Since their first arrival on the market in 1997, presbyopia-correcting intraocular lenses (IOLs) have had our patients demanding more from their cataract surgeries.1 The greatest causes of dissatisfaction after presbyopia-correcting IOL implantation are residual refractive error and dry eye, both of which can be corrected by identifying and treating the eye before the surgery.2 Treating dry eye disease (DED) will stabilize the tear film, capture more accurate measurements and reduce residual refractive error.3
Researchers on behalf of the Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study group found the incidence of dry eye in patients scheduled to undergo cataract surgery in a real-world setting is higher than anticipated.4 And, in a 2017 study, it was found that when DED was tested for, more than half of patients were diagnosed with definite or probable DED before cataract surgery.5 Dry eye is common and can be exacerbated by cataract surgery.
Eyecare practitioners should assess for pre-existing DED and initiate treatment before surgery.6 A healthy tear film is prerequisite for optimal visual performance, especially in patients receiving multifocal IOLs.7 Any ocular surface disease (OSD), including DED, can reduce visual acuity and adversely affect refractive measurements before ocular surgeries.8
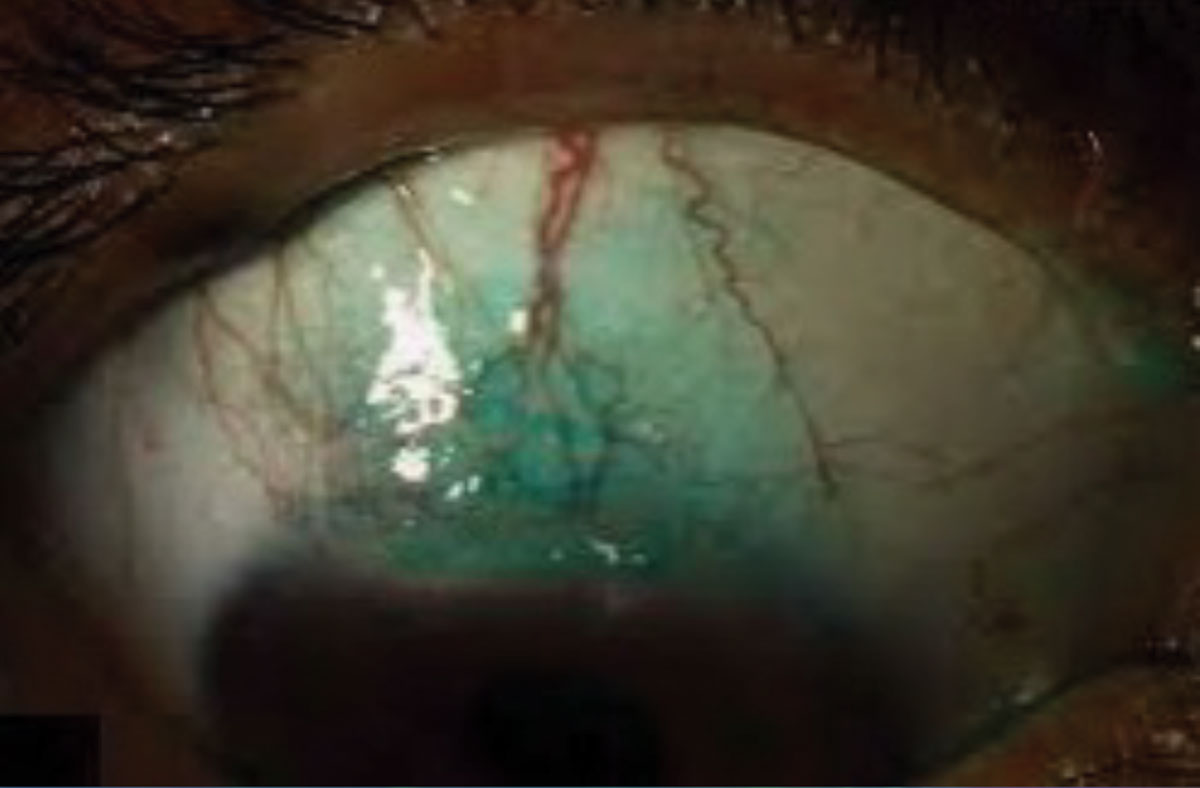 |
| Pictured here is a 3+ lissamine green stain on conjunctiva from dry eye. Click image to enlarge. |
Does Cataract Surgery Cause DED?
Cataract surgery has been reported in the literature to induce dry eye and to exacerbate pre-existing dry eye.9 Both ophthalmologists and the referring optometrist need to assess for pre-existing DED.6 Several factors during ocular surgery can have a profound effect on exacerbating or initiating OSD.
