Phototherapeutic keratectomy (PTK) requires the use of a 193nm excimer laser to treat superficial corneal lesions. This type of photoablation provides a minimally invasive approach to removing lesions while ablating less than 20% of the corneal tissue. The goal is to improve the corneal clarity, enhance visual quality and reduce future corneal sequalae.1
As the world of eye care continues to grow, so are the types of surgical procedures. PTK first gained FDA approval back in 1995. Prior to the laser, a deep anterior lamellar keratoplasty was a first surgical consideration over a penetrating keratoplasty (PKP) for anterior corneal diseases. This procedure involves replacing the patient’s cornea down to Descemet’s membrane. However, normal endothelial function is required, otherwise a PKP is necessary to prevent corneal decompensation. Even then, a PKP carries its own list of complications and an average lifespan of 15 years.2
PTK offers patients a less invasive alternative to keratoplasties. An added advantage includes earlier recovery times and the ability to repeat the procedure in the case of recurrence. Studies observing the long-term efficacy of PTK have found that most recurrences take place, on average, within the first year, and 14% to 36% of patients who had a PTK required a second PTK.1,3,4 Mitomycin-C, an antifibrotic agent, can be used intraoperatively to reduce recurrence and minimize postoperative scarring.5
This procedure can be used in tandem with superficial keratectomy (SK), which is the manual dissection of the corneal epithelium without disrupting Bowman’s layer and using a surgical blade or diamond burr. Elevated opacities, like Salzmann’s nodular degeneration, respond well to this mechanical technique with the excimer laser to polish the underlying stroma.
Common Indications
PTK is suitable for patients with corneal pathologies within the anterior third of the cornea. The most common pathologies that require treatment with PTK involve stromal lesions, elevated epithelial lesions or recurrent corneal erosions.5 In our practice, patients commonly undergo PTK due to visually significant epithelial basement membrane dystrophy (EBMD) or recurrent corneal erosions.
 |
|
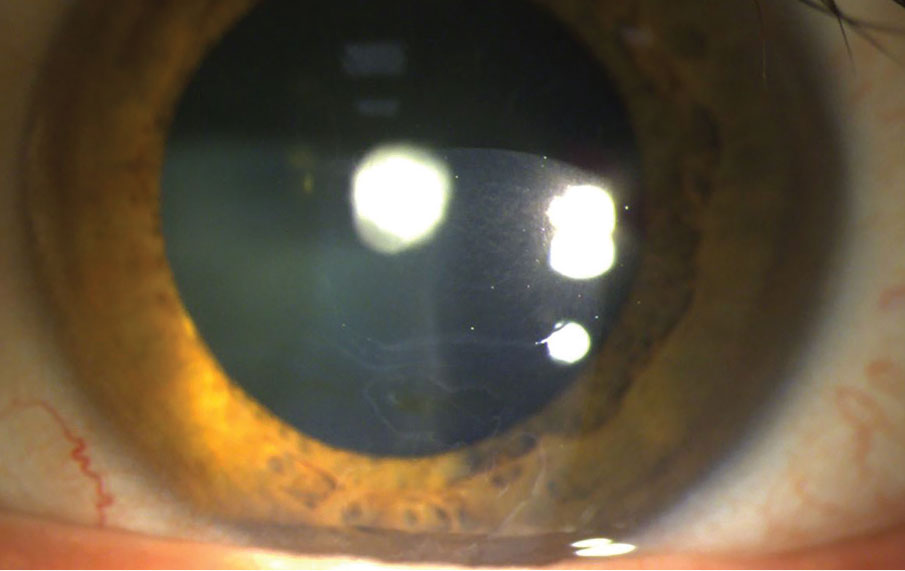
Fig. 1. Slit lamp photo of a patient with EBMD OS and a history of multiple RCEs. Patient is scheduled to undergo PTK surgery OS. A polar cataract is also captured in this photo. Click image to enlarge. |
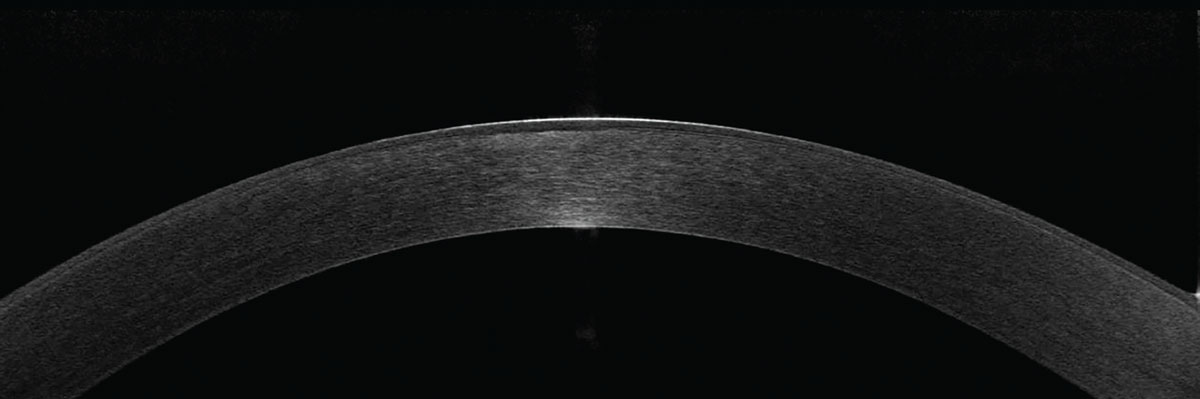
To assess whether a patient is a good candidate for PTK, a slit lamp examination is required, although an anterior segment OCT can be an even more powerful tool. Opacities and lesions are often clearly visible and can aid in quantifying the depth of the lesion. This is especially helpful in cases of depressed corneal scars.
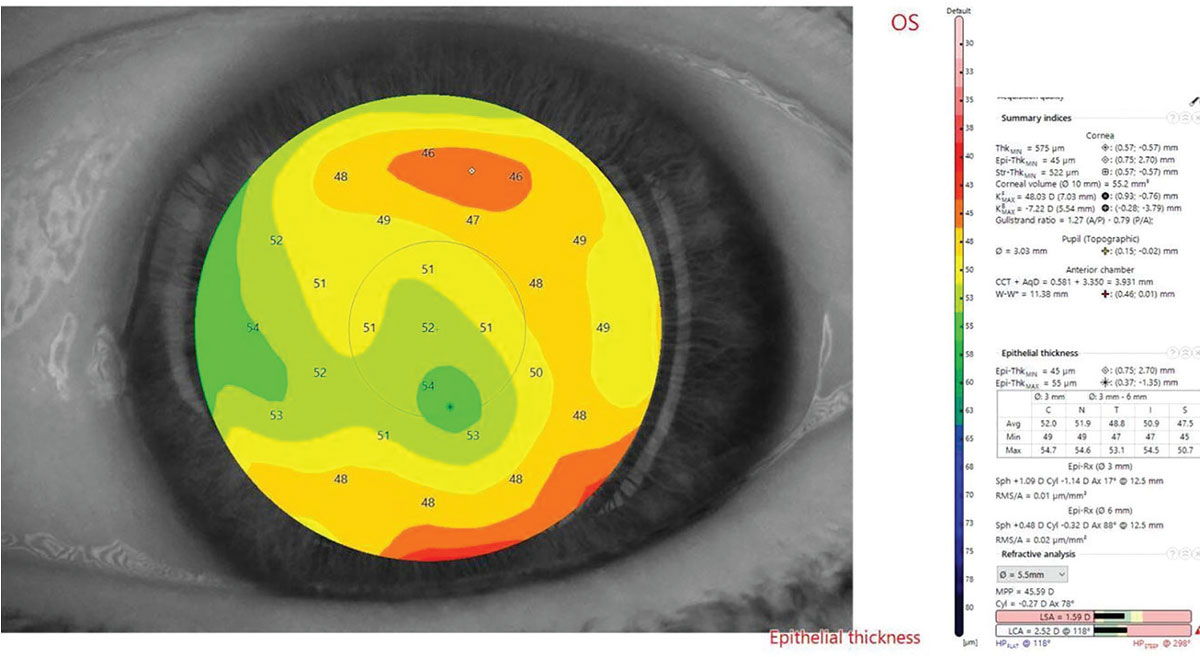
If corneal topography is available, this can also map out the cornea anteriorly. Patients are more likely to be visually symptomatic if the corneal pathology is within the central 5mm zone. If your practice has epithelial thickness mapping, this can enhance the predictability of healing post-PTK and highlight how the epithelium will respond to corneal pathologies.
