Myopia already affects a massive proportion of the population in Asia.1 For example, Taiwan has rates of myopia of up to 84% in school children, and 97% of 19-year-old South Korean male military conscripts are myopic.2,3 Myopia is also becoming a problem beyond East Asia, with the United States reporting increases in prevalence from 25% to 42% between 1972 and 2002, and high myopia, in particular, increasing eightfold from 0.2% to 1.6% in those older than 30 over the same period.4 In Australia, where myopia levels are generally considered to be low, the Sydney Adult Vascular and Eye Study recently reported that almost 30% of 17-year-olds are myopic.5
Although individual studies provide essential information on the prevalence of myopia, they are difficult to generalize, as they cover specific ages, groups or places. For effective planning, policymaking and interventions regarding myopia, we must organize and understand the data to predict trends and estimate future prevalence.
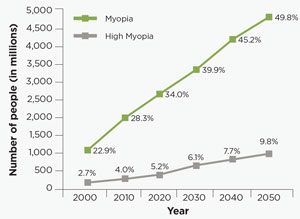 |
| Fig. 1. Estimated Global Prevalence of Myopia and High Myopia, 2000 to 2050. |
A study by the Brien Holden Vision Institute (BHVI), published in Ophthalmology in 2016, reported a meta-analysis of the global prevalence data on myopia and high myopia since 1995.6 Using the PubMed (National Library of Medicine) database to review the literature, this study highlights the condition’s prevalence across the 21 regions of global burden of disease (GBD), which are countries grouped together based on their geographic location and socioeconomic status (http://ghdx.healthdata.org/countries). Evidence of varying prevalence over time enabled our research team to create functions to predict the future prevalence of myopia and high myopia from 2000 through 2050 by decade. (see, “How BHVI Estimated Prevalence Rates Through 2050.”)
The model indicated the global prevalence of myopia affected almost 23% of the population in 2000. More importantly, it predicted that amount would grow to 50% of the world’s population by 2050 (Figure 1). Nearly 1.5 billion people were affected in 2000, and by 2050 this is expected to increase to almost five billion.6
High myopia is also set to rise from an initially low prevalence of almost 3% in 2000 to close to 10% in 2050. This equates to 163 million people in 2000, and by 2050 almost one billion people will be potentially at risk of developing permanent vision impairment and blindness associated with high myopia.6
Approaching 2050, the difference in prevalence rates between Asia and the rest of the world start to decrease, with many regions reaching a prevalence of more than 50%, presumably due to increasing urbanization and socioeconomic development. For example, in 2010, the high-income Asia-Pacific nations had a prevalence of 48.8%, while Eastern Europe and North Africa and the Middle East had prevalences of 25% and 14.2%, respectively. But by 2050, the research suggests, the gap will close, with Eastern Europe reaching a prevalence rate of 50.4%, North Africa and the Middle East jumping to 52.2% and high-income East Asia moving up less significantly to 66.4% (Figure 2).6
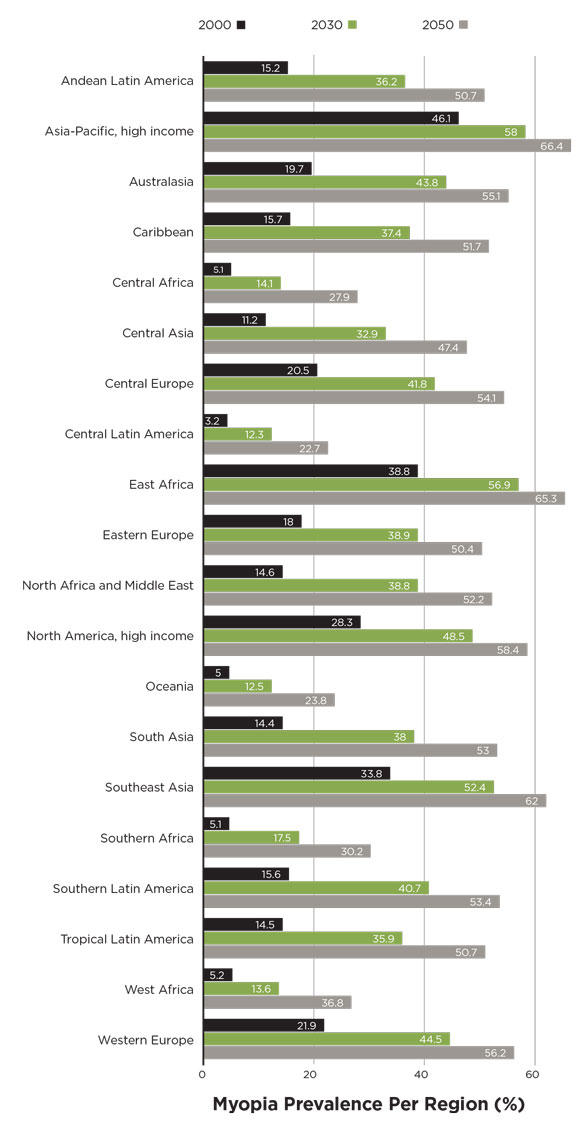 |
| Fig. 2. Regional prevalence of myopia in 2000, 2030 and 2050. Source: Adapted from Holden BA, et al. |
The projected increases in myopia and high myopia are largely considered to be driven by environmental factors and lifestyle changes, such as reduced time outdoors and increased near-based activities.1 Genetic predisposition is also a factor, but it cannot explain the rapid changes in prevalence seen in such a short timespan.7
Research suggests the high-pressure educational systems children are subjected to at very young ages in countries such as Singapore, Korea, Taiwan and China may be a major contributing lifestyle factor.1 Excessive use of electronic devices could also play a role.1
Other factors thought to be involved in myopia development and progression include light levels and specific wavelengths, time outdoors, vitamin D and peripheral defocus in the corrected and uncorrected myopic eye, stimulating axial elongation.8 Different light levels, different wavelengths and duration of light have been shown to affect axial elongation in animal studies, but are yet to be tested in humans.8 Trials conducted in Taiwan and China indicate time outdoors reduces risk of developing myopia, with less myopia progression seen in summer vs. winter months.9-11 The role of vitamin D in myopia is unclear; some reports suggest it is linked with myopia, while others have found no association.12,13 Investigators also found diet was not associated with myopia in a group of healthy children in Singapore.14
