Viral conjunctivitis is a common condition that presents in the offices of eye care practitioners. Because it is self-limiting, most of the time patients are advised to use artificial tears and monitor their symptoms. However, the process of recovery can often take two to three weeks and can be frustrating for patients because they are unable to attend school or work and must halt contact lens wear.
Patients with viral conjunctivitis may complain of itchy, burning, foreign body sensation and red eyes. They may also present with a history of upper respiratory tract infection or interaction with people with a red eye. Clinically, these patients may present with lid edema or erythema, watery discharge, palpable preauricular lymph node (PAN) and conjunctivitis—with or without corneal involvement. We’d like to introduce an ophthalmic treatment for viral conjunctivitis and present two case reports on applying this treatment regimen, as well as its follow-up and treatment outcome.
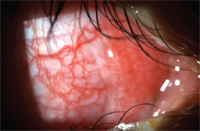
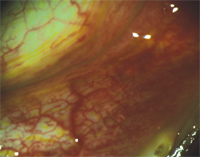
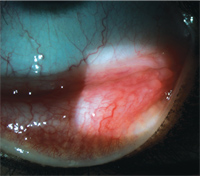
1. +2 Bulbar hyperemia and chemosis O.D.
Red, Itchy, Watery Right Eye
History: “John,” a 24-year-old male, complained of a red right eye, which started one day prior to the eye examination. He also reported mild-to-moderate itching, burning and a watery eye. He denied wearing contact lenses. John was in good general health without symptoms of cold of flu. He was not taking any medications and reported no known drug allergy.
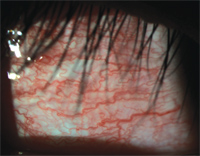
Diagnostic Data: Entering visual acuity was 20/20 O.D. and O.S. with normal pupillary responses and extraocular muscle movement O.U. Anterior segment evaluation was only significant for a +2 nasal bulbar conjunctiva injection and chemosis from two to five o’clock (figure 1). Moderate follicles and hyperemia were found in the right superior and inferior palpebral conjunctiva (figure 2). Eyelid, anterior chamber and corneas were unremarkable O.U. The rest of the anterior segment evaluation for the left eye was also unremarkable. There was no palpable preauricular lymph node (PAN) on either side of the face.
Diagnosis, Treatment and Management: John’s diagnosis was viral conjunctivitis O.D., without involvement O.S. He was treated in office with three drops of tetracaine and five drops of betadine 5% in the right eye. The betadine was wiped all over the upper and lower eyelid and lashes to maximize the treatment area with a gloved hand. Patient was asked to move his eye in all directions for one minute. The residual betadine was rinsed off thoroughly with saline solution to minimize residual ocular irritation from betadine. John was advised to return for day three, five and 14 follow-up or as needed.
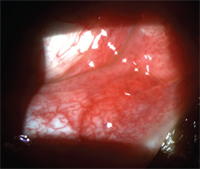
2. Moderate follicles O.D.
The patient returned for the day three follow-up and reported significant improvement in eye irritation (about 70% - 80% resolution). His right eye burned tremendously after the betadine treatment, but this sensation resolved after half a day. Bulbar conjunctival hyperemia was about grade 1 with trace chemosis (figure 3). Moderate follicles remained. John was very pleased with the fast recovery of the betadine treatment despite the initial burning.
The patient returned for day five follow-up and reported full resolution of the eye irritation. Bulbar conjunctival hyperemia was trace and chemosis had fully resolved (figure 4). Follicles appeared to be smaller, and the palpberal conjunctival injection was minimal (figure 5).
John returned for the final day 14 follow-up. He reported that his right eye continued to feel comfortable since the last visit. Viral conjunctivitis had completely resolved, and the patient was told to continue with routine eye examination.
Bilateral Red Eyes
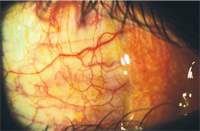
3. Grade 1 bulbar conjunctival hyperemia O.D.
History: A 20-year-old Asian female, “Sally,” presented to the eye clinic with a complaint of bilateral red, watery eyes for three days. She had onset of an upper respiratory infection two days prior to the red eyes. She did not wear contact lenses, was not taking any medications and reported no known drug allergy.
