Since the early 1990s, more than 17.4 million eyes have undergone excimer laser vision correction (i.e., PRK, LASIK and LASEK) worldwide. The procedure could be said to be the most successful refractive surgery based upon the absolute number of procedures performed—and also one of the most controversial. Entire web sites are devoted to publicizing poor surgical outcomes and marketing misrepresentations, both real and perceived. Critics argue that surgeons fail to adequately disclose the risks associated with the procedure and overpromise on results.
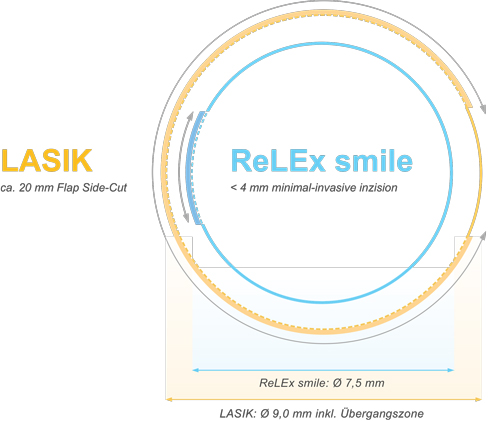 | |
Difference in corneal incision in LASIK vs. SMILE.1 Image: www.premiumeyes.de/de/augenlasern/relax-versus-lasik. |
Surgical procedures such as LASIK can be seen as both success stories and failures at the same time, depending on one’s evaluation criteria. Baseball legend Reggie Jackson is still considered one of the premier power hitters in the sport, but he also holds the dubious distinction of most recorded strikeouts. LASIK, too, has achieved successes that few other surgeries have matched, but still has failed to reduce complication rates to negligible levels. Complications well documented in the literature include post-surgical irregular astigmatism, epithelial ingrowth into the flap interface, postoperative dry eye and over- and undercorrection. Post-surgical interventions—such as surgical retreatment, corrective lenses, ocular surface therapies—remain higher than patients or practitioners would like.
Our practice is one of the US sites engaged in studies of a new procedure striving to overcome these limitations. This article shares our anecdotal impressions and provides an overview of the concept. Note: the surgical procedure was developed in conjunction with Carl Zeiss Meditec, and our practice receives research funding and consultation fees as part of its ongoing development.
Less is More
Currently, our practice and four others in the United States are investigating a new refractive surgery technique that seeks to reduce complications, side effects and retreatments needed compared with excimer-based methods. All-femtosecond corneal refractive surgery—known as small-incision lenticule extraction (SMILE)—differs from traditional LASIK in that the excimer laser is not used for tissue sculpting, nor is any photoablation performed. Instead, a lenticule of tissue is created using the femtosecond laser and removed manually through a short arc-length incision.
Additionally, rather than creating a hinged-flap lift, two passes of the femtosecond laser are performed: the first pass creates the posterior aspect of the lenticule and a peripheral stromal bed, while the second creates the anterior surface of the lenticule and one or two small access incisions of approximately 60 degrees at the 7.5mm optical zone. This gives the surgeon an entrance to dissect the remaining corneal attachments of the anterior and posterior surfaces and remove the lenticule through a small incision, usually 3mm or less.
The SMILE procedure was developed at six sites on three continents. Reported clinical outcomes suggested refractive results that mirror current LASIK outcomes, with predictability measures indicating that 95% of the eyes are +/- 0.5D from refractive target. With SMILE, outcomes are similar for low, moderate or high myopia; the same cannot be said for LASIK, where refractive accuracy diminishes as myopia increases.
Efficacy rates for the SMILE procedure from international study centers have demonstrated that 95% of treated eyes achieve at least 20/30 uncorrected distance visual acuity at three months for even moderate to high myopia levels (data on file, CZM). Safety results seem promising, with only 1% to 2% of eyes losing two or more lines of best spectacle-corrected visual acuity. Refractive stability is typically achieved at one week, with little to no change seen between this interval and the one and three month data sets.
