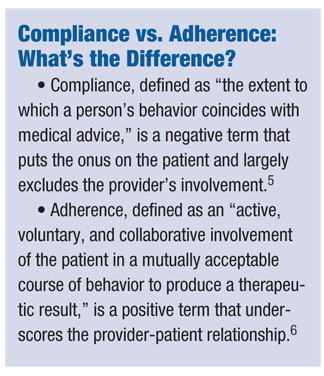
Compliance, defined as “the extent to which a person’s behavior coincides with medical advice,” suggests that it is a patient characteristic only and does not account for the provider’s potential role in non-compliance.4,5 Moreover, a patient who fails to comply with a provider’s instructions is often deemed uncooperative.3
In contrast to compliance, adherence has been defined as an “active, voluntary and collaborative involvement of the patient in a mutually acceptable course of behavior to produce a therapeutic result.”6
 Thus, using the term “adherence” underscores the importance of the provider-patient relationship and patient-centered focus to care by suggesting both patients and providers are involved in the process of establishing and following a patient’s treatment regimen.
Thus, using the term “adherence” underscores the importance of the provider-patient relationship and patient-centered focus to care by suggesting both patients and providers are involved in the process of establishing and following a patient’s treatment regimen.
This relationship is critical, as it sets the stage for accurately assessing and addressing adherence issues through honest, empathic communication between the provider and patient, such as discussions regarding patient-reported barriers to implementation of the care regimen.7,8
This article reviews the literature on adherence to contact lens care regimens, provides recommendations for future research and discusses implications for clinical practice from a patient-centered focus.
Characteristics of Non-Adherence
In contact lens care research, non-adherence rates typically have been reported to range from as low as 40% to as high as 91%.1,9,10 These rates are comparable to, or higher than, other areas of adherence research, such as asthma and diabetes.11-13 The high variability in rates of adherence suggests that patient non-adherence is influenced by a variety of factors. Studies have found that although most patients are able to demonstrate knowledge of their treatment plan, few realize that they are not adherent.14
Furthermore, adherence to contact lens care regimens may be complicated by the preventive nature of the treatment. Specifically, adherence to preventive treatments tends to be less reinforcing, as there often is no direct effect (e.g., decrease in symptoms) from following the treatment. So, patients may not perceive the treatment to be effective or necessary and are less likely to follow the prescribed regimen. Results from past studies corroborate the idea that adherence to preventive care is problematic; for example, one study found that asthma patients are less adherent to the proactive components of their treatment regimens.15 While there is no singular component that is of primary concern, common areas of non-adherence to contact lens care include hand hygiene, rinsing and disinfecting contact lenses, wear time and replacement time.1,10
Finally, it is important to measure whether patients are following their contact lens care regimen, and doing so correctly. Two ways of measuring adherence in contact lens wearers are direct methods (e.g., microbiological assays, home spot checks) and indirect methods (e.g., surveys, demonstration of cleaning).1 While direct methods may provide a more objective assessment, they are impractical and expensive.
 Many physicians rely on indirect methods to assess adherence. However, the indirect methods are often problematic because the constructs that are measured (e.g., knowledge) may not be accurate indicators of adherence behavior and self-reporting measures may be biased by outside factors (e.g., social desirability, or a tendency to want to please the health care provider by reporting adherence).
Many physicians rely on indirect methods to assess adherence. However, the indirect methods are often problematic because the constructs that are measured (e.g., knowledge) may not be accurate indicators of adherence behavior and self-reporting measures may be biased by outside factors (e.g., social desirability, or a tendency to want to please the health care provider by reporting adherence).
Non-adherence Factors
While it is important to know what non-adherence looks like and how it is measured, most researchers also are interested in what factors contribute to this problem, and how non-adherence can be addressed.
Review studies have found that many factors are associated with neglect in contact lens care.1,10 One factor associated with non-adherence is insufficient knowledge. While many patients believe they are following their treatments, most did not fully understand all of the components of their lens care and, as a consequence, were non-adherent.1,2,9,14
Also, patients who have less education or lower income, have worn contacts for a longer period of time, have briefer lens replacement times, or wear contacts for cosmetic reasons have been found to have increased rates of non-adherence.10
Finally, the health-belief model has been applied to this area; this model postulates that adherence to a treatment regimen is due to an interaction of factors, including perceived severity of illness, health benefits of adherence and patient motivation.16 One study found that the health-belief model accounted for approximately 32% of the variance in adherence to contact lens care regimens in adolescents and adults who wore contacts for at least two years.17
Unfortunately, the identification of all aforementioned factors stems from a small body of research. More in-depth studies should be conducted to increase our understanding of what exactly contributes to non-adherence to contact lens care regimens in order to better focus interventions aimed to improve non-adherence.
