In the past few years, the standard of care for keratoconus has transitioned to more effective use of contact lenses and earlier surgical treatment to arrest or delay the progression of the disease as well as improve visual acuity. Minimally invasive surgical treatments including collagen crosslinking (CXL) and intrastromal corneal ring segments (ICRS) are aimed at replacing or delaying the need for corneal grafting. These procedures represent the culmination of centuries of research—so how do they measure up against current and preceding treatments? What innovations are we and our patients now enjoying, and what’s on the horizon for the near future? This article will trace the path of evolution in one of eye care’s most persistent challenges.
Historical Standards of Keratoconus Care
Burchard Mauchart, a professor at the University of Tübingen, Germany, first described keratoconus in a doctoral dissertation in 1748 as staphyloma diaphanum.1,2 Previously, there was scant mention of this condition in the literature and many physicians simply called it ochlodes, which translates from Greek to mean “annoying.”3 However, it wasn’t until 1854 that British physician John Nottingham, in a 270-page treatise, clarified this condition as a corneal ectasia. Naming it “conical cornea,” Nottingham described several hallmark features of the disease, including the distinct cone shape and thinness of the cornea, which became the modern definition we use today.3
In 1859, British surgeon William Bowman was the first to use an ophthalmoscope to observe the condition, and many of his clinical insights are still used to diagnose the disease today.4 The condition was finally given its modern name, keratoconus, meaning “horn-shaped cornea” in a thesis by Swiss physician Johann Horner in 1869.4
At that time, keratoconus was commonly treated with chemical cauterization with silver nitrate.2 Results were less than optimal, and in 1888 a blown glass contact lens by Fick was introduced for the purpose of compressing the cone—one of the earliest uses of contact lens technology. Polymethylmethacrylate (PMMA) scleral lenses were subsequently introduced as another method by American optometrist William Feinbloom in 1936.4
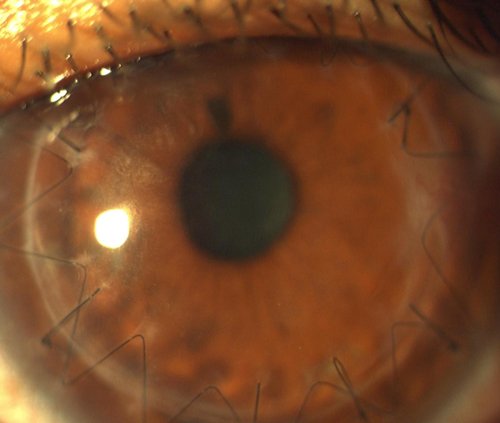 | |
| A successful corneal transplant, using a continuous suture technique, in the early postoperative period. |
In 1936, Spanish-American oph-thalmologist Ramon Castoviejo Briones successfully performed the first corneal transplant.4 Then in the late 1970s, American chemist Norman Gaylord was credited with a key role in developing gas permeable (GP) contact lens materials. Corneal GP lenses remained the medical treatment of choice for keratoconus for over 40 years.
Challenges with the Current Standard
When well fit and tolerated, corneal GP lenses correct visual acuity far better than spectacles.5 However, they do come with downsides: first and foremost, the number one challenge with corneal GP lenses is comfort. Even long-term wearers who adapt to the feeling rarely describe their lenses as truly comfortable. If environmental debris becomes trapped under the lenses, it must be removed immediately to avoid piercing pain.
Most corneal GPs are designed to translate upon blink in the lid-attachment style of fitting. This lens movement annoys many patients both sensorially and in the momentary fluctuation of vision, yet it is rarely addressed by practitioners. The interpalpebral style of fitting, in which the lens does not tuck under the lid at all and resides between the open eyelids in the interpalpebral space, is harder to achieve and is potentially problematic with keratoconus since the apex of the cone is rarely located in geometric center of the cornea and the lens will seek the apex of the cone. This lens fit is typically reserved for special circumstances, such as in the case of Graves disease or the presence of a bleb.
