Corneal collagen crosslinking (CXL) is the only minimally invasive surgical procedure to halt keratoconus progression, and is often considered the gold standard.1 While the Dresden protocol, known as “epi-off,” was FDA-approved for clinical use in the United States in 2016, the treatment option’s history traces back to the early 2000s. Today, a variety of newer protocols are under development with the hopes of reducing complications or improving outcomes from the standard epithelium-off protocol. The growing sense of intrigue has led to several US clinical trials investigating the alternative protocols already in use in other countries, as well as a spread of off-label uses.
 |
| CXL can stop progression of keratoconus and can also help to preserve vision. Photo: International Keratoconus Academy. Click image to enlarge. |
Reliability with Dresden
The Dresden protocol remains limited in scope, and only uses riboflavin solutions and an ultraviolet (UV) light system designed by Avedro. The current technique involves removing the epithelium and applying riboflavin solution (0.1% riboflavin in 20% dextran solution) to the de-epithelialized cornea 30 minutes before irradiating it with UVA at a wavelength of 370nm and power of 3mW/cm2 or 5.4J/cm2 for another 30 minutes.2 The riboflavin solution is applied to an 8mm area of the central cornea every three to five minutes during the irradiation process. The epithelial removal prior to CXL treatment addresses the epithelium’s shielding effect and ensures adequate penetration of riboflavin to the corneal stroma, while the riboflavin facilitates absorption of UVA and prevents UVA damage to the endothelium.3-5
Philadelphia’s Clark Chang, OD, of Wills Eye Hospital and TLC Vision, understands that the epi-off CXL procedure stands as the tried-and-true method. “It currently has a sufficient amount of scientific data behind it,” Dr. Chang says. “The efficacy of the procedure has been largely proven with good outcomes, and we continue to provide that treatment protocol in my practice to most of the patients coming in that seek crosslinking care.”
Cecelia Koetting, OD, of Virginia Eye Consultants, also believes that patients are seeing the benefits of the current protocol, even though payers might not cover it. “We have noticed some of our keratoconus patients have continued improvement in their visual acuity and corneal flattening well after one year from treatment,” Dr. Koetting says.
Still, the protocol’s reputation of complications precedes it. “The dextran-diluted riboflavin appears to cause significant dehydration, thus more occurrence of scars, melting, possible infection and delayed re-epithelialization,” explains A. John Kanellopoulos, MD, a clinical professor of ophthalmology at New York University Medical School and medical director of the Laservision Eye Institute in Athens, Greece.
S. Barry Eiden, OD, president and medical director at North Suburban Vision Consultants, Ltd., and president and co-founder of the International Keratoconus Academy (IKA), has seen patients who have undergone epi-off CXL experience significant discomfort for several days post-op associated with the epithelium removal, as well as slow recovery of vision, visual fluctuations over the initial weeks and months and a significant delay in the ability to wear contact lenses.
But patients can have great success following the epi-off protocol, as long as they are fully informed of the postoperative course, says Dr. Chang. “We do tell patients about the visual fluctuation that is present within the first three to six months, and that they can typically resume contact lens wear or fitting at about one month post-operatively,” Dr. Chang notes.
Gaining Speed
In an attempt to improve the visual and topographical outcomes of the standard CXL protocol and to minimize the time-related discomfort and endothelial-related side effects, researchers are investigating various modifications, such as a protocol known as accelerated CXL.1 This method uses shorter UVA exposure times of three, five or 10 minutes with higher energy levels of 30, 18 or 9mW/cm2—all of which provide a cumulative irradiation dose of 5.4J/cm2.1
“In addition to comfort and convenience, researchers have theorized that the shorter exposure time may reduce the rate of complications such as corneal thinning, haze, infection and melting,” explains Dr. Eiden.