The detrimental effects of cataract surgery on the ocular surface can both directly cause and exacerbate pre-existing DED.10 There are multiple mechanisms resulting in exacerbation of surface disease after cataract surgery.11 These factors include:
• The corneal incision causes decreased sensation over the incision width extending in a wedge-shaped sector.12 This sensory loss may take months to return to normal and is likely to upset tear film homeostasis while compromised.13 The incision itself can potentially cut through the nerves responsible for innervating the corneal surface and, by doing so, may delay the epithelial wound healing.14 Effects on the cornea caused by cataract surgery which can lead to dry eye are greater in eyes that already have symptoms of DED.15
• Meibomian gland function may be altered without accompanying structural changes after cataract surgery.9 Lid margin abnormalities were found at three months post cataract surgery.16
• Increased inflammation due release of postoperative inflammatory mediators.11
• Photokeratitis due to light from the operating microscope during surgery.11 Such exposure can also be a contributing factor to the patient’s dry eye syndrome.17 Excessive light exposure during ophthalmic procedures could be a pathogenic factor in dry eye syndrome after a surgery is performed.18
• Chemical toxicity from preservatives such as benzalkonium chloride (BAK) used in postoperative eye drops. BAK can cause tear film instability and reduce the number of mucin-expressing cells.11,19
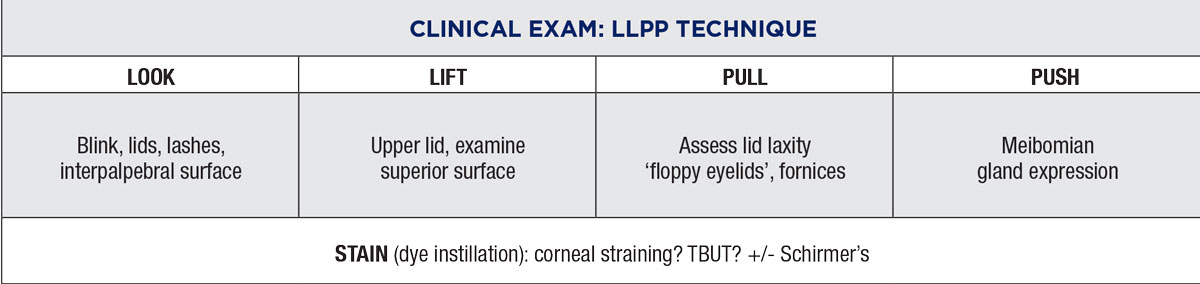 |
An algorithm developed by the ASCRS to assess the ocular surface prior to cataract surgery. This can help guide optometrists in knowing when to refer patients to an ophthalmologist. Click image to enlarge. |
The OD's Role in Surgery
We now know that cataract surgery alone can induce and worsen OSD.9 Having pre-existing DED will be reduced accuracy of measurements for surgical planning.6 Studies have shown that dry eye symptoms, such as blurred vision, are sometimes erroneously attributed to the cataract. This may contribute to the higher postoperative incidence of DED diagnosis.20
Precise topography and biometric measurements are prerequisites for postoperative visual performance.21 These measurements require a healthy and stable precorneal tear film, as it is the first refractive component of the eye.22
