confused with the other two maps; this map gives a sense of how high or low the cornea is (often distinct from how steep or flat). As such, elevation maps can often be the most helpful in visualizing how a GP lens may actually fit on the eye (with higher areas likely to touch, lower areas likely to pool and everything else somewhere in between).
These maps are also helpful with irregular corneas to determine if a GP lens would work of if a scleral lens would be the better choice. As a rule of thumb: if the steepest elevation compared with the flattest elevation shows a difference of greater than 300µm, then a scleral lens is likely to be most successful. Placing a GP lens on such a cornea with a large elevation difference is comparable to trying to balance a teeter-totter. The fit will be poor and the patient uncomfortable and unhappy.
The tangential map, known as the true map, in contrast to the other two, does not rely on a reference point, central axis or reference curvature. There is no airbrushing of the data, and true corneal shape can be appreciated; red represents steep curvatures, while blue represents true flat curves. This is the most sensitive of maps and allows for the greatest accuracy of data at the periphery.4 As such, these maps are critical in understanding the true shape of the cornea, the true size of a cone, the location of a scar or pinguecula, the fitting of orthokeratology (ortho-K) lenses that require peripheral fitting evaluation, determining the apex of the cornea and monitoring corneal conditions and irregularities for change over time. This is a high-yield map and should be the go-to for getting an accurate understanding of corneal shape and monitoring.
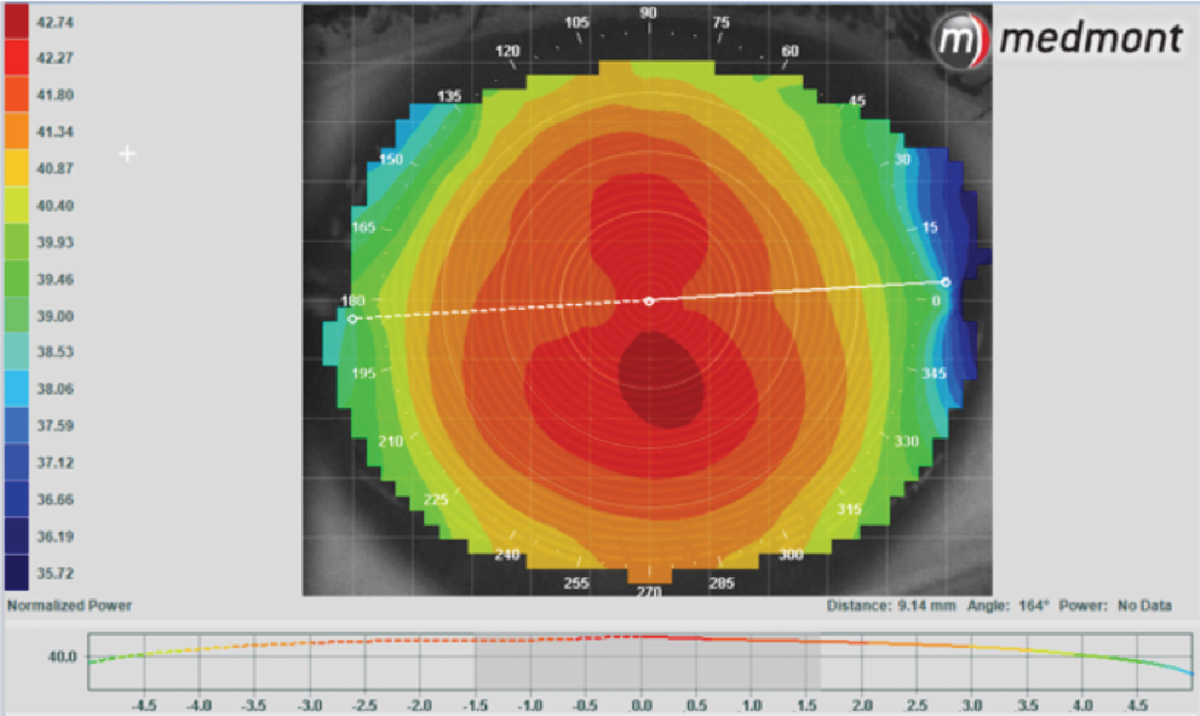 |
|
Axial map of a normal cornea. Click image to enlarge. |
Corneal Shape
The beautiful thing about topographers is that we can learn so much about the shape of the cornea before we start a contact lens fitting. Eccentricity and the shape factor are two values that can help us better understand the change in curvature of the cornea from the center to the edge.