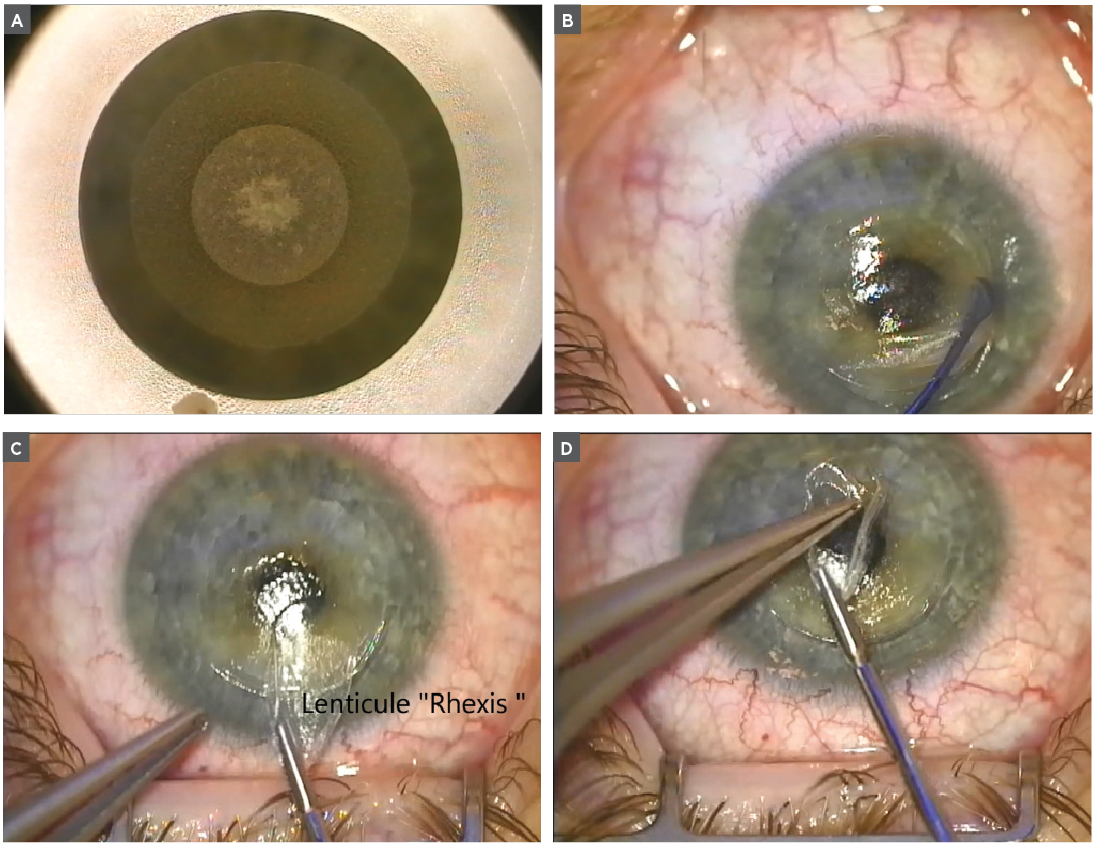 | |
A SMILE procedure: (A) A femtosecond laser creates a lenticule of tissue and an access port; (B) the surgeon dissects between tissue planes anteriorly and posteriorly of the lenticule; (C) the lenticule is detached and removed through the corneal incision in a "rhexis"-like procedure similar to that of cataract surgery; (D) the lenticule is then placed on the front of the corneal epithelium for inspection. |
Summary of Benefits
The advantages of the SMILE concept are numerous. The use of femtosecond laser technology reduces the invasiveness of the procedure and also removes the possibility of flap dislocation. Additionally, the cornea inherently maintains a greater biomechanical structure and fewer corneal nerves are incised; as a result, a lower frequency of dry eye complaints and a shorter healing cycle are expected. As in LASIK, contact lenses can be worn after SMILE.