The main advantage of the accelerated protocol in comparison with conventional CXL is the reduced treatment time. Theoretically, the infection risk might also be reduced since the de-epithelialized cornea is exposed for a shorter period of time.6
Although some contradictory clinical and laboratory results exist, many studies suggest accelerated CXL procedure as an effective method to stabilize the progression of keratoconus both in adults and in children.1
One study from the Sunderland Eye Infirmary in Great Britain found that the accelerated CXL protocol safely halted keratoconus progression over a 24-month period. The researchers observed that eyes with corrected distance visual acuity (CDVA) greater than or equal to 0.3logMAR significantly improved from 43 preoperatively to 50 (96.2%) eyes. They noted no adverse effects, as all cases of mild post-CXL corneal haze were transient and resolved by six months post-op after a course of topical steroids. The study proposes that early administration of CXL for progressive keratoconus leads to good long-term visual outcomes.7
More recently, pulsed-light accelerated crosslinking with eight minutes of UVA exposure at 30mW/cm2 with an energy dose of 7.2J/cm2 was introduced as an effective mode of treating keratoconus.8 A clinical study with a one-year follow-up found that the functional outcome of the pulsed-light accelerated CXL was better than the continuous-light accelerated CXL with the ability to penetrate deeper into the corneal stroma.9,10
Using a higher peripheral intensity profile allowed UV light to penetrate deeper into the periphery of the cornea during the accelerated procedure, increasing tissue crosslinking.11 While clinical studies indicate that accelerated CXL is successful in stabilizing keratoconus, several investigators have noted differences in the appearance and depth of the corneal stromal demarcation line that occurs when CXL is performed at different irradiances.12 Because surgical protocols for accelerated CXL are significantly different than the current one, researchers are unable to effectively compare the two.
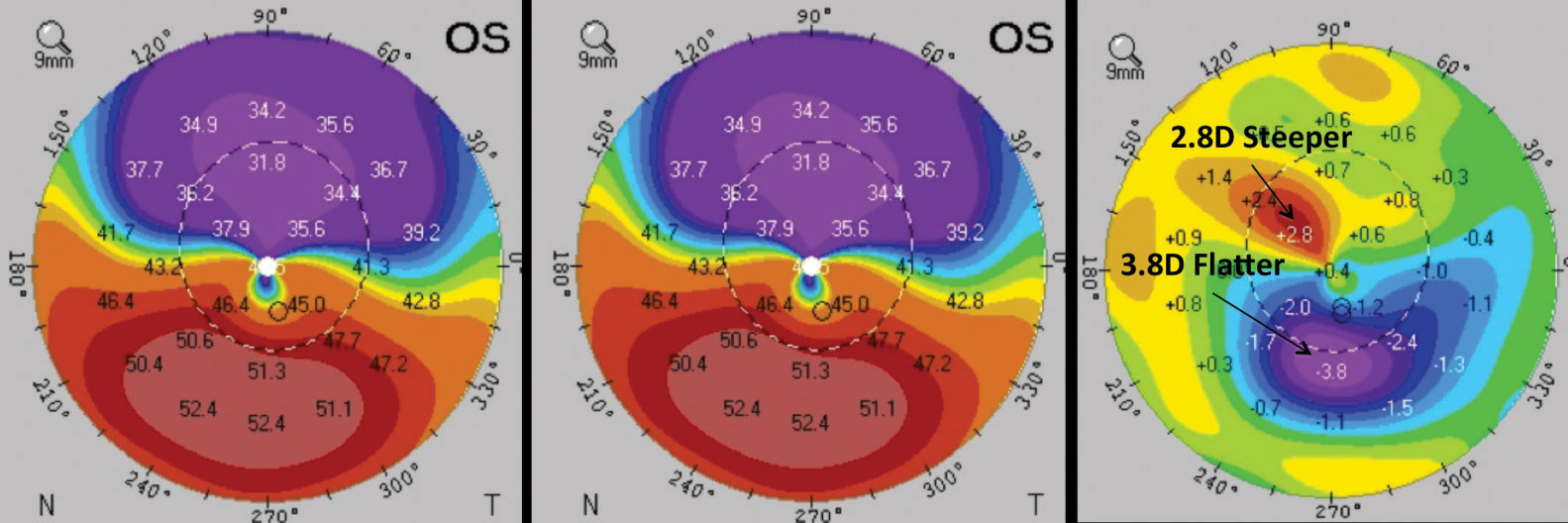 |
| This patient underwent epi-on CXL. Comparing the pre-op (left) and post-op (middle) corneal thickness reveals significant changes in corneal parameters in the difference map (right). Images: William Trattler, MD; International Keratoconus Academy. Click image to enlarge. |
Stick with the Epithelium
The clinical drawbacks of standard crosslinking—such as post-op pain, prolonged visual recovery due to the large epithelial defect and the inability to perform conventional CXL on thin corneas due to the risk of endothelial damage—has encouraged clinicians to look for a method of crosslinking without epithelial debridement.1 For transepithelial (epi-on) crosslinking, the corneal epithelium is left intact prior for the CXL treatment. One study notes that transepithelial CXL can be used as an effective treatment option for keratoconic patients with thin corneas.1
“Epi-on crosslinking has a number of potential advantages over epi-off, including a superior safety profile, faster recovery of vision and visual stability,” Dr. Eiden says, who uses the epi-on procedure in his practice. “It provides far less discomfort and the ability to return to normal life activities and contact lens wear in a much shorter period of time.”