Diagnostic Data: Sally’s best-corrected acuities were 20/20 O.D., and O.S., with normal pupillary responses and extraocular muscle movement O.U. On slit lamp examination, there was +3 bulbar conjunctival hyperemia 360° in each eye (figure 6). A +3 follicular response was noted in the lower palpebral conjunctiva of both eyes (figures 7, 8). The corneas in both eyes were clear without subepithelial infiltrates. The anterior chamber was deep and quiet O.U. There was no palpable preauricular node on the right or the left side of the face. Both eyes had watery discharge.
Diagnosis, Treatment and Management: Sally was diagnosed with bilateral viral conjunctivitis without corneal involvement. She was educated about the treatment options for viral conjunctivitis and opted for the ophthalmic betadine therapy.
Treatment of previous patients revealed that a significant side effect of the therapy was ocular discomfort on the day of the procedure as well as corneal staining. Patients consistently reported an 8/10 pain response on day one of recovery. For Sally, additional steps were taken to minimize ocular discomfort. After anesthetic was instilled, one drop of Acular LS (ketorolac tromethamine, Allergan) was placed in the eye. The betadine therapy was applied with strict adherence to no more than 60 seconds of ocular surface contact—with treatment to the lids and lashes completed during this period as well. The saline irrigation was done extensively with close attention to irrigating under the upper and lower eyelids.
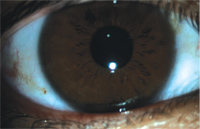
4. Clear cornea and bulbar conjunctiva O.D.
After the treatment was completed, another drop of Acular LS was instilled prior to the patient leaving the office. Sally was then instructed to use preservative-free lubricating drops every 30 minutes for the remainder of the day and then hourly while awake until follow-up two days later. In addition, two 200mg tabs of ibuprofen were suggested for pain every four to six hours, as needed.
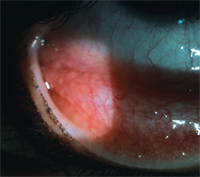
Sally returned for day three follow-up. She reported good compliance with the lubricating drops during the recovery period and that her discomfort was well controlled with the combination of the artificial tears and the oral ibuprofen. By the end of day one, her eyes were significantly more comfortable, and she awoke on day two with a feeling of 90% - 95% resolution of her conjunctivitis. The clinical exam revealed trace conjunctival hyperemia in each eye (figure 9), a +1 follicular reaction in the inferior palpebral conjunctiva O.U. (figures 10, 11) and significantly less palpebral hyperemia. Sally’s corneas were clear without subepithelial infiltrates, and she was discharged from care after this visit.
Discussion
Viral conjunctivitis is one of the most common causes of “pink eye,” and adenovirus is the most common agent for it. Three common types of viral conjunctivitis include epidemic keratoconjunctivitis (EKC), pharyngoconjunctivial fever and acute hemorrhagic conjunctivitis. Patients with EKC have significant subepithelial infiltrates and keratitis, and their vision can be affected. Patients with pharygoconjunctival fever also have systemic involvement, such as fever and sore throat; this type of conjunctivitis is often found in children. As the name “acute hemorrhagic conjunctivitis” suggests, conjunctival petechiae are often found.
5. Trace follicles O.D.
Some of the common treatments for viral conjunctivitis include artificial tears for ocular irritation, non-steroid anti-inflammatiory drugs (NSAID) for inflammation, antihistamine/mast cell stabilizers and cool compresses for the itchiness, topical steroids for subepithelial infiltrates, and topical antibiotic for corneal defects. Betadine, with its broad antimicrobial spectrum and low cost, has also been found in many studies to be useful in achieving quick resolution of some viral and bacterial conjunctivitis.1-5
Some potential side effects from betadine ophthalmic drops include conjunctival irritation, increased lacrimation, keratitis, papillary conjunctivitis, chemosis, conjunctival hemorrhage, dry eye, eye discharge, eye irritation, eye pain, eyelid edema, headache, red eye, reduced visual acuity and taste disturbance.6 Patients who were treated with betadine reported that the initial ocular discomfort lasted for about four - five hours in the treated eye. Some of these patients developed superficial punctuate keratitis post-betadine treatment.