Elevated Lesions
Salzmann’s nodular degeneration is a corneal disease that responds well to a combination of PTK and SK. Often, patients with these nodules remain asymptomatic and can be monitored. However, it can create irregular astigmatism and/or discomfort if the nodules increase in size. Since these elevated lesions are anterior to Bowman’s layer, SK alone can be enough to leave a smooth underlying surface. If irregularities remain underneath, then the excimer laser can help polish the underlying stroma.
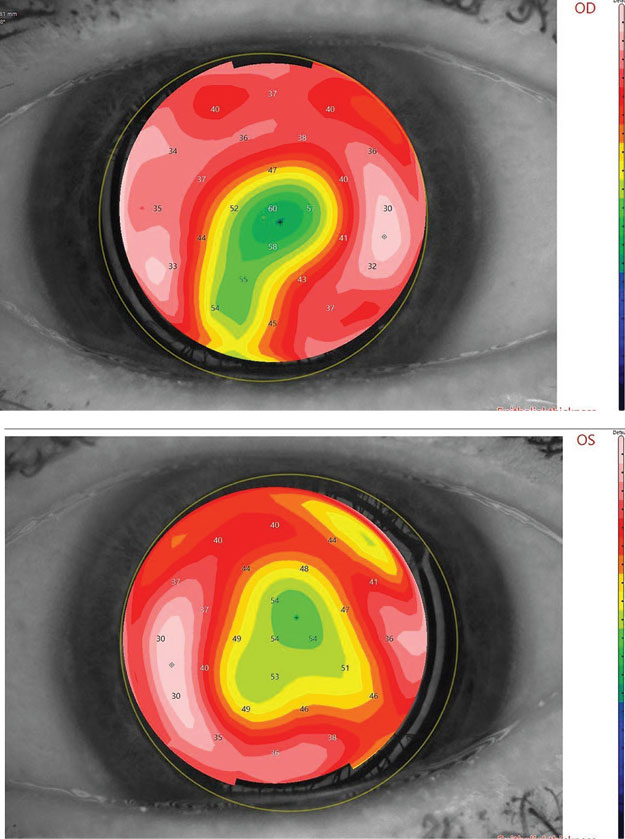 |
|
Fig. 2. Shown here is an epithelial thickness map of a patient with significant EBMD located centrally. An average epithelial thickness is 50µm. Differences greater than 5µm are considered abnormal. Click image to enlarge. |
EBMD and Recurrent Corneal Erosions
Among the corneal dystrophies, EBMD is the most common anterior dystrophy.6 It is characterized by an irregular epithelial appearance due to thickening of the basement membrane and weakened hemidesmosomes. This can lead to corneal erosions or be visually significant, depending on its severity. Based on the location of the EBMD, patients may be uncorrectable to 20/20 or have visual complaints. In these cases, a rigid gas permeable (RGP) over-refraction is an underused tool for determining whether the cornea is the source of visual complaints. If the patient displays subjective improvement, this can be the best evidence in support of proceeding with a PTK.