In addition to fitting style, practitioners have also debated which type of fitting against the apex of the cone is best. The Collaborative Longitudinal Evaluation of Keratoconus (CLEK) studies show an association between flat fitting lenses or compression of the apex of the cone and corneal scarring.6,7 Because CLEK was not a prospective multicentered randomized trial, causality could not be established; however, is it generally agreed upon that an apical clearance type fit reduces the risk of scarring in keratoconus.8 The problem with apical clearance fitting is that practitioners report compromised comfort and visual acuity. And with either fitting philosophy, as soon as the patient blinks and there is translation of the lens, the peripheral curve system contacts the corneal apex.
Attempting to improve comfort, practitioners began adding tandem or “piggyback” systems. Such a system involves fitting an optimal corneal GP with the addition of a disposable soft lens underneath. The theory of adding a piggyback is that the upper eyelid first contacts the soft edge, which acts as a ramp to the edge of the GP lens. Piggyback systems seem to stabilize and center GP lenses better than GP lenses alone. It is also theorized that a piggyback soft lens cushions against the apex of the cone and provides some measure of protection against the apex of the cone.
Vaulting Lenses
With the decrease in emphasis on corneal transplantation and the shift toward less invasive surgical procedures in the era of partial-thickness lamellar keratoplasties, surgeons have renewed their interest in ensuring keratoconic patients are fit optimally in contact lenses. Contact lenses complement these less invasive procedures and are almost universally necessary to achieve optimal vision. Based on the growth rate in industry data, prescribers are increasingly choosing vaulting strategies over traditional corneal GP lenses for patients with keratoconus.9
Vaulting contact lenses include both hybrid and scleral lenses. When properly designed, vaulting lenses never touch the apex of the cornea and move very little, if at all. Vaulting the apex of the cone is the best way that we know to avoid corneal scarring based on the CLEK criteria.10 With hybrid lenses, there is a tear pump under the lens, as evidenced by the loss of sodium fluorescein under the lens with time. When properly fit, hybrid lenses provide adequate oxygen supply to the cornea.11 Similarly, with properly fit scleral lenses, dissolved oxygen in the fluid of the significant post-lens tear reservoir and diffusion from the atmosphere maintains adequate corneal physiology.12 Scleral lenses are accommodating corneas that have been far too steep to fit with corneal GP lenses or may have failed with other modalities.13
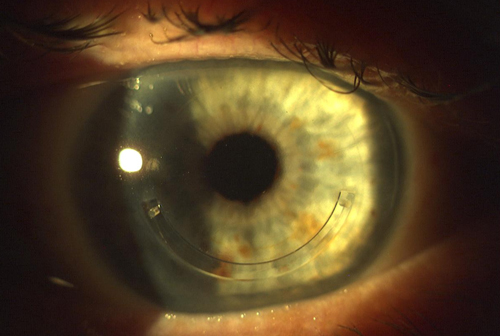 | |
| A single Intacs segment implanted in the mid-stromal region of a patient with keratoconus. |
Corneal Crosslinking
Practitioners the world over—minus the United States—have in recent years been able to treat keratoconic patients with one of the biggest advances in modern times: corneal collagen crosslinking using a combination of topical riboflavin and ultraviolet light to strengthen the cornea and arrest progression of the condition. The traditional procedure, or Dresden protocol, is completed after removal of the corneal epithelium. Trans-epithelial CXL is performed with an intact epithelium and has a mildly reduced risk of complications; however, studies have not confirmed that it has equal efficacy with regards to corneal stabilization. For this reason, many surgeons still prefer epithelium-off CXL.14
In late 2014, a project aimed at reaching a global consensus on the treatment of keratoconus and other ectatic diseases brought together 36 experts from the Asian Cornea Society, Cornea Society, EuCornea and PanCornea corneal societies. With regards to surgical management of keratoconus, the representatives reached a consensus that surgery should be considered for contact lens patients who are not able to obtain satisfactory best-corrected vision, meaning either those who could not achieve good corrected vision with contact lenses or those who are unable to tolerate or wear them comfortably.15
The panel determined that corneal collagen crosslinking in particular was important for the treatment of keratoconus with documented progression and recommended that it should be considered for this group of patients of any age. The panelists also indicated that CXL was important for treatment of keratoconus with a perceived risk of progression, but where progression has not yet been confirmed. The panel indicates that for eyes with contact lens intolerance or poor visual acuity with contact lenses, ICRS may be considered.15
CXL has been used safely in Europe for over 15 years but remains unapproved by the FDA in the United States. In February 2015, the FDA Dermatologic and Ophthalmic Drugs Advisory Committee and Ophthalmic Devices Panel of the Medical Devices Advisory Committee voted in support of approval of Avedro’s crosslinking system for the treatment of progressive keratoconus or corneal ectasia following refractive surgery. Despite the FDA advisory committee decision, however, the FDA ultimately decided in March 2015 to hold approval for the procedure and device. At this time, the exact timeline for approval and on-label treatment remains uncertain, but many clinics throughout the US are already performing the procedure on an off-label basis at an out-of-pocket expense to the patient or as part of clinical trials.16
Intrastromal Corneal Ring Segments (ICRS)
The most common ICRS are Intacs, which are semicircular inserts made of PMMA. During this procedure, small channels are created in the corneal stroma using a femtosecond laser (though a manual instrument can also be used) and the rings are inserted into these channels to reinforce and remodel the corneal structure. A single segment or two segments can be implanted based on topographic parameters and refractive state.