The BHVI study results show that, in the year 2000, the majority of myopia was occurring in those younger than 40, reflecting the major change in lifestyle in children and young people over the last two decades, especially in Asia.6 Due to urbanization and development, similar lifestyle factors will likely spread to other parts of the world that are still developing.
As a consequence of the rising prevalence of myopia, there will be substantial demand for increased eye care resources for refractive services, such as spectacles and contact lenses, in correcting the refractive error and treating myopia progression. In addition, there will be a need for managing and preventing high myopia–related ocular complications.
Uncorrected refractive error is already the primary cause of distance vision impairment globally, affecting 108 million people.15 It is also the second most common cause of global blindness.15 The economic burden of uncorrected distance refractive error was estimated to be $202 billion annually, of which myopia was the main cause.16 As a consequence of rising myopia levels, the prevalence of uncorrected refractive error and the associated burden will increase. High myopia also increases the risk of potentially sight-threatening conditions such as glaucoma, myopic macular degeneration, cataracts and retinal detachment.17 One billion people are predicted to be highly myopic by 2050, and the number of people with vision loss resulting from high myopia is predicted to increase sevenfold from 2000 to 2050.6 Based on these projections, myopia is set to become a leading cause of blindness worldwide.
Next Steps: Management
Many unanswered questions remain. To intervene at the appropriate stage, we need to better understand the risk factors associated with myopia onset and progression—such as ethnicity, lifestyle and parental myopia. It is important to regularly monitor population trends and characteristics to identify risk factors and adjust behaviors and management accordingly to limit the burden of rising myopia. For example, myopia has traditionally been treated with single vision spectacles and contact lenses, but now we know there are other options.
| How BHVI Estimated Myopia Rates Through 2050 |
| • Selected 145 relevant studies from a pool of 4,288 PubMed articles, representing 2.1 million individuals with myopia. • Combined myopia prevalence data with world population data and stratified data into age cohorts in five-year increments. • Defined myopia as spherical equivalent ≤-0.50D and high myopia as spherical equivalent ≤-5.00D.* • Grouped countries by GBD region for applicability to other epidemiological studies. (Results were extrapolated for GBD regions lacking myopia data). • Performed meta-analysis of prevalence data, combined with myopia change over time, to project prevalence rates for each decade from 2000 to 2050. *Spherical equivalent ≤-0.50D, the most commonly used myopia definition, is beyond the refraction measurement error and captures children at the start of their progression. Spherical equivalent ≤-5.00D for high myopia identifies people at higher risk of pathologic myopia and, if uncorrected, causes vision impairment equivalent to the World Health Organization’s blindness definition. |
Research has made considerable headway in identifying optical interventions that might aid in preventing the onset and progression of myopia. Optical interventions provide myopic defocus—bringing the image in front of the retina to slow axial elongation.18 The myopic eye tends to have relative peripheral hyperopia, and these interventions address this key risk factor. These strategies include bifocal spectacles, multifocal soft contact lenses and ortho-k—in combination with behavioral strategies such as reduced near work and more time outdoors, and pharmacological agents such as low-dose atropine. All these methods can help reduce the number of people with myopia progression.19
There is still much debate about when to start myopia control, what treatments should be used on whom and at what age. Optical treatments such as bifocal spectacles and multifocal soft contact lenses can be used full time as soon as a child is becoming myopic, and ortho-k is a good option if the child is a suitable candidate in terms of refractive error and their ability to perform extended wear. Concerning efficacy, the average slowing of myopia achieved across the bifocal spectacles, ortho-k and multifocal soft contact lenses are comparable, ranging from 35% to 50%.20-22 The choice often depends on the patient’s lifestyle and the rate of slowed progression achieved.