Patients with a history of corneal abrasion or trauma are also more susceptible to an RCE. As optometrists, we can manage this conservatively with a punctal occlusion, artificial tears, gel or ointment and a bandage contact lens (BCL). Loose epithelium can also be debrided behind the slit lamp. However, these conservative treatments often have a higher recurrence rate and lead to multiple visits for the patient.7 Due to the reduced recurrence rate with PTK, this can be a great first-line option to manage patients.
Stromal Lesions
Other anterior corneal dystrophies include Reis-Bücklers, granular dystrophy and lattice dystrophy. If they are visually significant, they can also respond well to PTK.
In cases where PTK is intended for spot treatment, there is a risk for unintended refractive changes. For central lesions, excessive localized laser treatment can induce a hyperopic shift because of a central flattening effect. In comparison, peripheral lesions may result in central steepening and induce an unintended myopic shift. Generally, PTK is considered a refractive neutral procedure due to the minimal surface ablation involved.
Corneal Scars
Rarely will a scar respond well to the excimer laser. Again, an anterior segment OCT is best for determining the depth of the scar. To minimize hyperopic shifts and stromal haze, depressed scars should not encompass more than 20% depth of the corneal tissue. Otherwise, you are running a high risk for stromal haze.
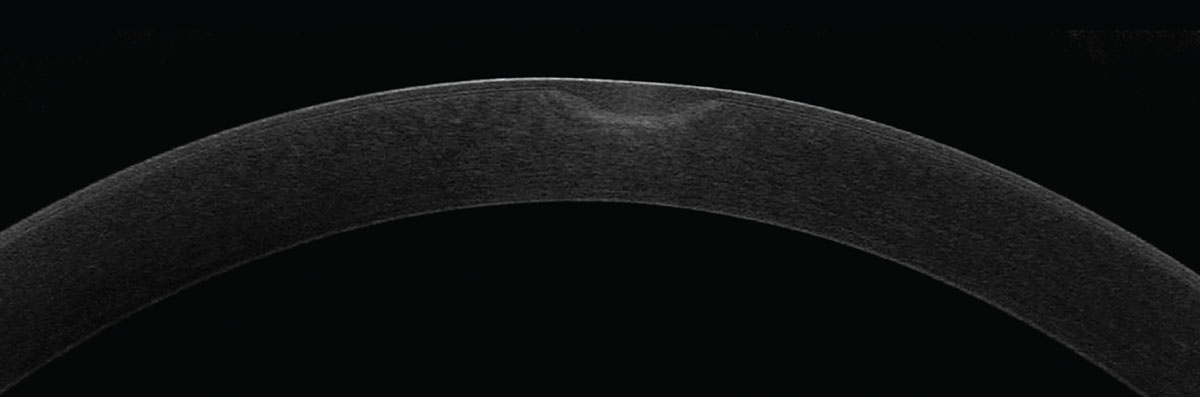 |
|
Fig. 3. Here is an example of a depressed corneal scar nearly missing the visual axis. This patient had complaints of visual disturbances but was not a good candidate for PTK due to the depth of the scarring. Click image to enlarge. |
Case A. PTK on a Superficial Scar
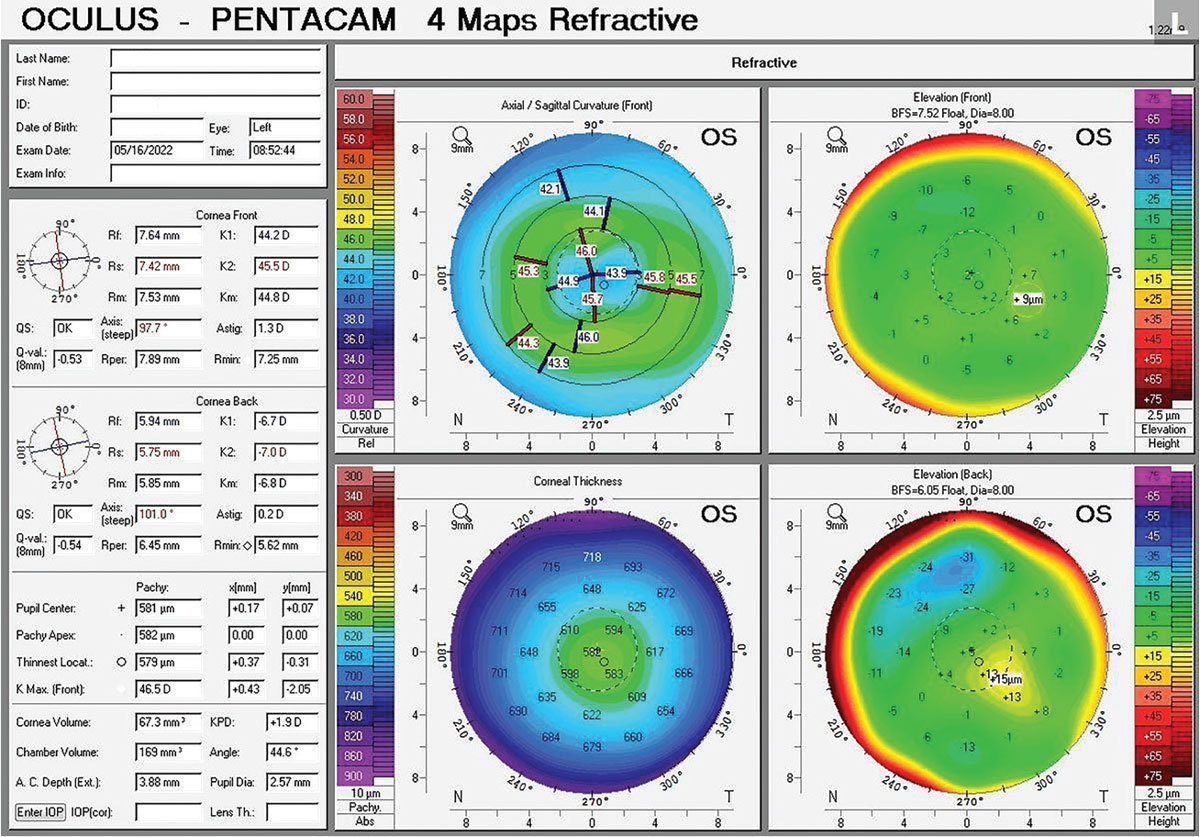 |
|