Eccentricity (E value) is the rate of flattening from the center of the cornea towards the edge. Normal corneas have an E value that ranges between 0.4 to 0.6.7 To visually understand E values a little better, look at Table 1.7
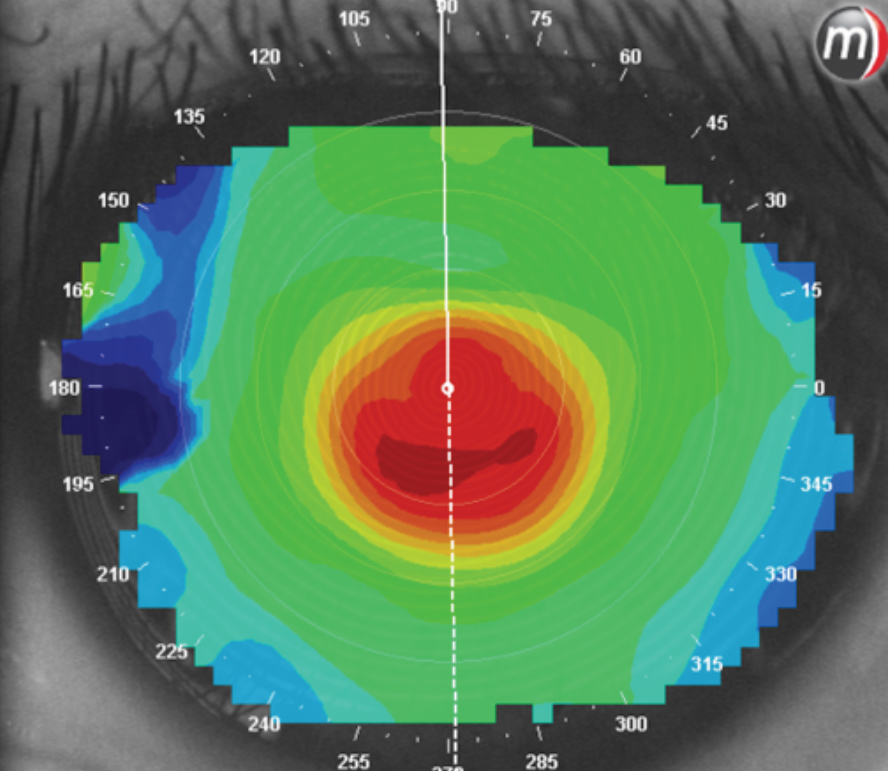
A prolate cornea is steep in the center and flattens outwardly toward the limbus. Prolate can be used to describe a normal cornea or even an ectactic cornea, such as nipple cone keratoconus and keratoglobus. Keratoconic eyes are just very highly prolate. A prolate cornea can be well described by an E value.
Oblate corneas are flat in the center and steepen towards the edge of the cornea.8,9 A patient who has undergone LASIK, post-keratoplasty, post-ortho-K lens wear, as well as some pellucid marginal degeneration cases are all examples of oblate corneas. Soft contact lenses are designed for prolate corneas.
When you place a soft contact lens on an oblate cornea, the optic zone of the lens may compress towards the globe with each blink, causing vision to fluctuate. Understanding this anomalous shape before starting a contact lens fitting allows you to select a contact lens modality best suited for success on these irregularly-shaped surfaces.
 |
|
Elevation maps of two different patients. Both have a reference sphere, from which the maps were created. The patient on the left has a very uniform elevation and was successfully fit with a spherical GP. The patient on the right has a very irregular elevation pattern and, with the scar in the inferior cornea, could only be fit with a very customized scleral lens. Nothing would stay on the eye without falling off. Click image to enlarge. |
Shape factor is another way to describe the rate of flattening of the cornea outwards from the center; the difference is that it can be used to describe both prolate and oblate corneas. There are several different methods that can be used to calculate the shape factor, each having their own reference point. A reference sphere can have a shape factor of either zero or one depending on which calculation method is used. A shape factor below sphere reference value would describe an oblate eye, and above would describe a prolate eye. Knowing the calculation method—and, more important, the reference point for your topographer—is important to understand how to interpret the shape factor.