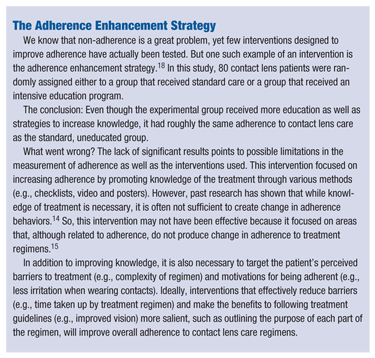
While there have been many suggestions to alleviate the problem of non-adherence, few interventions have been studied to determine whether they effectively improve this problem behavior. (See “The Adherence Enhancement Strategy,” above.)
 Clinical Practice Implications
Clinical Practice Implications
Overall, non-adherence to contact lens care regimens remains a significant problem, and research has demonstrated few effective methods for enhancing adherence in contact lens wearers. However, research in other health populations provides some evidence-based directions for clinical practice and future research to address non-adherence among contact lens wearers.
First, prior to enhancing patient non-adherence, ensure that non-adherence is accurately assessed. Due to the impracticality of direct measurements, indirect measurements such as self-report questionnaires or interviews often are used to assess adherence, despite research concluding that these methods tend to produce inaccurate estimates of adherence rates among other medical populations. 2,4,9,18,19 In addition, several studies have used the demonstration of contact lens cleaning to measure adherence to contact lens care regimens; but, demonstration of cleaning techniques may only assess patient knowledge of the regimen and not actual adherence.9,18,19
Current methods used to evaluate adherence to contact lens care regimens may provide inaccurate measurements due to a variety of issues, including social desirability bias associated with self-report measures, assessment of regimen knowledge rather than adherence behavior per se, and “white coat” adherence (i.e., increasing adherence to a regimen prior to a clinic appointment).
So, we should consider using a more objective, indirect method of assessing adherence to contact lens care regimens—much the way that pharmacy refill data has been found to provide a more adequate estimate of adherence rates among other health populations (e.g., youth with cystic fibrosis).20
Additionally, the quality of the provider-patient relationship and the provider’s communication style are important factors to consider in the assessment and management of non-adherence issues. Much research has demonstrated that patient adherence is higher with physicians who communicate well.8,21 When physicians undergo training in effective communication skills, their patients display greater adherence than patients of physicians who did not receive training.8
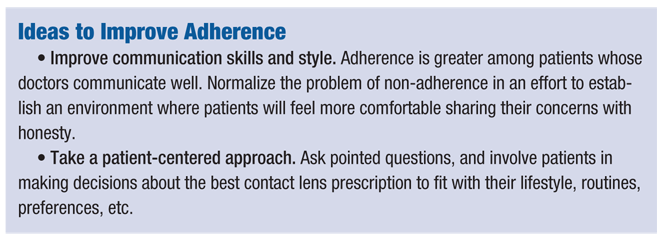 In addition to advocating the importance of effective communication between provider and patient, another strategy is using a patient-centered approach that focuses on patient perceptions of the physician’s advice and involves the patient and family in decision-making about treatment plans.7 Such an approach allows the patient to have more control over his or her own treatment regimen and may improve the patient’s adherence.
In addition to advocating the importance of effective communication between provider and patient, another strategy is using a patient-centered approach that focuses on patient perceptions of the physician’s advice and involves the patient and family in decision-making about treatment plans.7 Such an approach allows the patient to have more control over his or her own treatment regimen and may improve the patient’s adherence.
More specifically, providers can phrase questions about adherence in a manner that normalizes the issue for patients in an attempt to elicit more honest and accurate information regarding their patients’ adherence. For example, providers can explain that they do not expect their patients to be perfectly adherent with their contact lens care because many individuals with contact lenses forget to clean them once and a while.