The American Society of Cataract and Refractive Surgery (ASCRS) developed an algorithm to assess the ocular surface prior to surgery.8 The first step is biometry measurements. If you are not working alongside a surgeon, you may not have access to the equipment needed for this step. However, the algorithm can still be used to guide optometrists when to refer to an ophthalmologist for surgery.
You could use the testing protocol developed by investigators in the PHACO study. Here, researchers sought to identify DED prior to cataract surgery. They used a simple battery of tests that can be performed without needing expensive devices, including tear break-up time (TBUT), fluorescein stain, lissamine green stain, Schirmer’s test and the Ocular Symptom Disease Index (OSDI).23
Ideally, the measurement scales used to identify clinical change in the patients should track progression of disease.24 Use corneal staining to track the progress of treatment. Fluorescein stain is used to elucidate corneal punctate staining, as it shows small area of pooled dye in a space where the cell surface is disrupted or completely missing.25 Lissamine green dye, on the other hand, penetrates membrane damaged conjunctival cells to stain the nucleus.25
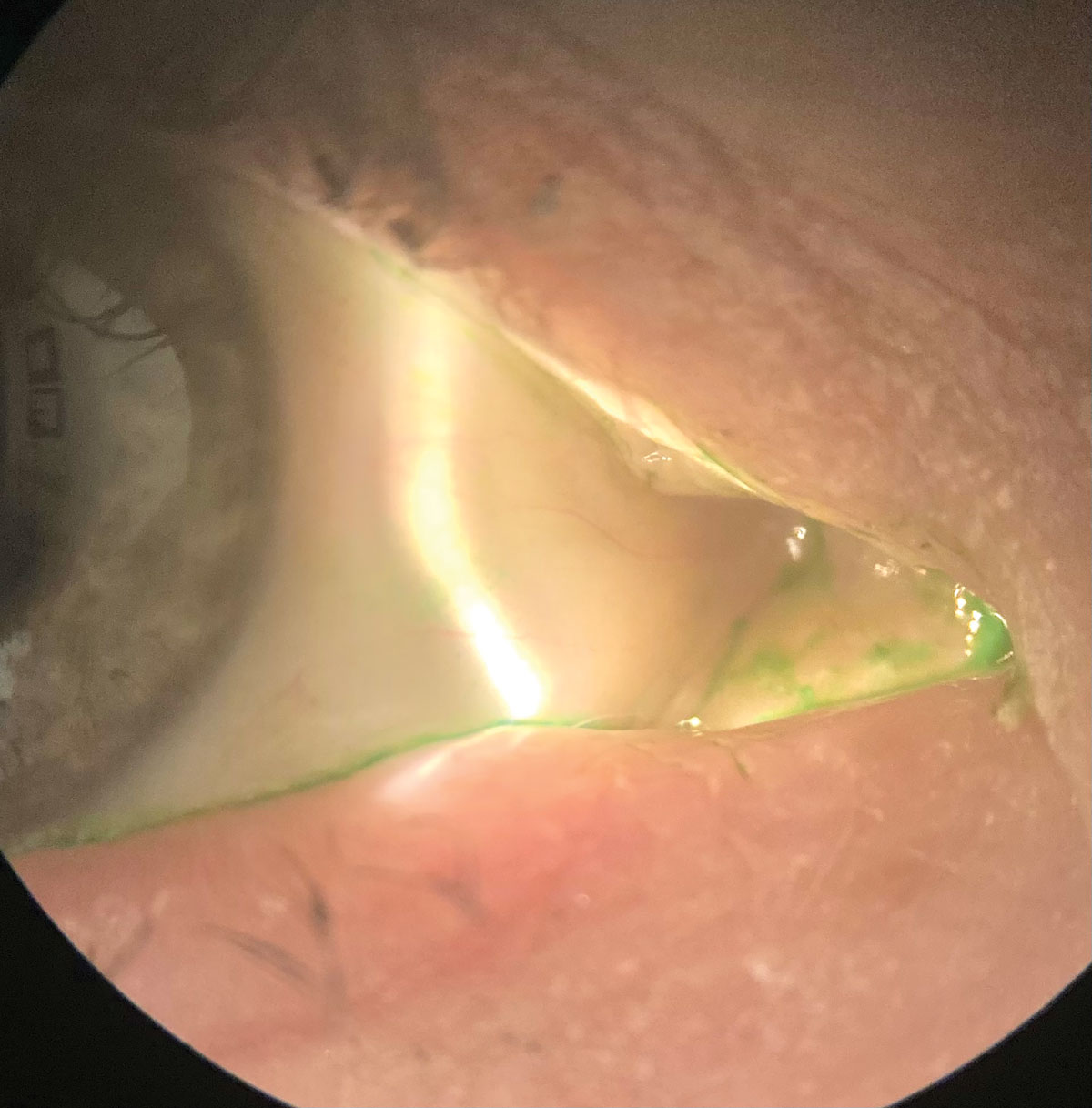 |
Another lissamine green stain seen on a patient. Click image to enlarge. |
If your clinic does not have any additional testing devices, you can still perform testing based on both the ASCRS Algorithm and the PHACO study. In both studies, a screening survey (OSDI or SPEED) and a slit lamp examination that include fluorescein and lissamine green stain, TBUT and Schirmer’s are recommended.
Treat the eyes based on the subtype and severity of the OSD and have the patient return in two to four weeks and repeat the exam. Only when OSD is ruled out during a normal exam without signs, symptoms or staining, should IOL calculation and surgery proceed.8
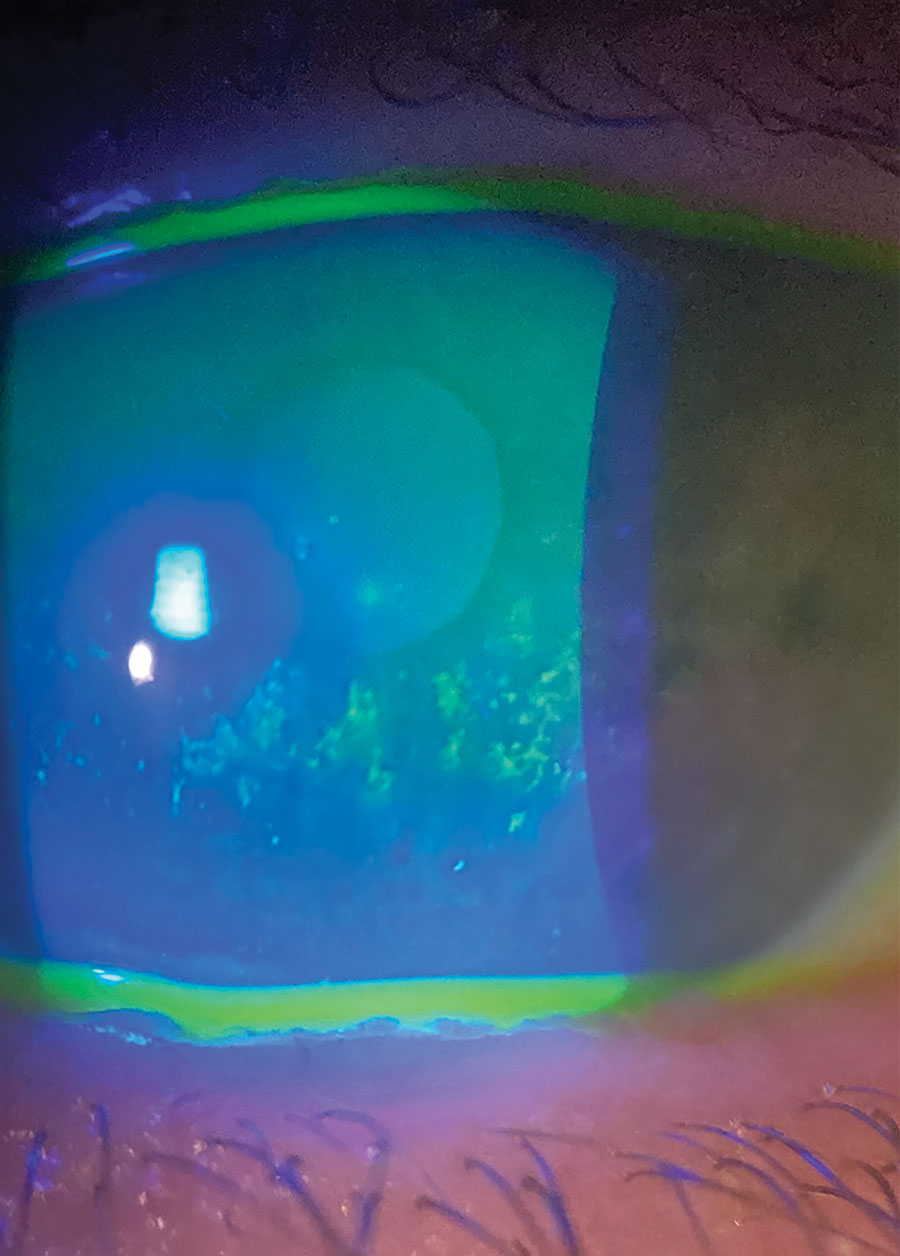 |
| Pictured here is a 2+ fluorescein stain. Click image to enlarge. |
Treat OSD Before Referring for Surgery
Let’s examine the most common OSDs and how to treat them effectively to prepare the patient for surgery.