However, because of the newness of the procedure, several considerations remain unknown. At this point, we have limited data on procedure success and complications beyond five years. Our experience with other lamellar techniques suggests that we may be able to surmise that what we see early (i.e., at three months) will persist long-term (i.e., beyond five years), but this remains speculative at this time. More research is also needed on certain details of the procedure. For example, can small refractive errors (i.e., 1D or less) be effectively treated, and what approach will be taken for small residual refractive errors after an initial SMILE procedure has been performed? With LASIK, we do treat less than 1D for primary procedures and enhancements. Enhancements with SMILE are currently done by creating a LASIK flap or performing a PRK procedure.
There are at least a handful of theoretical and speculative benefits of SMILE as compared to LASIK. Eliminating flap creation leads to complete avoidance of flap displacement, dislodgement and slippage with associated epithelial ingrowth. Additionally, because of its minimally invasive nature, the procedure negligibly violates Bowman’s layer and excises less of the anterior stroma. SMILE’s diameter of treatment field is typically 7.5mm, while in LASIK the treatment field is usually at least 8.5mm. This smaller diameter leads to improved corneal tensile strength by preserving the most biomechanically significant anterior one-third of the cornea. Since there is greater preservation of the anterior cornea with less corneal nerve interruption, one would speculate that fewer dry eye complaints from neurotrophia would occur.
Another unique feature of SMILE is that it is completed intrastomally—for all intents and purposes, it is completed in a vacuum. By contrast, the excimer laser energy must traverse the final lens in the optical train of the laser and pass the air environment of the working distance to the environmentally exposed corneal surface. Because of this, certain factors must be considered during the LASIK procedure—namely, air purity, humidity, barometric pressure and temperature of the operating room—that can affect the photoablation ability of the excimer beam and the amount of dry cornea removed with each pulse. This results from variable hydration of the tissue, which is dependent on the time from start to finish of the photoablation. In addition, this can change from case to case and surgeon to surgeon, in the same and variable environments. By performing the refraction treatment intrastromally, the SMILE procedure eliminates such variables. This explains why a -10D treatment is just as predictable as a -1D treatment with SMILE, compared with comparable excimer laser treatments. Similarly, in my personal experience, I have found a -1D SMILE procedure is just as predictable as a -1D excimer laser correction.
Despite these perceived benefits, only time will tell if SMILE can compete on the playing field of a commercial refractive practice. More research is needed to determine the predictability, effectiveness, stability of result, safety and quality of vision of the procedure, as well as reversibility and adjustability, minimal wound healing, immediacy of final refractive outcome and comparison with other vision modalities such as glasses and contact lenses. Although flap complications are obviated, other complications typical of refractive surgery (e.g., ectasia, residual refractive error, dry eye, infection, inflammation) are possible—but less likely, given the increased structural integrity and less invasive nature of the SMILE procedure.
Procedure counts provide an indication of SMILE’s ability to compete with LASIK. Approximately 20,000 SMILE procedures were performed by December 2012; this increased to 50,000 by the end of July 2013. Carl Zeiss Meditec reports that 200,000 eyes have undergone SMILE worldwide since February 2015 (data on file, CZM). It is clear SMILE is gaining interest among surgeons throughout the world. Pending FDA approval, will the same hold true for surgeons within the US? As more data continually becomes available, it will likely tell us what impact a femtosecond laser could achieve as a stand-alone refractive surgical device.
John F. Doane, MD, FACS, is a cornea and refractive surgeon with Discover Vision Centers in Kansas City, MO. He is also Clinical Assistant Professor at Kansas University Medical Center Department of Ophthalmology.
Jace Rickstrew is currently a second-year medical student at the University of Kansas.
1. Premium Eyes. Available at: www.premiumeyes.de/de/augenlasern/relex-versus-lasik. Accessed October 23, 2015.