Providers also can take the needs of individual patients into account when prescribing contact lenses (e.g., prescribe monthly disposable lenses to a patient who has difficulty remembering to remove their lenses each night). Taking this approach, a provider might say the following to a patient: “Many people find it difficult to follow standard procedures in caring for and wearing their contact lens. Some of these difficulties may be due to time and hassle, or perhaps financial costs that are hard to afford. I want to be able to prescribe contact lenses that fit with your needs and concerns. What might be some concerns you could have in following your contact lens care routine?”
Based on such research, eye care practitioners should consider undergoing training in communication skills and taking a patient-centered approach to addressing adherence issues for their contact lens patients.
By taking a patient-centered approach to care and implementing some of these suggestions into your practice, you may be able to enhance adherence among your contact lens patients.
Dr. Duncan is an associate professor of psychology at West Virginia University and coordinator of the clinical child psychology doctoral program. Possessing a PhD in clinical psychology, her areas of research expertise include pediatric psychology, adherence to pediatric medical regimens, and the transition from pediatric to adult health care. She has garnered funding for her research at the local, national and federal levels.
Dr. Duncan's co-authors, Ms. Szabo and Mr. Enlow, are both graduate students in the Clinical Child Psychology doctoral program at West Virginia University in Morgantown, W.Va.
1. Claydon BE, Efron N. Non-compliance in contact lens wear. Ophthalmic Physiol Opt. 1994 Oct;14(4):356-64.
2. Bui TH, Cavanagh HD, Robertson DM. Patient compliance during contact lens wear: perceptions, awareness, and behavior. Eye Contact Lens. 2010;36:334-339.
3. Luftey KE, Wishner WJ. Beyond “compliance” is “adherence.” Diabetes Care. 1999;22:635-638.
4. Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331-342.
5. Haynes RB, Taylor DW, Sackett DL. Compliance in health care. Baltimore, MD: Johns Hopkins University Press; 1979.
6. Meichenbaum D, Turk DC. Facilitating Treatment Adherence: A Practitioner's Guide-book. New York, NY: Plenum Press; 1987.
7. Donovan JL. Patient decision making: the missing ingredient in compliance research. Int J Technol Assess Health Care. 1995;11:443-455.
8. Zolnierek KBH, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826-834.
9. Collins MJ, Carney LG. Compliance with care and maintenance procedures amongst contact lens wearers. Clin Exp Optom. 1986;69:174-177.
10. Donshik PC, Ehlers WH, Anderson LD, Suchecki JK. Strategies to better engage, educate, and empower patient compliance and safe lens wear: compliance: what we know, what we do not know, and what we need to know. Eye Contact Lens. 2007;33:430-433.
11. Cramer, JA. Systematic review of adherence with medications for diabetes. Diab. Care. 2004;27;1218-1224
12. Drotar D, Bonner MS. Influences on adherence to pediatric asthma treatment: a review of correlates and predictors. J Dev Behav Pediatr. 2009 Dec;30(6):574-82.
13. Schoenthaler AM, Schwartz BS, Wood C, Stewart WF. Patient and physician factors associated with adherence to diabetes medications. The Diab Educ. 2012;38;397-408.
14. Robertson, DM, Cavanagh, HD. Non-compliance with contact lens wear and care practices: A comparative analysis. Optom Vision Sci. 2011;88;1402-1408.
15. Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way? J Ped Psych. 2006;31;846-858.
16. Janz NK, Becker MH. The health belief model: a decade later. Health Edu Quart. 1984;11;1-47.
17. Phillips LJ, Prevade, SL. Replacement and care compliance in a planned replacement contact lens program. J American Optom Assoc. 1993;64;201-205.
18. Claydon BE, Efron N, Woods C. A prospective study of the effect of education on non-compliant behaviour in contact lens wear. Ophthalmic Physiol Opt. 1997 Mar;17(2):137-46.
19. O’Donnell C, Efron N. Non-compliance with lens care and maintenance in diabetic contact lens wearers. Ophthalmic Physiol Opt. 2004 Nov;24(6):504-10.
20. Modi AC, Lim CS, Yu N, et al. A multi-method assessment of treatment adherence for children with cystic fibrosis. J Cyst Fibros. 2006 Aug;5(3):177-85.
21. Nobile C, Drotar D. Research on the quality of parent-provider communication in pediatric care: implications and recommendations. J Dev Behav Pediatr. 2003 Aug;24(4):279-90.