• DED. The PHACO study found almost 60% of patients undergoing screening for routine cataract surgery showed signs of DED, including a reduced TBUT and central corneal staining with fluorescein dye.23
Preoperative use of artificial tear therapy alone has not been shown to prevent DED postoperatively.6 However, patients who used lifitegrast 5% (Xiidra, Novartis) BID for four weeks preoperatively showed improvements in higher-order aberrations, accuracy of pre-operative biometry, symptom scores (SPEED), TBUTs and corneal fluorescein staining.26
Another randomized clinical trial (RCT) showed use of Cequa (cyclosporine 0.09%, Sun Pharmaceuticals) BID for 28 days gave significant improvement in the prediction error of the spherical equivalent outcome of surgery.27
Cryopreserved amniotic membrane (CAM) is useful in treating DED, as its short-term efficacy is attributed to its potent anti-inflammatory effect.28 DED treatment with CAM also increases corneal nerve density, which correlates to increased corneal sensitivity and reduced dry eye symptoms.29
The results of the retrospective DREAM (Dry Eye Amniotic Membrane) study demonstrated that CAM treatment can accelerate the recovery of corneal surface in patients with moderate and severe DED. The DREAM study used CAM for three to seven days and showed significant improvement of both DED signs (corneal staining) and symptoms (ocular discomfort score).30 Optimal duration of CAM placement was five days to achieve an average symptom-free duration of four months in patients with DED.28 The expediency of this treatment in stabilizing the ocular surface makes it an excellent treatment prior to cataract surgery.
• Epithelial basement membrane dystrophy (EBMD) and recurrent corneal erosion (RCE). Ocular surface disease encompasses a broad variety of conditions, including EBMD, RCE, Salzmann’s nodular degeneration (SND), ocular allergy and conjunctivochalasis, and they all share inflammation as the common underlying etiology.31 EBMD, also known as map-dot-fingerprint dystrophy, is the most common corneal dystrophy.32 It affects over 2% of the population worldwide.33
Long-standing inflammation and elevation of key matrix-metalloproteases and cytokines associated with DED may ultimately lead to disorganization of the basement membrane seen in EBMD and SND.34 CAM is known to contain potent anti-inflammatory mediators and growth factors, as well as potent anti-fibrotic, anti-angiogenic, pro-healing effects important in promoting regenerative healing.35
 |
| A patient undergoing epithelial debridement. Click image to enlarge. |
Meibomian gland dysfunction (MGD). This may be altered even without structural changes of the gland after cataract surgery.9 Preoperative at-home management of MGD should include warm compressors, lid hygiene and anti-inflammatory treatment.36 The anti-inflammatory and antimicrobial effects of treatment of MGD oral tetracycline antibiotics and topical azithromycin may reduce bacterial proliferation and improve meibum secretion.16
In addition to at-home therapy, studies have shown that thermal pulsation treatment prior to cataract surgery is also beneficial to postoperative outcomes. Thermal pulsation treatments such as LipiFlow (TearScience, Johnson & Johnson) showed significant improvement in meibomian gland patency, meibum quality, increased TBUT and reduced corneal staining, as well as symptoms reported on the OSDI. In fact, even patients without preoperative MGD who were treated with thermal pulsation showed less worsening or improvement of MGD and DED induced by surgery.37