Using the various indicators of corneal shape can help understand the cornea and assist in lens design. This data demonstrates that the majority of corneas are flatter nasally, which can cause soft lenses to decenter towards the nose. We also know that GP lenses tend to center over the steepest apex of the cornea. Knowing where the steepest apex is allows us to better predict if a lens will decenter. Using these tools to predict the performance of our various lens designs on-eye has been a time-saving approach in my clinic.
 |
|
The left image is an axial map of an ortho-K patient with a great fit, great vision and much happiness. The right image shows the tangential map, which defines the edges of the cornea and shows a complete ring of treatment around the central treatment zone. The tangential map gives us a clear, complete picture of what is going on with this ortho-K fit. Click image to enlarge. |
Fitting Soft Lenses
Truthfully, when fitting soft contact lenses (spheres, torics or multifocals), we don’t often think of using topography to assist in our fitting process. We typically have one diameter and one base curve per lens design and are highly successful with them. Ordering a specialty lens is rarely indicated for soft lenses based on a fitting issue and more frequently needed based on power availability. When there are two base curve options, we generally use our autorefractor K readings and choose one. When on the eye, if the lenses are found to be either too steep or too flat on the eye, then we switch to the other base curve option if the direction of change correlates with the available second base curve option or we try a different brand entirely.
Table 1. Relating Corneal Shape to E Values | |
| Shape | E Value |
| Sphere | 0 |
| Ellipses | 0-1 |
| Parabolas | >1 |
| Hyperbolas | <1 |
We have been spoiled by the wonderful lens technology available to us; the soft lenses of today have been engineered to work well on the vast majority of our patients and often with the first lens we try. If the fit is not successful, our topographers now play a larger role in helping troubleshoot why we are not getting the predictable and ultimately highly successful outcomes we have come to expect with these lenses.
Despite the ease in fitting soft lenses, the argument can be made that topographies should be used to establish a baseline before every contact lens fit. Soft contact lenses can cause corneal compression or corneal edema if fit too tight, if on eyes with tight lids or if over-worn.10 Using baseline measurements for comparison, we can monitor the cornea as the fitting progresses to look out for these issues. If vision decreases, topographies compared with baseline images can show change over time, ruling out or revealing corneal changes.
 |
|
A central cone that signals a highly prolate cornea. Click image to enlarge. |
Astigmatism
Perhaps the most familiar use of these tools is for establishing magnitude of astigmatism. Keratometers and autorefractors provide central K readings, which guide us as to whether our patients have corneal astigmatism. Topographers take this a step further and outline exactly the type, shape and magnitude of this astigmatism. Regular vs. irregular, with-the-rule or against-, central or limbus-to-limbus are all distinctions a topographer can provide.
When I think of with-the-rule astigmatism, I think of a face stretched horizontally. The flat meridian or least power is along the horizontal and the steep more minus power is along the vertical. This form of astigmatism is more common. The opposite depiction is true for against-the-rule astigmatism. Picture a vertically stretched long face. The flat meridian is along the vertical and the steep meridian along the horizontal.
 |
|
A patient with normal corneas who overwore their soft one-day disposable lenses caused a compression right on their peripheral cornea, as seen on a tangential map. Click image to enlarge. |
Toric soft lenses are stabilized to fit these astigmatic corneas. Stabilization techniques vary from brand to brand but all are designed with a combination of thick and thin zones to best center or orient the lens on-eye. Optimizing the design to the type and distribution of astigmatism can help troubleshoot to minimize rotation, decentration and excessive movement.
Soft Multifocal Lens Fitting
Baseline topographies can also help us understand if the corneal and visual axes are aligned. The size of the pupil and lens centration are critically important to multifocal lens performance.11,12 If a lens is decentered, the best optics of the lens will not be in the center of the pupil or on the visual axis. If our line of sight and geometric center of the cornea do not line up, then there is a natural decentration inherent in the eye. You can determine this with your topographer; if you ask a patient to look straight ahead and your mires on not centered on the cornea, you know that natural alignment is off.
You can fix this for imaging by asking the patient to look either right or left to better center the mires on the cornea, but when this happens we know that the center of the cornea and the visual axis are not in line with one another. When patients do not perform well with multifocal contact lenses, this may be the reason. Knowing that a patient is naturally visually decentered before you start a multifocal fit may impact your decision to move forward with the fit, to set realistic expectations of the visual potential or on the complexity of the fit, which may require more of your time.
Another little trick that you can use with multifocal lenses is to take a topographical scan of the lens on-eye. The tangential map will show the power distribution of the lens on-eye. You can identify if the optic zone of the lens is centered over the pupil as desired.
 |
|
Regardless of which technology we choose to use, corneal topographers are more than just colorful maps of our patient’s eyes. They provide a wealth of information and have a wide variety of applications. Click image to enlarge. |
Software-guided Lens Fitting
There are many different programs that are starting to become available that allow you to fit GP and scleral contact lenses. Profilometry describes scleral lens topographers— e.g., the Eaglet Eye Surface Profiler, Oculus Pentacam, sMap 3D (Visionary Optics)—that are designed to help practitioners with choosing the first lens to start your scleral lens fitting.