Fig. 4. Pentacam of patient from Case A with a history of a corneal ulcer infection OS resulting in a central corneal scar. The depressed corneal scar can be appreciated with the axial curvature map. Click image to enlarge. |
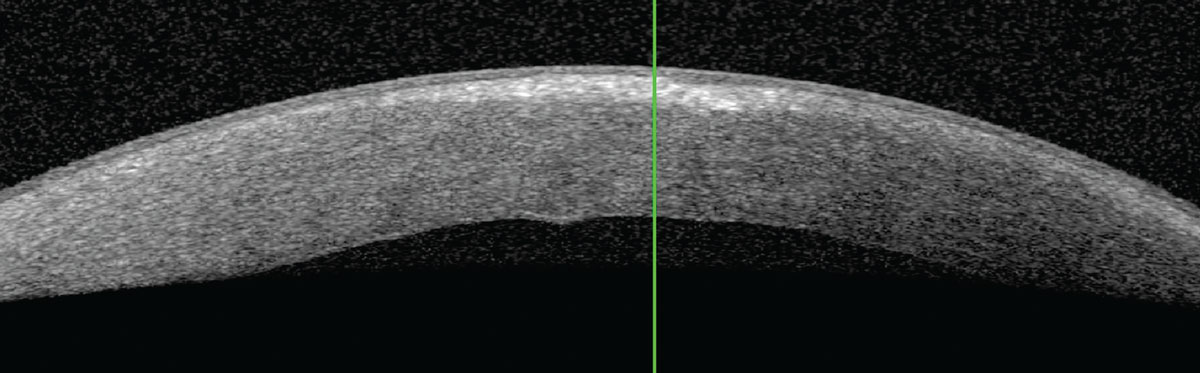
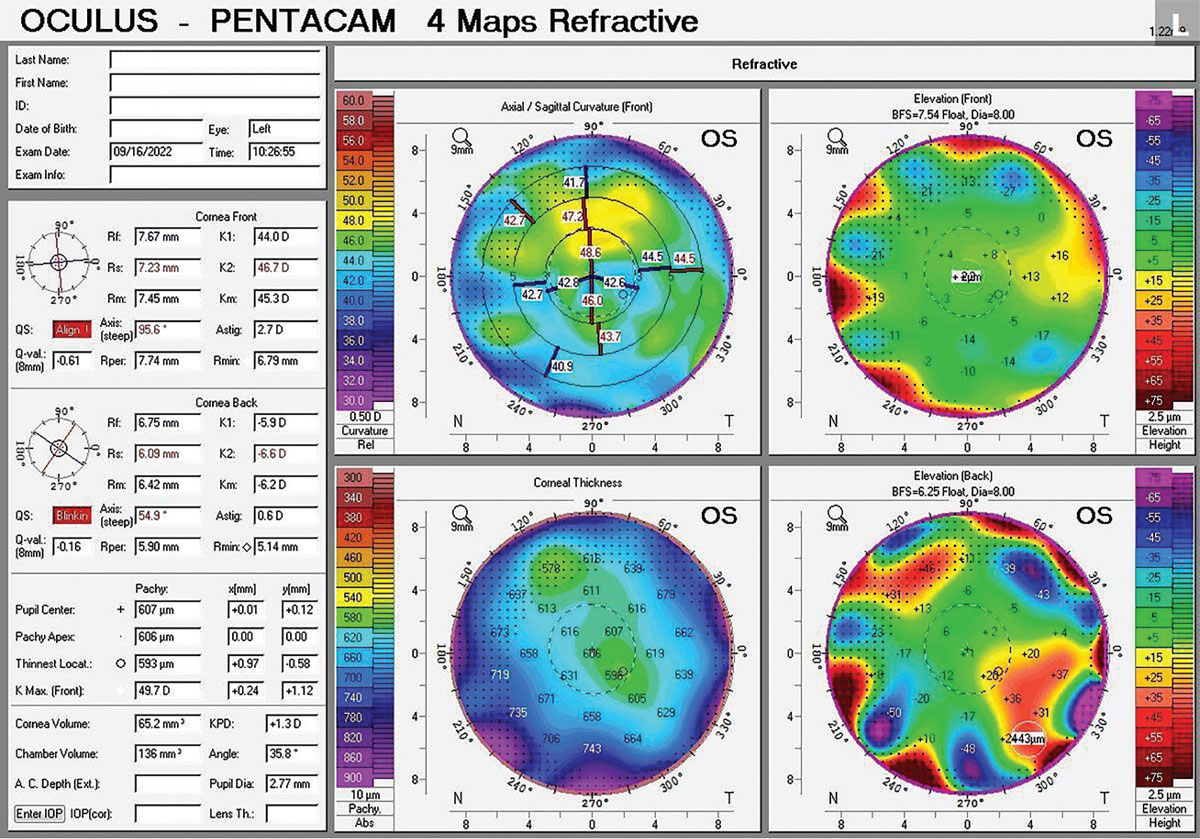
A 70-year-old female presented for a cataract evaluation. BCVA was 20/25 OD and 20/30 OS. Slit lamp examination revealed a mild cataract OD and OS with a central 2mm depressed corneal scar OS. The patient was educated on a guarded visual prognosis following cataract surgery due to the central scar in her left eye (Figs. 4 & 5). After further diagnostic testing, the patient was determined to be a candidate for PTK (Fig. 6). Based on the superficial nature of the scar, the patient elected to proceed with PTK prior to cataract surgery to attempt improvement of her visual potential. After the cornea heals, the patient will proceed with a small-aperture (IC-8; AcuFocus) IOL OS to reduce corneal aberrations.