In a separate RCT, TearCare (Sight Sciences) was shown to be equally effective to LipiFlow in significantly reducing the signs and symptoms of DED in patients with MGD prior to cataract surgery.38
Treating DED After Surgery
Even with the ocular surface evaluation performed preoperatively, the incidence of dry eye after phacoemulsification has been reported to be 9.8%.41 The use of eye drops during and after surgery, because of the harmful effects of preservatives, may lead to injury to corneal epithelial and conjunctival epithelial and goblet cells.11
Following routine cataract surgery, patients are typically given treatment regimens of topical steroid, nonsteroidal anti-inflammatory and antibiotic drops as part of standard care.42 Such topical medications usually contain preservatives. Both laboratory and clinical studies have demonstrated the toxic properties of eye drop preservatives on the ocular surface.43
I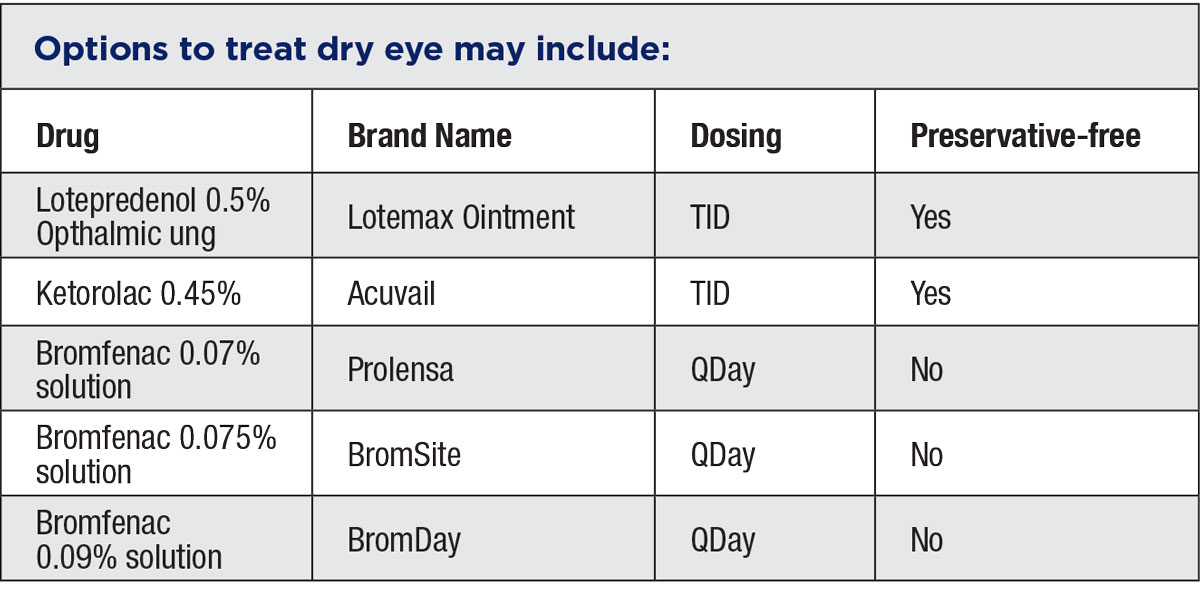 |
Opting for alternative delivery methods of the necessary post-op medications is a great way to mitigate the effects of BAK preserved drops on the ocular surface. Clinical signs associated with the use of BAK-preserved drops include superficial punctate keratitis, conjunctival hyperemia, staining and follicles, increased osmolarity, decrease in tear production and a reduction in TBUT.44
An RCT of 80 patients supported the use of preservative-free drops after cataract surgery to minimize DED.45 Switching to a preservative-free formulation removes the potential harmful effects of introducing a preservative to the ocular surface.17
Reducing the dosing of postoperative drops is another way to protect the ocular surface. Bromfenac 0.075% (BromSite) outcomes from dosing BID were equivalent to the outcomes from dosing with 0.075% bromfenac QD in an uncomplicated postoperative cataract surgery.4
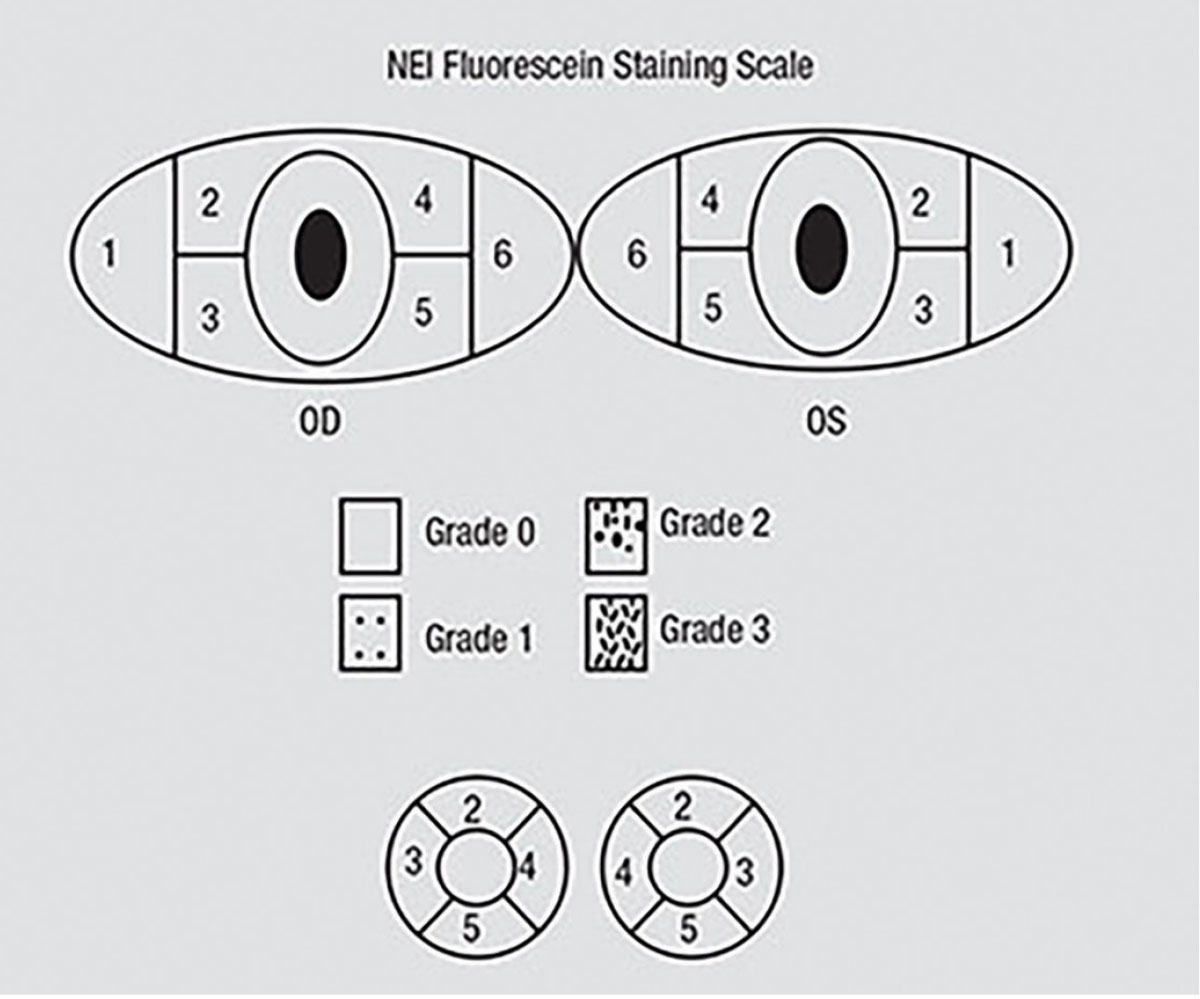 |
The NEI scale for grading fluorescein staining divides the corneal and conjunctival surfaces to help measure fluorescein uptake. A standardized grading system of 0 to 3 is used for each of the five areas on each cornea. Grade 0 is specified when no staining is present. Click image to enlarge. |
Alternatively, “dropless cataract surgery” is a great way to eliminate or reduce the burden of topical medications. It involves intravitreal injection of a single-use, compounded combination of antibiotics and corticosteroids.39
The side effects of postoperative drop use can also be minimized using intracameral antibiotics and sub-Tenon’s injection of steroids. Intracameral use of antibiotics during surgery is a safe and effective method to prevent post-cataract endophthalmitis.46 This in conjunction with a single sub-Tenon’s intracameral triamcinolone to control inflammation following cataract surgery will reduce postoperative drop burden.47
Even with the best preoperative screening and postoperative care, some patients will still experience new of exacerbated symptoms of DED. Postoperative management of DED is crucial in ensuring that tear film homeostasis is preserved as much as possible and to avoid long-term adverse effects of the ocular surface.6