Research demonstrates that preserving the epithelial layer conserves corneal morphology and makes the procedure more comfortable for patients.1 Performing CXL with an intact epithelium can reduce the risk of infective keratitis, improve patient comfort, reduce stromal haze and minimize intraoperative corneal thinning, likely due to less tissue damage and reduced wound healing reaction.13
However, epi-on CXL might affect corneal sensitivity to a lesser degree than the standard protocol. Riboflavin—a high molecular weight, hydrophilic molecule—may not penetrate the intact epithelium as well.14 An intact epithelium might also diminish oxygen diffusion into the stroma, further weakening the crosslinking effect.15
Currently, Avedro is recruiting practitioners for a Phase III study on the efficacy of the epi-on protocol, with a primary completion date of June 2020.16
While patient comfort is important to the treatment’s eventual adoption, its efficacy is even more crucial, and researchers continue to study whether epi-on is as effective as the standard protocol. Dr. Eiden thinks that might be a tall order. “The volume of evidence-based data supporting the efficacy of epi-off CXL exceeds that for epi-on CXL; however, over the years greater support for epi-on CXL efficacy has come to light,” Dr. Eiden says.
“Despite clinical debates regarding long-term efficacies of epithelium-on protocols, this area will continue to fascinate physicians within the United States,” says Dr. Chang. “Recent research effort to refine transepithelial protocols will result in better treatment standardization and reduce questions about its long-term efficacy.”
Staying Current
Other investigations are underway to explore the use of iontophoresis to help address some of the shortcomings of the epi-on protocol. This technique uses a low-voltage electrical current to increase the penetration of riboflavin deeper into the corneal layers during epi-on CXL. The iontophoresis method (I-CXL) of riboflavin loading typically takes only five minutes—far better than the 30 minutes necessary for the Dresden protocol.1 A study investigating human corneas following I-CXL and conventional CXL methods suggested that I-CXL induced less tissue damage and provided better stromal remodeling compared with conventional CXL treatment.1
Iontophoresis may provide other advantages as well. Studies show a significant improvement in contrast sensitivity in patients who underwent I-CXL compared with those who had conventional CXL.17,18 This may be due to the epithelial debridement and wound healing in standard CXL, according to the researchers. Also, early investigations suggest a reduction in postoperative pain and incidence of infective keratitis due to its transepithelial nature. However, long-term follow-ups are needed to establish its efficacy.19
 |
| Epi-on/accelerated/oxygen-enhanced CXL remains investigational, but it might be common in the future. Photos: Avedro, International Keratoconus Academy. Click image to enlarge. |
Reaping Refractive Benefits
“Once the efficacy question has been answered, then how do we maximize the refractive benefit from crosslinking?” Dr. Chang asks. While most keratoconus patients will continue to require contact lenses, these new CXL protocols may help to improve their vision when they aren’t wearing corrective lenses.
According to Dr. Kanellopoulos, refractive crosslinking involves the use of customized, variable-pattern, variable-fluence crosslinking to address refractive error based on topography. “This includes the concept of treating corneal irregularity with a higher refractive correction than standard crosslinking,” he says.
Dr. Kanellopoulos and his team have been working on a new CXL protocol that uses a customized pattern and variable fluences to deliver different energy crosslinking to enhance crosslinking’s refractive effect—known as the Athens protocol. According to Dr. Kanellopoulos, refractive crosslinking has been a buzzword outside the United States since he began his work on it in 2013. The Athens protocol offers the ability not only to halt keratoconus and ectasia evolution but also to have a more significant refractive rehabilitation for these patients.
This protocol combines crosslinking and a partial topography-guided photorefractive keratectomy (PRK), using 6mW for 15 minutes with the treatment and soak. The combined treatment lasts for about 22 minutes in total instead of more than an hour. Those following the protocol now use saline-diluted riboflavin instead of dextran-diluted riboflavin, which causes less corneal dehydration and less epithelial damage, according to Dr. Kanellopoulos.
“This treatment has been in use for the last decade now and has been in use by many clinicians globally, even if it is not labeled as Athens protocol,” Dr. Kanellopoulos says. “The combination of the partial customized ablation with higher fluence CXL appears to not only stabilize ectasia but dramatically improve visual rehabilitation in these patients. Thus, combining it with refractive crosslinking can offer an even more enhanced effect with less tissue removal.”
