In November 2011, I was invited to the Global Contact Lens Care Summit to deliver a presentation on evidence and lens care in practice. It was the closing clinical presentation after two days of largely academic, rapid-fire conversations among a who’s who in contact lens research that included epidemiologists, microbiologists and representatives from administrative bodies, such as the FDA and standards organizations.
I was initially a bit apprehensive about
discussing my clinical impression that daily disposables represent the
future of most soft lens wear. As a clinician, I am fully aware of the
skepticism with which those who focus on scientific evidence regard
anecdotal observations. However, I have always supported my clinical
observations with good science—and as such, have kept a close eye on the
evidence as it has continued to expand and evolve over the years.
After all, sometimes clinical practice
guides the direction of research and, at other times, science drives
clinical practice. The two are synergistic in nature.
The Daily Disposable Plunge
Approximately 15 years ago, I made the decision to fit new soft lens
patients and refit symptomatic wearers into single-use disposable
lenses whenever possible. Based on personal clinical observations, I
found this modality to be the best, safest, most convenient and
trouble-free option available. In the following decade, our practice
supplied more than one million single-use lenses. Only rigid
gas-permeable (RGP) lenses can beat the safety record of one-day soft
contact lenses.1-4
  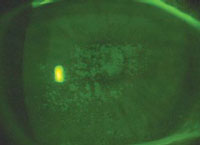 |
| Avoid, minimize or reduce these complications
(left to right, dry eye, giant papillary conjunctivitis, corneal
staining) with daily disposable lenses.
|
Keep in mind that this is not unexpected: When new technologies (such as single-use lenses) are launched, the patients who are more likely to be “risk-takers” are at the front of the line to try them.11,12 There may also have been some contaminating factors in this study, such as undisclosed overnight wear or re-use of daily disposables.
However, one important takeaway from the Dart study was that MK cases in daily disposable wearers seemed to be less severe than in other soft lens wearers. We should, however, not obsess over the very rare incidence of MK in single-use lens wearers.
Compliance and Lens Handling
Two of the last few barriers for enhanced contact lens safety are
compliance and lens handling. Researchers have personally communicated
to me that the natural tear film is relatively microbe-free, implying
that contact lenses (through lens care and handling) are the vehicle for
introducing pathogens or their endotoxins. Most of the time, the eye’s
amazing natural defenses, particularly the tear film, do an admirable
job of preventing infection.13,14
As eye care practitioners, we struggle with compliance. The facts are astonishing: One study found 98% of lens wearers were non-compliant in some aspect of lens wear and care.15-17 As we know, single-use lenses eliminate many steps in lens care, which alone is enough to improve compliance. In addition, daily disposables eliminate the need for the often contaminated lens cases, as well as allow us to sidestep the myriad heavily debated issues that surround multipurpose disinfecting solutions (e.g., infection, allergy, toxicity, incompatibility, inflammation, solution-induced corneal staining or preservative-associated transient hyperfluorescence, contact lens papillary conjunctivitis, and the like).18-20
Our last hurdle is to eliminate digital
contact, and the transfer of and contamination by microbes and
pollutants (such as moisturizers) from dirty fingers.
The Total Cost
After sitting through numerous conferences and lectures on the
topic, I keep coming back to the same conclusion: One-day lenses should
be our “go-to” choice in the majority of soft lens fittings,
piggybacking and problem-solving cases. Yet the majority of contact lens
prescribers in the US and worldwide don’t seem to understand that daily
disposables are best.
I often hear cost mentioned as a
deterrence. I respond by saying that daily disposables cost the
equivalent (or less!) than a cup of coffee per day. Nathan Efron,
BScOptom, PhD, DSc, compared spherical daily disposables to other
planned replacement disposables and found that the costs break even at
five days of use per week.21 In other words, two cups of coffee per week would cover the difference.
Now, factor in the total cost of ownership. If a regular disposable wearer has just one unscheduled visit every year or two, or an infection needing expensive eye drops or ophthalmological care, then suddenly the finances favor daily disposable lenses. In my experience, one-day lenses require less chair time and aftercare, fewer unscheduled visits and less time spent instructing patients on how to use disinfecting solutions. In addition, we see fewer complications such as red eye, dry eye, allergy, infiltrates, solution reactions, comfort problems and infections.
When comparing price, it is important for
eye care practitioners to remind patients to consider the full cost of
lenses and solutions. Often patients fail to add the cost of solutions
that they may purchase elsewhere into their running tally.
Remember, addressing objections is a minor but a pivotal part of the philosophical switch to daily disposables. Cost is only a problem when the perceived value doesn’t align with the price. Try shifting the focus from cost to benefits, such as convenience and comfort. With fresh lenses, patients no longer have to worry about uncomfortable denatured protein or lipid build-up.
International Trends
In the US, we are starting to see the transition of daily
disposables into the primary modality of choice; both the US and Canada
have increased from single to double-digit percentages over the past few
years.22
This trend seems to be continuing
worldwide. In Australasia, daily disposable lens prescribing is now
between 20% and 40%, with ever-increasing levels in some Asian regions,
such as Hong Kong and Taiwan. Japan and some European nations (including
Norway, Denmark, Italy and the United Kingdom) already have high levels
of single-use prescribing, within the 40% to 60% range.
However, some of their immediate neighbors (e.g., The Netherlands at 8%) are reporting lower percentages of 5% to 20%, similar to the US and Canada.22 These low numbers can be attributed to many factors, such as affluence, a high rate of RGP lens prescribing (The Netherlands has among the highest in the world), clinical training and the educator’s philosophy.