Two clinical trials have shown that using cyclosporine 0.05% drops to optimize tear film function after cataract surgery may have protective effects on the ocular surface after cataract surgery.48,49 A separate RCT indicated that receiving omega-3 supplements (1000mg TID PO for one month after cataract surgery) had better symptoms (OSDI scores) and signs (higher TBUTs) than patients who did not take omega-3s.50
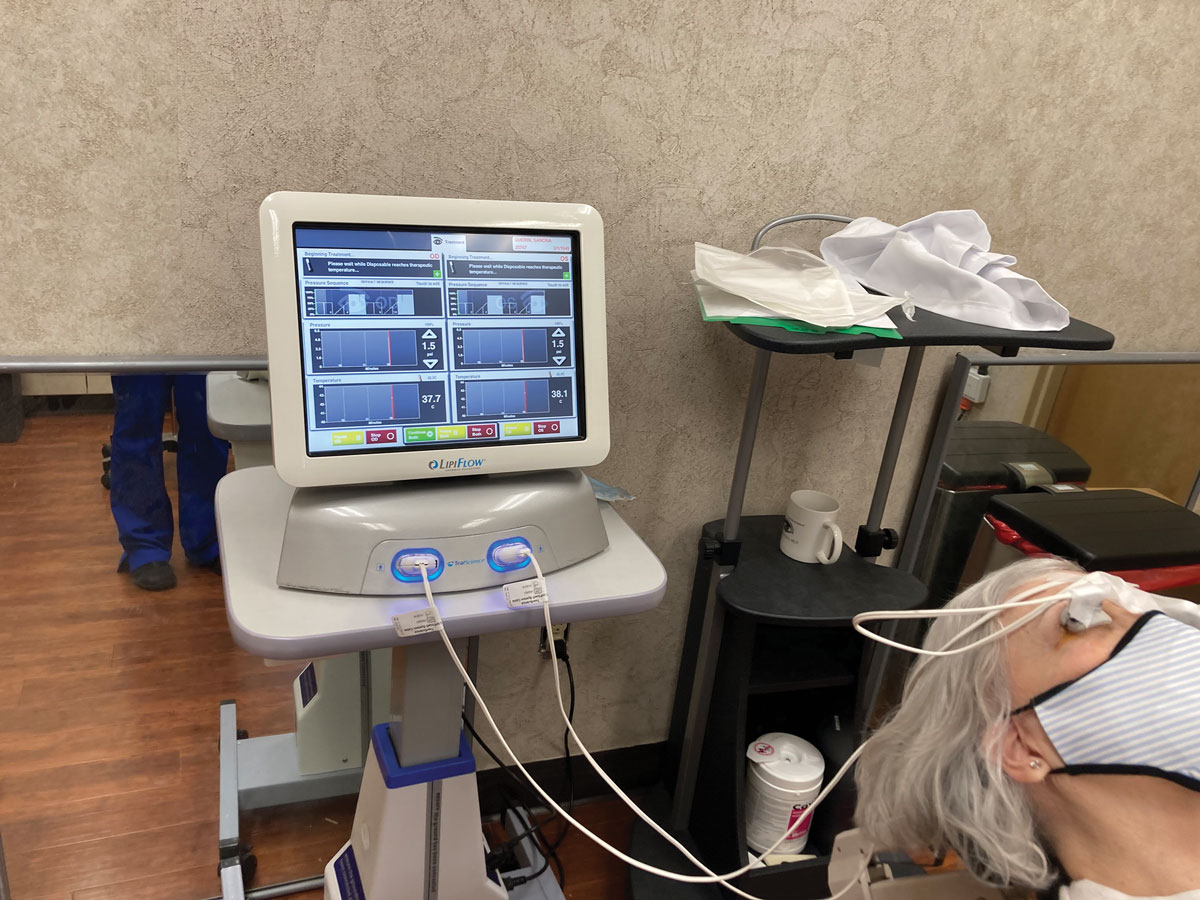 |
LipiFlow treatment has shown improvement in meibomian gland patency, meibum quality, increased TBUT and reduced corneal staining prior to cataract surgery. Click image to enlarge. |
Takeaways
Dry eye disease can have a negative impact on the mental well-being of a patient. A systematic review demonstrated that patients with DED have higher rates of anxiety and depression compared to controls.51 DED also carries a high economic burden at an estimated annual cost of treating a single dry eye patient in the United States to be $11,302.52
Ocular surgery can exacerbate or induce OSD, leading to worsened vision, increased symptoms and overall dissatisfaction.8 Preoperative screening and assessment for DED is essential to ensure that patients receive appropriate treatment prior to surgery. This will also ensure that accurate biometry measurements are obtained for surgical planning.6 Treating OSD preoperatively will ensure postoperative visual outcomes and patient satisfaction can be significantly improved.8
Dr. Theriot practices at a multi-specialty eye clinic in Shreveport, LA. Her clinical practice covers a broad spectrum of ocular care with a unique clinical focus on ocular surface disease and dry eye. She received her doctorate in optometry from the University of California at Berkeley, School of Optometry, and completed her residency at the State University of New York, College of Optometry. She is a consultant for Novartis and key opinion leader for Sun Pharmaceuticals and Kala Pharmaceuticals.
1. Hiraoka T, Asano H, Ogami T, et al. Influence of dry eye disease on the measurement repeatability of corneal curvature radius and axial length in patients with cataract. J Clin Med. 2022;11(3):710. 2. Gibbsons A, Ali T, Waren D, Donaldson K. Causes amd correction of dissatisfaction after implanation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965-70. 3. Matossian C. Impact of thermal pulsation treatment on astigmatism management and outcomes in meibomian gland dysfunction patients undergoing cataract surgery. Clin Ophthalmol. 2020;14:2283-9. 4. Trattler W, Hosseini K. Twice-daily vs. once-daily dosing w ith 0.075% Bromfenac in DuraSite: outcomes from a 14-day phase II study. Ophthalmol Ther. 2017;6(2):277-84. 5. Miyake K, Yokoi N. Influence on ocular surface after cataract surgery and effect of topical diquafosol on postoperative dry eye: a multicenter prospective randomized study. Clin Ophthalmol. 2017;11:529-40. 6. Naderi K, Gormley J, O’Brart D. Cataract surgery and dry eye disease: a review. Eur J Opthalmol. 2020;(5):840-55. 7. Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implanation. J Cataract Refract Surg. 2009;35:992-7. 8. Starr CE, Gupta PK, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Ref Surg. 2019;45(5):669-84. 