Another refractive crosslinking method, photorefractive intrastromal corneal collagen crosslinking (PiXL), applies high-energy UV light to specific areas of the cornea to modify refractive error. PiXL uses riboflavin of a significantly higher concentration than what is used in the Dresden protocol. In addition to its application as a method to address normal refractive errors, PiXL potentially can provide specific improvement in cases of irregular topography such as with keratoconus, according to Dr. Eiden. Customizing the energy application to specific areas of the cornea can reduce irregularity and improve visual performance, he said.
“If shown to be safe and effective, PiXL for the treatment of irregular corneas could be an exciting addition to our armamentarium,” Dr. Eiden says. “Without a doubt, any of our patients who have already suffered significant disease and corneal irregularity would welcome the opportunity to have their severity of disease reduced by a safe and effective treatment method.”
Clinical trials are currently underway in the United States to investigate PiXL’s ability to improve vision without compromising corneal biomechanical integrity.20 Researchers are also testing the efficacy of oxygen goggle use during the epi-on procedure to help boost the oxygen supply and, thus, treatment efficacy.21
Lingering Questions
One major drawback of the current CXL procedure isn’t directly involved with the protocol; rather, it is the lack of a standardized analysis of corneal biomechanics following the procedure. As it stands, only limited studies exist on the ultra-structural alterations of the crosslinked cornea, with a majority of studies focusing on the biomechanical properties following conventional CXL treatment.1 A detailed investigation into the fine morphological changes that occur following CXL is needed to further understand and evaluate the long-term effects of CXL.
Accurate corneal biomechanical measurements in the clinical environment remains a challenge today, as most practitioners make treatment decisions based on topographic and tomographic data.22 Corneal tomographers only provide morphologic information on curvature and elevation that can be used to assess disease severity and localization. Currently, no widely available clinical diagnostic tool can locate the region of biomechanical weakness in an individual patient. Therefore, abnormalities in the anterior corneal curvature and posterior corneal elevation observed on corneal tomography are used as a proxy to define the cone area.12
“We do not have a measurement of the actual corneal stability in relation to its effect on that individual eye,” Dr. Kanellopoulos points out. “So, we do not know the threshold we should respect and pursue with crosslinking, and then we get different amounts of stabilization with the procedure.” Some eyes have a significant flattening effect due to the crosslinking, while others unfortunately continue on to ectasia, Dr. Kanellopoulos says.
Dr. Kanellopoulos thinks better biomechanical measurements are key elements to first assess which eyes are at risk and how much crosslinking—and what type of CXL procedure—can provide biomechanical stability. “This value would be not only helpful for ectasia cases but for all refractive surgery cases that are based on a corneal procedure,” he says. Dr. Kanellopoulos believes the measurements could “weed out” patients who would be in danger of having ectasia or flag the post-LASIK or post-PRK cases that are in danger of ectasia, thus offering practitioners an ideal crosslinking stabilization option.
While tomography and topography are helpful, any potential biochemical measures will act as an adjunct in the near future, Dr. Chang says. Optometrists won’t stop relying on tomography; instead, future diagnostic tools will provide additional clinical metrics to help measure the need for crosslinking more accurately.
“In the foreseeable future, corneal biomechanical data will not completely replace the need for tomography, but it certainly would be something that can enhance the accuracy of our diagnoses and corneal monitoring,” Dr. Chang says. A better understanding of corneal cell biology prior to surgery could produce optimized laser ablation profiles and less inflammation, especially in crosslinked corneas, making an already safe and successful procedure produce better outcomes.23
Practitioners are also curious about the long-term effects of crosslinking on both the cornea and the disease progression—both of which are key for predicting patient outcomes. “Long-term data of progression of 15 to 20 years could allow for better prediction and anticipation of possible patients who may need to be re-treated or consider alternative treatment,” says Dr. Koetting.
As the discourse continues, many practitioners in the United States will continue to debate whether new crosslinking protocols can effectively handle the common complications of the Dresden protocol and usurp it as the gold standard. Although many short- and long-term studies have evaluated the effectiveness of these various crosslinking treatments, they provide contradictory results.1 While optometrists have yet to reach a consensus, many continue to follow the ongoing trends outside of the FDA-approved bubble, eagerly awaiting the next development abroad that may provide the best impact on keratoconus progression management.