PTK Complications
Watch out for the following adverse events after the procedure:
- Recurrence of disease
- Infections
- Reactivation of herpes simplex virus
- Delayed healing of epithelium
- Corneal haze or scarring
- Hyperopic shift
Postoperative Management
We as optometrists play a crucial role in the postoperative management of PTK. As the referring doctor, trust has been established. Patients will likely choose to return to be comanaged. Initially, these patients should be educated and advised about the first four days after surgery. Burning, stinging, irritation, light sensitivity and overall discomfort is to be expected since a large epithelial defect is present. Individuals with a history of herpes simplex keratitis should be prophylactically treated with oral antivirals to prevent reoccurrence.
Similar to photorefractive keratectomy (PRK), patients will have a BCL after the procedure. Our practice schedules post-op visits at four days and one month after surgery.
At the day-four visit, a healed epithelium or epithelial ridge should be present. If an epithelial defect is still visible, it is not advised to remove the BCL at that time. The patient should return at a later date; otherwise, there is a risk of an iatrogenic corneal erosion during the removal of the BCL.
 |
|
Fig. 5. Epithelial thickness mapping in Case A shows thickening overlying the depressed corneal scar. Click image to enlarge. |
As a tip, if a patient’s BCL continues to fall out without any manipulation from the patient, try using a larger diameter lens or recommend a temporary tape tarsorrhaphy. This can alleviate a patient’s concern and prevent multiple trips back to the office.
Patients are prescribed a combination antibiotic/anti-inflammatory eye drop for two weeks. We use Pred-Moxi (prednisolone acetate and moxifloxacin; Imprimis) QID for one week, then BID for one week. The patient is also advised to heavily lubricate with preservative-free artificial tears, especially during the first week. Oral NSAIDs are recommended for patients in a considerable amount of pain. Topical anesthetic is handed out to patients for rare circumstances. We do not dilute the bottle and advise patients to discard by day two postoperatively. Patients need to be well educated prior to using these drops, as instilling more than six times a day can result in delayed wound healing. Remember, compared to PRK, there is a higher risk for poor healing, infection and haze after PTK since these corneas are routinely not “normal.”
 |
|
Fig 6. Anterior segment OCT reveals a subtle stromal haze centrally. The overlying scar is not well depicted. Due to the location of this opacity lying within the anterior third of the cornea, it would respond well to PTK. Click image to enlarge. |
Which First: PTK or Cataract Surgery?
When patients with cataracts present to your office, they will have complaints of decreased BCVA, increased glare and halos at night and/or struggles with their daily living activities. Accurate biometry and keratometry is essential for calculating an appropriate IOL to ensure the best postoperative visual outcome.
Corneal pathologies like EBMD can affect the reliability of these measurements. If an irregularity visualized on slit lamp examination is supported by abnormal topography or epithelial thickness mapping, an RGP over-refraction is a crucial next step. The RGP over-refraction utilizes the tear film to mask the corneal surface, diagnostically ruling out whether the cornea, cataract or both are impeding vision. If there is subjective improvement, it is worth optimizing the ocular surface with a PTK first. Not only will this smooth the surface to aid in IOL calculations, but patients may see enough of an improvement to defer cataract surgery.