Low-dose atropine (0.01%) is commonly prescribed for myopia progression in places such as Hong Kong, Taiwan and Singapore, and, more recently, in some Western nations, one drop daily before sleep. Research shows the use of pharmacologic treatments such as low-dose atropine for myopia is safe in those as young as six, with the longest study being five years.23 The mechanism by which low-dose atropine works to slow myopia remains unclear, but it significantly slows the change in the spherical equivalent by 60% after two years, although this is not seen in a change in the axial length.23 Some caution is still required, as the effects of chronic treatment with low-dose atropine are unknown, including the overall level of myopia control when combining behavioral, optical and pharmacologic treatments.Although consensus surrounding myopia management has not yet been achieved, it is critical to successfully address the issue of myopia. The Brien Holden Vision Institute hopes to further foster the movement towards consensus through collaboration with researchers, clinicians and health bodies using our experience in advocacy in areas such as uncorrected refractive error.
More research is required to fully understand the mechanisms of myopia development and progression and identify those at risk of developing high myopia. Public health advocates will also need to develop wellness promotion strategies and provide resources such as clinical guidelines to respond to this significant public health challenge. Industry can also take a leadership role by working with researchers and clinicians to develop FDA-approved myopia treatments that will have a positive impact.
Overall, the world is becoming more myopic—a trend that has significant financial and societal implications. More importantly, high levels of myopia pose a threat to sight that reduces quality of life and exposes those affected to greater health risks. Evidence suggests myopia can be managed better by reducing the risk of the eye becoming more myopic with a number of lifestyle, optical and pharmaceutical interventions. The BHVI will be releasing the first online myopia management education program for optometrists in March 2017. Please go to www.brienholdenvisioninstitute.org for details.
| Want to learn more? |
| Access the freely available study at: www.sciencedirect.com/science/article/pii/S0161642016000257 |
Dr. Jong is senior research fellow at the Brien Holden Vision Institute (BHVI) in Sydney, Australia, and a visiting fellow at the University of New South Wales (UNSW), Australia.
Dr. Sankaridurg is program leader for the Myopia Program at BHVI and an associate professor at UNSW.
Dr. Fricke is a consultant at BHVI.
Dr. Naduvilath is head biostatistician at BHVI.
Dr. Resnikoff is a consultant at BHVI and a visiting professor at UNSW.
Dr. Naidoo is CEO of BHVI, a visiting fellow at UNSW and founder of the African Vision Research Institute, University of Kwa Zulu Natal, South Africa.
1. Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739-48.
2. Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Annals of the Academy of Medicine, Singapore. 2004;33:27-33.
3. Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in seoul, South Korea. Invest Ophthalmol Vis Sci. 2012;53:5579-83.
4. Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632-9.
5. French AN, Morgan IG, Burlutsky G, et al. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120:1482-91.
6. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016 May;123(5):1036-42.
7. Lim LT, Gong Y, Ah-Kee EY, et al. Impact of parental history of myopia on the development of myopia in mainland china school-aged children. Ophthalmology and Eye Diseases. 2014;6:31-5.
8. Smith EL 3rd, Hung LF, Arumugam B. Visual regulation of refractive development: insights from animal studies. Eye. 2014;28:180-8.
9. Wu PC, Tsai CL, Wu HL, et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080-5.
10. He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142-8.
11. Donovan L, Sankaridurg P, Ho A, et al. Myopia progression in Chinese children is slower in summer than in winter. Optom Vis Sci. 2012;89:1196-202.
12. Williams KM, Bentham GC, Young IS, et al. Association between myopia, ultraviolet B radiation exposure, serum vitamin D concentrations, and genetic polymorphisms in vitamin D metabolic pathways in a multicountry European study. JAMA Ophthalmol. 2017;135:47-53.
13. Tideman JW, Polling JR, Voortman T, et al. Low serum vitamin D is associated with axial length and risk of myopia in young children. European J Epidemiology. 2016;31:491-9.
14. Lim LS, Gazzard G, Low YL, et al. Dietary factors, myopia, and axial dimensions in children. Ophthalmology. 2010;117:993-7e4.
15. Bourne RR, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990-2010: a systematic analysis. The Lancet Global Health. 2013;1:e339-49.
16. Fricke TR, Holden BA, Wilson DA, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bulletin of the World Health Organization. 2012;90:728-38.
17. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Progress in Retinal and Eye Research. 2012;31:622-60.
18. Sankaridurg P, Holden B, Smith E 3rd, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52:9362-7.
19. Sankaridurg PR, Holden BA. Practical applications to modify and control the development of ametropia. Eye. 2014;28:134-41.
20. Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014;132:258-64.
21. Si JK, Tang K, Bi HS, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92:252-7.
22. Li SM, Kang MT, Wu SS, et al. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic & Physiological Optics. 2017;37:51-9.
23. Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016;123:391-9.