9. Han KE, Yoon SC, Ahm JM, et al. Evaluation of dry eye and meibomian gland dysfunction after cataract patient (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-30. 10. Ishrat S, Nema N, Chandravanshi SCL. Incidence and pattern of dry eye after cataract surgery. Saudi J Ophthalmol. 2019;33(1):34-40. 11. Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and anaysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16-20. 12. John T. Corneal sensation after small incision, sutureless, one-handed phacoemulsification. J Cataract Refract Surg. 21(4):425-8. 13. Lyne A. Corneal sensitivity after surgery. Trans Ophthalmol Soc U K 1982; 102(pt. 2):302–5. 14. Chester T. Treat the front before the cut. Rev Optom. 2020. 15. Ram J, Gupta A, Brar G, Kaushik S, Gupta A. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28(8):1386-9. 16. Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100:300-6. 17. Sutu C, Fukuoka H, Afshari N. Mechanisms and management of dry eye in cataract surgery patients. Curr Opin Ophthalmol. 2016;27:24-30. 18. Hwang, Hyung & Kim, Hyun. (2014). Phototoxic Effects of an Operating Microscope on the Ocular Surface and Tear Film. Cornea. 33:82-90. 19. Wilson WS, Duncan AJ, Jay JL. Effect of benzalkonium chloride on the stability of the precorneal tear film in rabbit and man. Br J Ophthalmol. 1975;59(11):667-9. 20. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-8. 21. Koh S. Irregular astigmatism and higher-order aberrations in eyes with dry eye disease. Invest Ophthalmol Vis Sci. 2018;59(14):DES36-40. 22. Koh S, Tung C, Inoue Y, et al. Effects of tear film dynamics on quality of vision. Br J Ophthalmol. 2018;102(12):1615-20. 23. Trattler W, Majmudar P, Donnenfield E, et al. The prospective health assessment of cataract patient (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-30. 24. Abelson M, Smith L, Hollander D, Usner D. How do you quantfify the qualitative? Rev Ophthal. 2016;5(8). 25. Bron AJ, Argueeso P, Irkec M, Bright FV. Clinical staining of the ocular surface: mechanisms and interpretations. Prog Retin Eye Res. 2015;44:36-61. 26. Hovanesian J, Epitropoulos A, Donnenfield ED, Holladay JT. The effect of Liftegrast on refractive accuracy and symptoms in dry eye patients undergoing cataracy surgery. Clin Ophthalmol. 2020;14:2709-16. 27. Hovanesian JA, Epitropoulos A, Holladay JT. Effect of Cyclosporine 0.09% treatment on accuract of preoperative biometry and higher order aberrations in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2021;15:3679-86. 28. Cheng AM, Zhao D, Chen R, et al. Accelerated restoration of ocular surface health in dry eye disease by self-retained cryopreserved amniotic membrane. Ocul Surf. 2016;14:56-63. 29. John T, Tighe S, Sheha H, et al. Corneal nerve regeneration after self-retained amniotic membrane in dry eye disease. J Ophthalmol. 2017:6404918. 30. McDonald MB, Sheha H, Tighe S, et al. Treatment outcomes in the Dry Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018;12:677-81. 31. Acera A, Rocha G, Vecino E, et al. Inflammatory markers in the tears of patients with ocular surface disease. Ophthalmic Res. 2008 Oct;40(6):315-21. 32. He J, Bazan HE. Corneal nerve architecture in a donor with unilateral epithelial basement membrane dystrophy. Ophthalmic Res. 2013;49(4):185-91. 33. Lee WS, Lam CK, Manche EE. Phototherapeutic keratectomy for epithelial basement membrane dystrophy. Clin Ophthalmol. 