We already cover the bulk of the
refractive bell curve in daily disposables, with an ever-widening range
of astigmatic corrections. We have low surface friction lenses, low
modulus, moisture-retaining and lubricating options, and an increasing
number of high-Dk hydrogel and silicone hydrogels (SiHy). New
myopia-controlling and multifocal daily contact lenses have recently
appeared on the market, as well as flat-packs, a gradient-water SiHy and
a novel 78% water hydrogel with a lipo-mimetic surface, UV block and
aspheric optics. Antimicrobial surfaces, enhanced materials and unique
packaging strategies are likely to be seen in the not-too-distant
future.
Isn’t it time that you consider switching
your patients to daily disposables? The evidence almost unanimously
tells me that it’s the right thing to do.
Editorial assistance provided by BioScience Communications.
Dr. Saks is a third-generation optometrist and has served multiple terms as president of the Contact Lens Societies of South Africa & New Zealand. He has served as examiner in contact lenses and clinical optometry, lectures worldwide, participates in workshops and arranged conferences, and has served on the editorial boards for The South African Optometrist and International Contact Lens Clinic and as a referee for Clinical and Experimental Optometry.
1. Nagachandrika T, Kumar U, Dumpati S,
et al. Prevalence of contact lens related complications in a tertiary
eye center in India. Cont Lens Anterior Eye. 2011 Dec;34(6):266-8.
2. Cavanagh HD, Ladage P, Yamamoto K, et al. Effects of daily and
overnight wear of hyper-oxygen transmissible rigid and silicone hydrogel
lenses on bacterial binding to the corneal epithelium: 13-month
clinical trials. Eye Contact Lenses. 2003 Jan;29(1 Suppl):S14-6.
3. Efron N, Morgan PB, Hill EA, et al. The size, location, and
clinical severity of corneal infiltrative events associated with contact
lens wear. Optom Vis Sci. 2005 Jun;82(6):519-27.
4. Stapleton F, Keay L, Edwards K, et al. The incidence of contact
lens-related microbial keratitis in Australia. Ophthalmology. 2008
Oct;115(10):1655-62.
5. Solomon OD, Freeman MI, Boshnick EL, et al. A 3-year prospective
study of the clinical performance of daily disposable contact lenses
compared with frequent replacement and conventional daily wear contact
lenses. CLAO J. 1996;22:250-257.
6. Walline JJ, Long S, Zadnik K. Daily disposable contact lens wear in myopic children. Optom Vis Sci. 2004 Apr;81(4):255-9.
7. Brujic M. Daily disposable advantages and options. CL Spectrum. 2008 Feb.
www.clspectrum.com/articleviewer.aspx?articleID=101565 Accessed on July 9, 2012.
8. Efron N, Morgan PB, Woods CA, The international Contact Lens
Prescribing Survey Consortium. International survey of contact lens
prescribing for extended wear. Optom Vis Sci. 2012 Feb;89(2):122-9.
9. Dumbleton K, Woods C, Jones L, et al. Patient and practitioner
compliance with silicone hydrogel and daily disposable lens replacement
in the United States. Eye Contact Lens. 2009 Jul;4:164-71.
10. Dart JK, Radford CF, Minassian D, et al. Risk factors for
microbial keratitis with contemporary contact lenses: a case-control
study. Ophthalmology. 2008 Oct;115(10):1647-54.
11. Willcox MD, Carnt N, Diec J, et al. Contact lens case
contamination during daily wear of silicone hydrogels. Optom Vis Sci.
2010 Jul;87(7):456-64.
12. Keay L, Radford C, Dart JK, et al. Perspective on 15 years of
research: reduced risk of microbial keratitis with frequent-replacement
contact lenses. Eye Contact Lens. 2007 Jul;33(4):167-8.
13. Flanagan JL, Willcox MD. Role of lactoferrin in the tear film. Biochimie. 2009 Jan;91(1):35-43.
14. Morgan P, Dobson C. Tear film proteins and soft contact lenses. Optician. 2009 Jun:26-8.
15. Sokol JL, Mier MG, Bloom S, et al. A study of patient compliance
in a contact lens-wearing population. CLAO J. 1990
Jul-Sep;16(3):209-13.
16. Carnt N, Keay L, Willcox M, et al. Higher risk taking propensity
of contact lens wearers is associated with less compliance. Cont Lens
Anterior Eye. 2011 Oct;34(5):202-6.
17. Robertson D, Cavanagh HD. Non-compliance with contact lens wear
and care practices: a comparative analysis. Optom Vis Sci. 2011
Dec;88(12):1402-8.
18. Carnt N, Jalbert I, Stretton S, et al. Solution toxicity in soft
contact lens daily wear is associated with corneal inflammation. Optom
Vis Sci. 2007 Apr;84(4):309-15.
19. Bright FV, Maziarz P, Liu M, et al. PHMB and PQ-1 impact on a
liposome corneal surface membrane model. Invest Ophthalmol Vis Sci.
2011;52:e-abstract.
20. Efron N. Contact Lens Complications. 3rd ed. Elsevier Health Sciences; 2012.
21. Efron N, Efron SE, Morgan PB, et al. A ‘cost-per-wear’ model
based on contact lens replacement frequency. Clin Exp Optom. 2010
Jul;93(4):253-60.
22. Morgan PB, Woods CA, Tranoudis IG, et al. International contact lens prescribing in 2011. CL Spectrum. 2012 Jan;27:26-32.