Our original protocol (John’s case) did not involve using Acular LS and strictly followed the protocol proposed by the Betadine for EKC Study.6 The treatment inclusion criteria for the Betadine for EKC Study called for patients who are at least 18 years of age with symptoms for less than five days, those who have no active ocular allergies or hypersensitivity to iodine and those who have not been treated with any topical ocular medications.6 Our protocol was later modified (Sally’s case) to implement Acular LS prior to and after betadine instillation to reduce ocular inflammation secondary to betadine treatment. We have gotten good feedback from patients whose eyes we had treated with Acular LS in addition to the betadine treatment regimen. Additional studies have also reported that dexamethasone reduces ocular inflammation, resulting in improved ocular discomfort with the betadine treatment.5
6. +3 Conjunctival hyperemia.
Billing Pearls
When monitoring viral conjunctivitis without initiating treatment, only an EM 2 can be billed. However, once betadine treatment has been initiated, an EM 3 can be billed. A bottle of 30ml betadine 5% costs about $17.95, and a bottle of 15ml tetracaine 0.5% costs about $4.25. The per-drop cost of betadine is only about $0.03. It is also important to note and discuss with your patients that using betadine for treating viral conjunctivitis is considered off-label usage and that patients may respond differently to the treatment.
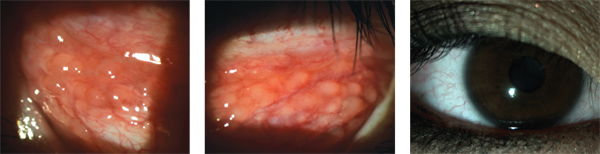
7. +3 Follicles inferior palpebral conjunctiva O.D.
8. +3 Follicles inferior palpebral conjunctiva O.S.
9. Trace conjunctival hyperemia and clear cornea on day three follow-up.
Treatment Plan Redefined
10. Resolving follicles and hyperemia of inferior palpebral conjunctiva O.D.
Incorporating betadine treatment for viral conjuncitivitis into our practice has been satisfying for both patient and practitioner. However, adjusting our treatment protocol to include topical NSAIDs both before and after treatment, oral pain medication on day one and non-preserved artificial tears to minimize corneal irritation has greatly improved patient comfort. With the fast resolution of ocular signs and symptoms and our ability to control for ocular discomfort post treatment, we do not hesitate to offer this very effective therapy.
11. Resolving follicles and hyperemia of inferior palpebral conjunctiva O.D.
The authors have no financial interest with any ophthalmic eye drops manufactures.
1. Gordon YJ. The evolution of antiviral therapy for external ocular viral infections over twenty-five years. Cornea. 2000 Sep;19(5):673-80.
2. Gregori NZ, Schiffman JC, Miller DM, Alfonso EC. Clinical trial of povidone-iodine (Betadine) versus placebo in the pretreatment of corneal ulcers. Cornea. 2006 Jun;25(5):558-63.
3. Isenberg SJ. The ocular application of povidone-iodine. Community Eye Health 2003;16:30-1.
4. Isenberg SJ, Apt L, Valenton M, et al. A controlled trial of povidone-iodine to treat infectious conjunctivitis in children. Am J Ophthalmol. 2002 Nov;134(5):681-8.
5. Pelletier JS, Stewart K, Trattler W, et al. A combination povidone-iodine 0.4%/dexamethasone 0.1% ophthalmic suspension in the treatment of adenoviral conjunctivitis. Adv Ther. 2009 Aug;26(8):776-83.
6. Goldberg D. Betadine for EKC Study. Available at: www.betadineforekc.com/the-study.aspx. (Accessed September 2010).
Dr. Wilmer is an Associate Clinical Professor and Director of Residency Programs at the University of California Berkeley, School of Optometry.
Dr. Hsieh completed her residency training at the University of California, Berkeley, School of Optometry in Primary Care and Low Vision. She currently works in the private practice sector in Campbell, Fremont and San Jose, Calif.


