 |
A week later, vision had improved to 20/60 and the epithelium was nearly resolved. The BCL was removed and Pred Forte (Allergan) added to control scarring. After another week, the nasal central corneal ulcer remained. Current meds were discontinued and she was started on fortified vancomycin, tobramycin and ofloxacin and referred for tertiary care.
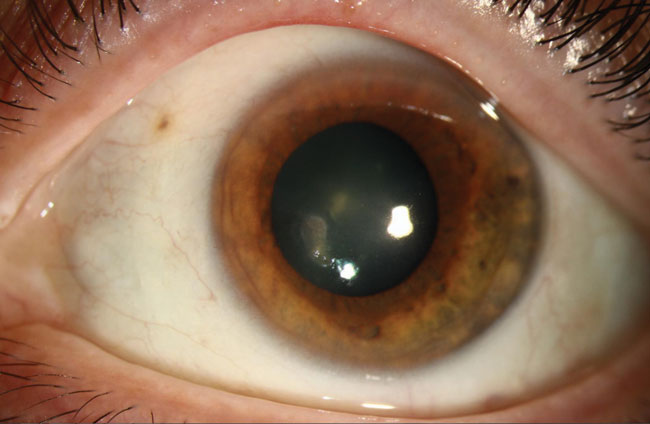
The clinical image below shows a small, ~1.5mm x 0.5mm paracentral area of subepithelial haze with feathery edges and surrounding corneal haze without stromal thinning. Confocal microscopy demonstrated multiple areas suspicious for trophozoites near Bowman’s membrane and several areas of branching elements in the mid to deep stroma.
Concern is for an amoebic keratitis as well as possible branching fungal elements. Recommend treatment for Acanthamoeba keratitis is PHMB and oral ketoconazole. The decision was made to hold off on treating for a superimposed fungal keratitis. A corneal biopsy was performed for further pathogenic characterization that will further guide treatment. Topical antimicrobials will continue until there is clinical improvement on anti-amoebic therapy.
 |
CALL FOR ENTRIES: If you have great clinical images of fascinating cases to share, send large, high resolution photos (corneal disease or contact lens wear only) and a brief case description to: [email protected].