ICRS implantation results in moderate corneal flattening, with studies citing a range of 1.5D to 7.8D of flattening effect. Returning to contact lens wear is often an important goal of implantation, and studies indicate a variable rate of success at achieving this goal ranging from 33% to 100%. By redistributing corneal stress, ICRS are considered by many to be a therapeutic option to delay the progression of corneal ectasia. This thought is supported by some literature, but is not yet a clear consensus among practitioners. More research regarding this topic is indicated.14,17
Intacs segments were first FDA-approved for treatment of low myopia in 1999. In 2004, the FDA approved Intacs for treatment of keratoconus under a Humanitarian Device Exemption. Because the procedure is FDA approved, it is covered by many medical insurance panels. Complications of ICRS, though rare, include microbial keratitis, cornea thinning in the area over the segment, extrusion, reduced corneal sensation, neovascularization, persistent epithelial defects, corneal haze, corneal melting and uveitis.14
CXL and Intacs implantation can be used together and have been suggested to have a synergistic effect, with the ICRS achieving primarily corneal flattening and CXL achieving primarily corneal stabilization. CXL can be performed before, during or after ICRS implantation, but the ideal sequence is currently unknown.18
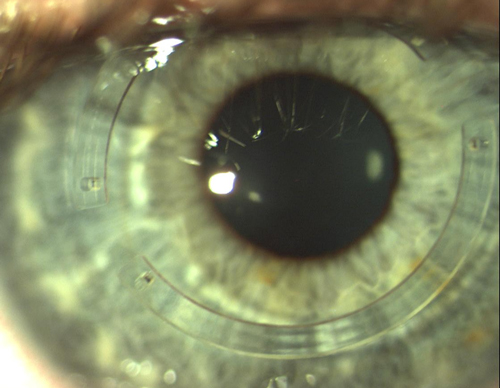 | |
| A keratoconic patient treated with implantation of dual Intacs segments. |
Transplantation
Whereas full-thickness penetrating keratoplasty (PKP) historically has been the mainstay of treatment for keratoconus, corneal transplantation is now generally reserved for eyes that are unable to achieve functional vision with other surgical or nonsurgical modalities due to scarring or contact lens intolerance. PKP has become increasingly successful due to advances in microsurgical techniques, including the use of the femtosecond laser. Advances in eye banking, corneal preservation and treatment of postoperative complications have also improved success rates. Nevertheless, risk of rejection is always possible: data from the Australian Corneal Graft registry indicates a 91% successful PPK graft rate at one year postoperatively and a 74% success rate at five years. Even when the graft is anatomically successful and clear, irregular astigmatism, contact lens intolerance and other complications can cause poor visual function.19
Deep anterior lamellar keratoplasty (DALK) is now preferred over PKP for conditions anterior to Descemet’s membrane, including keratoconus. In DALK, the pathological corneal stroma is removed to the level of Descemet’s membrane and then a donor graft is placed. It has several advantages over PKP including preservation of the endothelium, reduced use of postoperative steroids and faster visual rehabilitation. An intact host endothelium reduces the risk of graft rejection and keeps the procedure safer as it remains extraocular.18
Over history, we have come a long way in the treatment of keratoconus. New options for treating both medically with contact lenses and surgically have changed the standard of care for this condition. Vaulting contact lenses will potentially significantly reduce the risk of central corneal scarring and accommodate much more severe corneas, further relegating full-thickness corneal transplantation to a relic of the past.10 And when CXL is eventually approved in the US, we will again see the standard of care shift.