There are software programs available that will help you visualize and design a fit of a gas permeable lens. This software is built into topographers, one of the first being the Medmont. You can see what the fluorescein pattern would like for specific lens on the eye, modify parameters and see how those changes would impact your fit—all before you order a lens.
Other programs that also do this include the EyeSpace and Wave contact lens programs.
 |
|
This patient has astigmatism. It is a regular form that stretches from limbus to limbus and is with-the-rule. Click image to enlarge. |
Takeaways
The art of fitting contact lenses stems from a relationship between the contact lens and the cornea. With all the advanced lens technologies available to us, it seems considering corneal shape has largely gone by the wayside in soft lens fitting. Even the best soft lenses fail us on occasion, and our topographers can often save the day with an explanation of why. Having baseline topographies helps us identify fits that may be more challenging. Knowing this from the start of a fit will allow you to properly educate your patient and set realistic expectations of the process that lies ahead. When you take a few minutes to do these steps before a fit begins, you can increase the success of your fits, reduce frustration and speed up your decision-making process.
Ultimately, an understanding of corneal shape remains a valuable tool in optimizing the soft lens experience for our more challenging patients and in monitoring their success over time, and topographers will continue to be beloved and worthwhile investments in a contact lens practice.
Dr. Pal runs a group practice in Toronto specializing in speciality contact lenses, myopia management and ocular aesthetics. She is a Fellow for the American Academy of Optometry, Scleral Lens Education Society and British Contact Lens Association. She is a consultant for Allergan, Alcon, Bausch + Lomb, CooperVision, Johnson & Johnson Vision Care and Menicon, as well as a facilitator of the CooperVision STAPLE lens fitting workshops.
1. Kojima R. Validating corneal topography maps. CL Spectrum. July 1, 2007. www.clspectrum.com/issues/2007/july-2007/validating-corneal-topography-maps. Accessed March 17, 2022. 2. Erdélyi B, Csákány B, Németh J. Spontaneous alterations of the corneal topographic pattern. J Cataract Refract Surg. 2005;5(31):973-8. 3. Muller-Breitenkamp U, Hockwin O. Scheimpflug photography in clinical ophthalmology. a review. Ophthalmic Res. 1992;24 Suppl 1(0030-3747):47-54. 4. Lebow K. Learning the intricacies of axial and tangential maps. CL Spectrum. September 1, 1999. www.clspectrum.com/issues/1999/september-1999/learning-the-intricacies-of-axial-and-tangential-m. Accessed March 17, 2022. 5.. Klein SA. Corneal topography reconstruction algorithm that avoids the skew ray ambiguity. Optom Vis Sci. 1997;74(11):945-62. 6. Dehghani C. The elevation map best fit sphere as starting point for gas permeable contact lens fitting. Presented at AAO Meeting 2012. November 2012. www.aaopt.org/detail/knowledge-base-article/elevation-map-best-fit-sphere-starting-point-gas-permeable-contact-lens-fitting. Accessed March 17, 2022. 7. Hansen D. Evaluating the eye with corneal topography. CL Spectrum. August 1, 2003. www.clspectrum.com/issues/2003/august-2003/evaluating-the-eye-with-corneal-topography. Accessed March 17, 2022. 8. Lebow K. Are all aspheric contact lenses created equal? CL Spectrum. February 1, 1999. www.clspectrum.com/issues/1999/february-1999/are-all-aspheric-contact-lenses-created-equal. Accessed March 17, 2022. 9. Scholz K, Messner A, Eppig T, et al. Topography-based assessment of anterior corneal curvature and asphericity as a function of age, sex, and refractive status. J Cataract Refract Surg. 2009;35(6):1046-54. 10. Cook GW, Benton MG, Akerly W, et al. Structural variation and its potential impact on genome instability: Novel discoveries in the EGFR landscape by long-read sequencing. PLOS One. 2020;15(1):ee0226340 11. Papatadou E, Del Águila-Carrasco AJ, Esteve-Taboada JJ, et al. Objective assessment of the effect of pupil size upon the power distribution of multifocal contact lenses. Int J Ophthalmol. 2017;10(1):103-8. 12. Fedtke C, Ehrmann K, Thomas V, et al. Association between multifocal soft contact lens decentration and visual performance. Clin Optom (Auckl). 2016;8:57-69. |


