 |
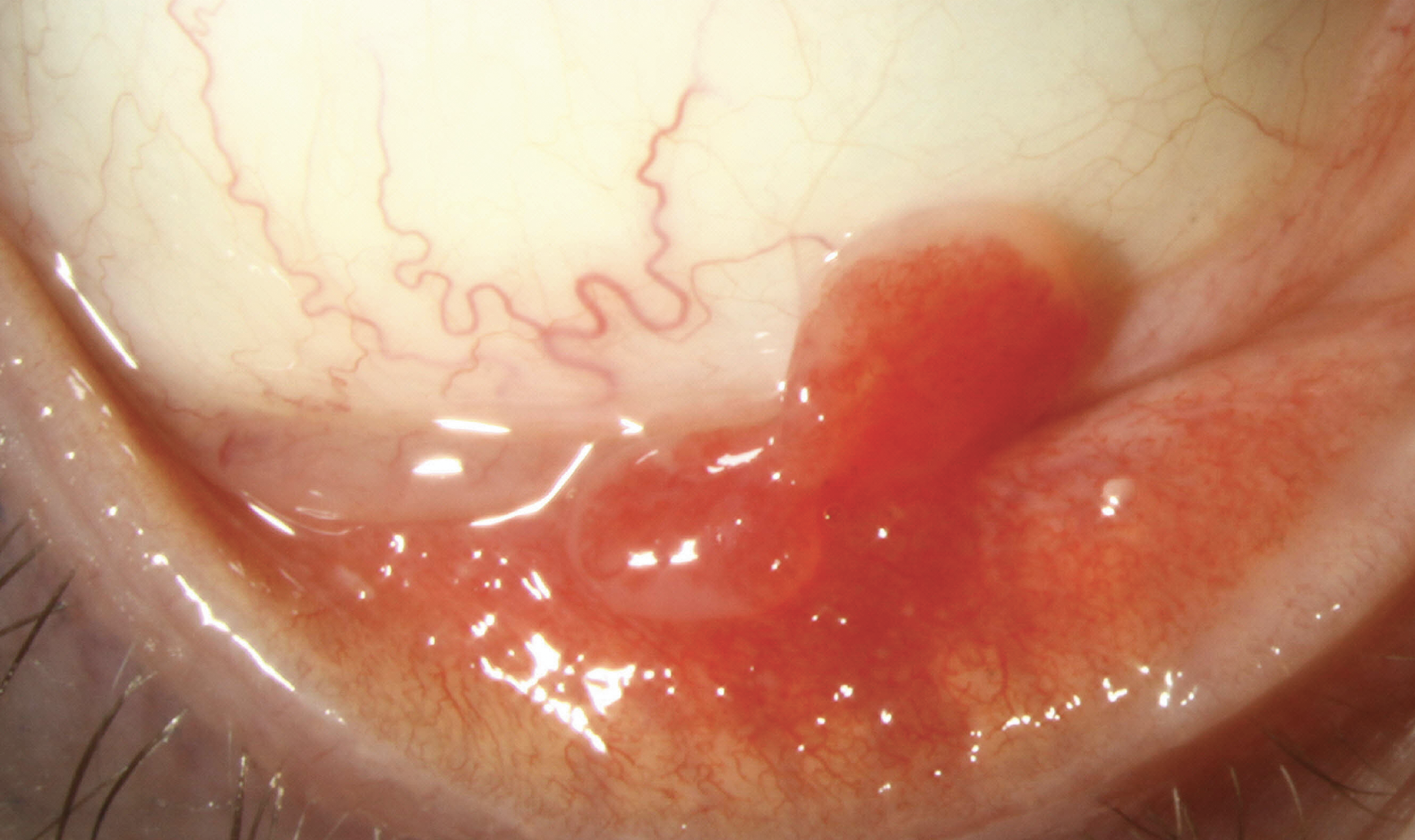
A 22-year-old male presented with concerns of a painless mass in his inferior fornix. His medical history was largely unremarkable except for the use of retinoid cream for the treatment of acne. Upon examination, a highly vascularized, pedunculated mass was observed growing from the inferior palpebral conjunctiva. He was diagnosed with a pyogenic granuloma (PG) and started on a course of topical steroids. It had resolved by his four-week follow up.
Conjunctival pyogenic granulomas are benign, non-neoplastic, fast-growing vascular proliferations located on either the palpebral or ocular surface conjunctiva. They often appear as fleshy, red, smooth, polypoidal or pedunculated nodules. PGs may bleed if disturbed. They are associated with chronic trauma (e.g., contact lens or foreign body irritation) pregnancy, viral infections, use of medications such as retinoids, antiretrovirals and anti-neoplastics, and Sturge-Weber syndrome. It has been proposed that tissue injury activates a neovascular pathway, promoting cell proliferation.1
 |
|
Click image to enlarge. |
There is no ethnic or gender predilection and PG may appear at any age, although it is more common in younger patients. PG resembles granulation tissue; however, histopathology shows branching endothelium-lined vessels with inflammation and edema without granuloma formation. PGs are classified as either a lobular or non-lobular capillary hemangioma. Fibrosis can be observed as the tissue regresses.
If left untreated, conjunctival PG may spontaneously regress; however, depending on the location and patient tolerance of the lesion, therapeutic treatment is recommended. Treatment options include excisional surgery, cryotherapy, electrocautery, laser ablation and topical medical therapy.
Medical therapy is the recommended first-line treatment for conjunctival PG. Options include topical steroids and topical β-blockers. While the anti-inflammatory effects of steroids have been the historical treatment, BID dosing with a nonselective β-adrenergic antagonist such as 0.5% timolol is growing in popularity. β-blockers cause vasoconstriction of blood vessels within the lesion, leading to vascular growth factor inhibition and cellular apoptosis. β-blockers also have a lower adverse event profile compared to steroids.
1. Godfraind C, Calicchio ML, Kozakewich H. Pyogenic granuloma, an impaired wound healing process, linked to vascular growth driven by FLT4 and the nitric oxide pathway. Modern Pathology. 2013 Feb;26(2):247-55. |