1. Subasinghe SK, Ogbueh KC, Dias GJ. Current perspectives on corneal collagen crosslinking. Clin Exp Ophthalmol. 2018;256(8):1363-84. 2. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620-7. 3. Samaras K, Doutch J, Hayes S, et al. Effect of epithelial retention and removal on riboflavin absorption in porcine corneas. J Refract Surg. 2009;25(9):771-75. 4. Mooren P, Gobin L, Bostan N, et al. Evaluation of UVA cytotoxicity for human endothelium in an ex vivo corneal cross-linking experimental setting. J Refract Surg. 2016;32(1):41-6. 5. Wollensak G, Aurich H, Wirbelauer C, Sel S. Significance of the riboflavin film in corneal collagen crosslinking. J Cataract Refract Surg. 2010;36(1):114-20. 6. Kymionis GD, Kontadakis GA, Hashemi KK. Accelerated versus conventional corneal crosslinking for refractive instability: an update. Curr Opin Ophthalmol. 2017;28(4):343-7. 7. Ting DSJ, Rana-Rahman R, Chen Y, et al. Effectiveness and safety of accelerated (9mW/cm2) corneal collagen cross-linking for progressive keratoconus: a 24-month follow-up. Eye. January 4, 2019. [Epub ahead of print]. 8. Mazzotta C, Baiocchi S, Bagaglia SA, et al. Accelerated 15 mW pulsed-light crosslinking to treat progressive keratoconus: two-year clinical results. J Cataract Refract Surg. 2017;43(8):1081-8. 9. Mazzotta C, Traversi C, Paradiso AL, et al. Pulsed light accelerated crosslinking versus continuous light accelerated crosslinking: one-year results. J Ophthalmol. 2014;(3):604731. 10. Mazzotta C, Traversi C, Caragiuli S, Rechichi M. Pulsed vs continuous light accelerated corneal collagen crosslinking: in vivo qualitative investigation by confocal microscopy and corneal OCT. Eye. 2014;28(10):1179-83. 11. Herber R, Kunert KS, Veliká V, et al. Influence of the beam profile crosslinking setting on changes in corneal topography and tomography in progressive keratoconus: preliminary results. J Cataract Refract Surg. 2018;44(6):718-24. 12. Lytle G, Marshall J. Beyond the Dresden protocol: optimization of corneal crosslinking for visual function. In: Barbara A, ed. Controversies in the Management of Keratoconus. Cham, Switzerland: Springer Nature Switzerland AG; 2018:87-108. 13. Deshmukh R, Hafezi F, Kymionis GD, et al. Current concepts in crosslinking thin corneas. Indian J Ophthalmol. 2019;67(1):8-15. 14. Baiocchi S, Mazzotta C, Cerretani D, et al. Corneal crosslinking: riboflavin concentration in corneal stroma exposed with and without epithelium. J Cataract Refract Surg. 2009;35:893-9. 15. Hersh PS, Lai MJ, Gelles JD, Lesniak SP. Transepithelial corneal crosslinking for keratoconus. J Cataract Refract Surg. 2018;44:313-22. 16. Avedro. Study to evaluate the safety and efficacy of opi-on corneal crosslinking in eyes with progressive keratoconus. clinicaltrials.gov/ct2/show/NCT03442751. Updated February 15, 2019. Accessed February 15, 2019. 17. Lombardo M, Serrao S, Raffa P, et al. Novel technique of transepithelial corneal cross-linking using iontophoresis in progressive keratoconus. J Ophthalmol. 2016;2016:7472542. 18. Lombardo M, Giannini D, Lombardo G, Serrao S. Randomized controlled trial comparing transepithelial corneal crosslinking using iontophoresis with the Dresden protocol in progressive keratoconus. Ophthalmology. 2017;124:804-12. 19. Jia HZ, Peng XJ. Efficacy of iontophoresis-assisted epithelium-on corneal cross-linking for keratoconus. Int J Ophthalmol. 2018;11:687-94. 20. Avedro. Clinical trials & innovation. int.avedro.com/clinical-trials-innovation/. Accessed February 15, 2019. 21. Elling M, Kersten-Gomez I, Dick HB, et al. Photorefractive intrastromal corneal crosslinking for the treatment of myopic refractive errors: Six-month interim findings. J Cataract Refract Surg. 2017;43:789-95. 22. Samaniego CAR. Crosslinking playbook: future directions of CXL. Eyeworld. January 2019. 23. Hafezi, F. What’s hot and heating up in CXL. Cataract Refractive Surgery Today. 2018;November/December:86-90. |