Dr. Sonsino is a partner in a specialty contact lens and anterior segment practice in Nashville, diplomate in the cornea, contact lens and refractive therapies section of the AAO, council member of the cornea and contact lens section of the AOA, fellow of the Scleral Lens Education Society and GPLI advisory board member.
Dr. Rock is a consultative optometrist at Wang Vision Institute who advises keratoconus patients on nonsurgical and surgical treatment options, including corneal crosslinking, Intacs, and corneal transplantation. He is also the clinical study coordinator for an FDA Phase III corneal crosslinking clinical trial.
Dr. Wang is the director of Wang Vision Institute, where he performs Intacs, corneal crosslinking and corneal transplantation procedures for patients with keratoconus and corneal ectasia. He is also the principal investigator for an FDA Phase III corneal crosslinking clinical trial.
1. Kinoshita B, Choo J, Caroline P, Andre M. Etiology, diagnosis and management of keratoconus: new thoughts and new understandings. Pacific University College of Optometry. 2008, 12-15.
2. Michaud Biographie Universelle (2nd ed). Delagrabe, 1843-1865; 27:301-02.
3. Grzybowski A, McGhee C. The early history of keratoconus prior to Nottingham’s landmark 1854 treatise on conical cornea: a review. Clin Exp Optom 2013.
4. Abedelaziz L, Barbara R. History of the development of the treatment of keratoconus. International Journal of Keratoconus and Ectatic Corneal Diseases, Jan-April 2013; 2(1): 31-33.
5. Mrazovac D, Barisić Kutija M, Vidas S, et al. Contact lenses as the best conservative treatment of newly diagnosed keratoconus—epidemiological retrospective study. Coll Antropol. 2014 Dec;38(4):1115-8.
6. Zadnik K, Barr JT, Steger-May K, et al. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005 Dec;82(12):1014-21.
7. Edrington TB, Szczotka LB, Barr JT, et al. Rigid contact lens fitting relationships in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Optom Vis Sci. 1999 Oct;76(10):692-9.
8. Korb DR, Finnemore VM, Herman JP. Apical changes and scarring in keratoconus as related to contact lens fitting techniques. J Am Optom Assoc. 1982 Mar;53(3):199-205.
9. Bennett, E. GP Annual Report 2012 Contact Lens Spectrum, Volume: 27, Issue: October 2012, 26-39.
10. Schornack MM, Patel SV. Scleral Lenses in the Management of Keratoconus. Eye Contact Lens. 2010 Jan;36(1):39-44.
11. Lee KL, Nguyen DP, Edrington TB, Weissman BA. Calculated in situ tear oxygen tension under hybrid contact lenses. Eye Contact Lens. 2015 Mar;41(2):111-6.
12. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012 Dec;35(6):266-71.
13. Segal O, Barkana Y, Hourovitz D, et al. Scleral Contact Lenses May Help Where Other Modalities Fail. Cornea 2003;22(4):308-10.
14. Ziaei M, Barsam A, Shamie N, et al. Reshaping procedures for the surgical management of corneal ectasia. J Cataract Refract Surg. 2015;41(4):842-872.
15. Gomes JAP, Tan D, Rapuano CJ, et al. Global Consensus on Keratoconus and Ectatic Diseases. Cornea. 2015;34(4):359-369.
16. FDA Does Not Approve Avedro’s Corneal Cross-Linking Platform Application, Requesting Additional Information. EyeWireToday. 2015.
17. Bedi R, Touboul D, Pinsard L, Colin J. Refractive and topographic stability of Intacs in eyes with progressive keratoconus: five-year follow-up. J Refract Surg 2012; 28:392–396.
18. Özertürk Y, Sari ES, Kubaloglu A, et al. Comparison of deep anterior lamellar keratoplasty and intrastromal corneal ring segment implantation in advanced keratoconus. J Cataract Refract Surg. 2012;38(2):324-332.
19. Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41(1):41-46.