2017;11:15-22. 34. Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-35. 35. Huang Y, Sheha H, Tseng SCG. Self-retained amniotic membrane for recurrent corneal erosion. J Clin Exp Ophthalmol. 2013;4:272-6. 36. Song P, Sun Z, Ren S, et al. Preoperative management of MGD alleviates the aggravation of MGD and dry eye induced by cataract surgery: a prospective, randomized clinical trial. Biomed Res Int 2019;2019:2737968. 37. Park J, Yoo YS, Shin K, et al. Effects of Lipiflow treatment prior to cataract surgery: a prospective, randomized, controlled Study. Am J Ophthalmol. 2021;230:264-75. 38. Gupta PK, Holland EJ, Hovanesian J, et al. TearCare for the treatment of meibomian gland dysfunction in adult patients with dry eye disease: a masked randomized controlled trial. Cornea. 2022;41(4):417-26. 39. Lindstrom RL, Galloway MS, Grzybowski A, Liegner JT. Dropless cataract surgery: an overview. Curr Pharm Des. 2017;23(4):558-64. 40. Zhang Z, Thomas LW, Leu SY, et al. Refractive outcomes of intraoperative wavefront aberrometry versus optical biometry alone for intraocular lens power calculation. Indian J Ophthalmol. 2017;65(9):813-7. 41. Kasetsuwan N, Satitpitakul V, Changul T, Jariyakosol S. Incidence and pattern of dry eye after cataract surgery. PLoS One. 2013;8(11):e78657. 42. Solomon KD, Sandoval HP, Potvin R. Comparing combination drop therapy to a standard drop regimen surgery: a prospective, randomized, controlled study. Am J Ophthalmol. 2021;230:264-75. 43. Epstein SP, Ahdoot M, Marcus E, Asbell PA, Comparative toxicity of preservatives on immortalized corneal and conjunctival epithelial cells. J Ocul Pharmacol Ther. 2009;25(2):113-9. 44. Walsh K, Jones L. The use of preservatives in dry eye drops. Clin Ophthalmol. 2019;13:1409-25. 45. Jee D, Park M, Lee HJ, et al. Comparison of treatment with preservative-free versus preserved sodium hyaluronate 0.1% and fluorometholone 0.1% eyedrops after cataract surgery in patients with preexisting dry-eye syndrome. J Cataract Refract Surg 2015;41:756–76. 46. Titiyal, Jeewan S; Kaur, Manpreet. Role of intracameral antibiotics in endophthalmitis prophylaxis following-cataract surgery. Ind J Ophthalmol. 2020;68(5):688-91. 47. Kim SY, Yang J, Lee YC, Park YH. Effect of a single intraoperative sub-Tenon injection of triamcinolone acetonide on the progression of diabetic retinopathy and visual outcomes after cataract surgery. J Cataract Refract Surg. 2008;34(5):823-6. 48. Donnenfeld ED, Solomon R, Roberts CW, et al. Cyclosporine 0.05% to improve visual outcomes after multifocal intraocular lens implantation. J Cataract Refract Surg. 2010;36:1095–100. 49. Ganesh S, Brar S, Bagare SN. Topical cyclosporine (0.05%) for management of dry eyes in patients undergoing cataract surgery-a comparative study. Open Ophthalmol J. 2019;13(1):3442. 50. Mohammadpour M, Mehrabi S, Hassanpoor N, et al. Effects of adjuvant omega-3 fatty acid supplementation on dry eye syndrome following cataract surgery: a randomized clinical trial. J Current Ophthalmol. 2017;29(1):33-8. 51. Wan KH, Chen LJ, Young AL. Depression and anxiety in dry eye disease: a systematic review and meta-analysis. Eye. 2016;30(12): 1558-67. 52. Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the United States: a decision tree analysis. Cornea. 2011;30:379-87. |