PTK should also be considered if a patient is motivated to be more independent from glasses. For these individuals, a premium diffractive multifocal IOL is a great option. However, any retinal or corneal pathologies can limit their candidacy. To avoid missing subtle epithelial changes, make sure to lift your patients’ lids up while behind the slit lamp. Sodium fluorescein staining can additionally help highlight areas of negative staining in EBMD.
Once a PTK is performed, patients will wait a minimum of three months before repeating measurements and proceeding with cataract surgery. This provides the cornea enough time to heal, and our patients have been successful with this implemented timeline. It is often a longer journey, but a patient’s visual outcome can improve from 20/25 to 20/30 down to 20/20.
While a patient with superficial corneal irregularities can elect to have cataract surgery first, it is important to consider and recommend PTK if an RGP over-refraction subjectively improves vision. PTK is a powerful tool and option for patients motivated to improve their visual outcome. At the cataract evaluation, it is important to manage patient expectations and help them understand that while this may be a long journey, it will ultimately improve the patient’s success in IOLs.
 |
|
Fig. 7. Anterior segment OCT of the left cornea with visually significant stromal haze. Click image to enlarge. |
Case B. Repeat PTK on Stromal Haze
An 84-year-old female presented to our clinic with complaints of “viewing through a haze” in the left eye (Fig. 7). The patient had a history of a DMEK OS and a corneal abrasion OS that left a central scar, which had previously been treated with PTK in 2016 (Fig. 8).
At this visit, an RGP over-refraction improved her vision OS from 20/30 to 20/20. The source of her visual complaints was determined to be primarily from her stromal haze. Due to her motivation and subjective improvement noted, she elected to proceed with a repeat PTK OS.
 |
|
Fig. 8. Pentacam of this patient with a history of a DMEK who presented with stromal haze. Axial curvature highlights the irregularity on the anterior cornea. Click image to enlarge. |
Conclusion
Phototherapeutic keratectomy is a versatile procedure with an excellent risk/benefit ratio. Many anterior corneal pathologies can respond well to the excimer laser. This procedure can reduce the rate of recurrences and potentially prevent a patient from undergoing a corneal transplant.
If a reduced image quality is partially due to a form of corneal involvement amenable to excimer laser treatment, PTK should be considered first for your patients and prior to cataract surgery to optimize IOL calculations.
Both Drs. Ibach and Nguyen work at Vance Thompson Vision in Sioux Falls, SD. There, Dr. Ibach is a residency trained optometrist and is the residency co-coordinator. Dr. Nguyen is currently completing her advanced clinical training in ocular disease with an emphasis in ocular and refractive surgery, glaucoma and anterior segment.
1. Dinh R, Rapuano CJ, Cohen EJ, Laibson PR. Recurrence of corneal dystrophy after excimer laser phototherapeutic keratectomy. Ophthalmol. 1999;106(8):1490-7. 2. Keane M, Coffey N, Jones V, et al. The Australian corneal graft registry: 2021/22 report. Flinders Univ. 2022. 3. Baryla J, Pan YI, Hodge WG. Long-term efficacy of phototherapeutic keratectomy on recurrent corneal erosion syndrome. Cornea. 2006;25(10):1150-2. 4. Cavanaugh TB, Lind DM, Cutarelli PE, et al. Phototherapeutic keratectomy for recurrent erosion syndrome in anterior basement membrane dystrophy. Ophthalmol. 1999;106(5):971-6. 5. Spaeth GL, Danesh-Meyer H, Goldberg I, Kampik A. Ophthalmic surgeries principles and practice (4th ed.). Elsevier-Saunders. 2012. 6. Waring GO 3rd, Rodrigues MM, Laibson PR. Corneal dystrophies. I. Dystrophies of the epithelium, Bowman’s layer and stroma. Surv Ophthalmol. 1978;23(2):71-122. 7. Miller DD, Hasan SA, Simmons N, Stewart MW. Recurrent corneal erosion: A comprehensive review. Clin Ophthalmol. 2019;13:325-35. |


