A study by Mark Ritson, Ph.D., of the London Business School, found that contact lens patients are 60% more profitable for practices than patients who wear spectacles alone.1 Because many factors can influence our patients’ comfort in contact lens wear, it is important to have a thorough understanding of these influences that will often lead to many successful fittings. This knowledge will, in turn, lead to increased patient loyalty and practice profitability. But, in order to improve the rate of success, we must first measure it. We need to figure out how many existing patients we have and how many new contact lens fittings we perform on a monthly basis. Of course, this number will vary to a degree, but monitoring the overall trend and comparing it to where you are today is an important business step.
Understandably, there are many extraneous factors that affect the success of business including political, environmental and other elements. But, the business of contact lenses is one area optometry owns. We need to be very deliberate as to how we want to manage this business in our practice and understand how it affects the contact lens market as a whole. For that reason, our primary goal needs to be consistently finding ways to minimize dropouts and maximize new wearers.
Contact lens success is comprehensive. It includes good vision and lens comfort—patient education on proper wearing habits is just as critical. It also means careful evaluation for various “silent” causes of contact lens dropouts—like dry eyes, allergies, issues with compliance and choosing the right modality/material combination. These issues must be caught early and addressed up front in order to prevent more serious ramifications.
Focus on the Business of Contact Lenses
There is true value in providing these services. Many eye care professionals downplay our contact lens services when it comes to setting fees in our practices. It is not just about writing the prescription, even though, from the patient’s perspective, that may be the end product of everything that goes on behind the scenes.
Inferior papillary reaction jeopardizes successful contact lens wear.
The number of contact lens dropouts has the potential to substantially increase if eye care professionals don’t focus on ways to prevent them. According to the results of our survey, when patients did drop out, 45% did so within the first year of wearing contact lenses and 47% cited discomfort as the primary reason for dropping out.2 According to a global study by John B. Rumpakis, O.D., the typical age of the dropout was in the mid-twenties.3 In addition, more than one in six of your contact lens patients will discontinue lens wear.3 That is a big chunk of your bottom line. The study goes on to suggest that each dropout costs the business an average of $21,695 over the lifetime value of that patient.3 Keep in mind that not only were these patients purchasing contact lenses, but 33% were also purchasing spectacles.
Dr. Rumpakis, in the same article, cautions that the causes of contact lens dropouts are frequently misunderstood and underestimated.3 The economic impact of this misunderstanding is huge; the mean dropout rate in the United States is 15.9%.3 In order to prevent contact lens dropouts, it is critical that we, as practitioners, address the various causes of dropout with patients prior to prescribing contact lenses. This includes discussing any underlying pathology (dry eye, allergies), refitting the patient in newer technology materials (silicone hydrogel), prescribing the proper care system, utilizing the best modality to match the patient’s needs (daily versus frequent disposable), properly educating the patient on compliance, satisfying their visual needs and maximizing comfort.
Furthermore, the Contact Lens Council reported that 69% of consumers were not aware that new materials—specifically silicone hydrogels—are used in contact lenses to help alleviate dry eye symptoms.4 In addition, 83% of those consumers would be interested in contact lenses, if they could satisfy their visual requirements.4 Hence, there is an opportunity for eye care practitioners to discuss comfort options and help draw back some of the contact lens dropouts.
Addressing Dry Eye Complications
Dry eye can have a huge impact on the contact lens wearer and the contact lens practice. It is, therefore, important to identify and treat any underlying dry eye conditions prior to it affecting lens wear. According to the National Eye Institute’s Impact of Dry Eye on Everyday Life (IDEEL) questionnaire, approximately 34% of contact lens wearers discontinue use at least once, most frequently as a result of dry eye symptoms.5 With the systematic approach outlined below, eye care practitioners can minimize dry eye issues and maximize comfortable contact lens wear for many of their patients with underlying dry eye disease.
• Identify the problem. Don’t assume that your patients are wearing their contact lenses comfortably. Instead, patients may be silently dropping out of contact lens wear without your knowledge. Do your best to make sure that potential dry eye patients are identified through the medical history questionnaire and subsequent examination. Because patients are more likely to acknowledge an issue during the physical examination, be sure to ask about dry eye and allergies while you are evaluating their cornea behind the slit lamp. Here are some suggested questions for your appointment:
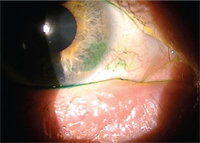
Limbal lissamine green staining secondary to a tight contact lens fit.
• What time do you take your contact lenses out in the evening? Why?
• Do your eyes ever burn, itch, water or feel scratchy while wearing your contact lenses?
• Do you ever experience intermittent blurred vision throughout the day? If so, how often does this occur?
• Do you use any eye drops throughout the day if/when your contacts feel dry?
• How many hours per day do you work at a computer?
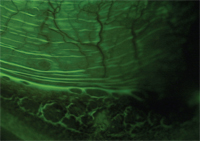
Although mentioned by many experts in the eye care field, it is important to reiterate the critical role dyes can play. The regular use of fluorescein allows for a detailed assessment of the anterior segment, including calculating the tear film break-up time (TFBUT), pinpointing the presence of corneal staining and acknowledging the presence of lid wiper epitheliopathy. Conjunctival staining with lissamine green can further reveal key characteristics of the previous lenses worn by the patient, like a tight lens and/or limbal irritation.
There is much promise with introduction of new tools, like the TearLab Osmolarity System. This non-invasive diagnostic test will provide a tear osmolarity measurement, which will quickly help practitioners assess if dry eye exists at all and, if so, to what severity.6
• Treat the underlying cause. Depending on the severity of dry eye, patients may require various levels of treatment during contact lens wear or be asked to discontinue lens wear use temporarily. The first step in the treatment of dry eye is to recommend that your patients modify their environment. Tell them to avoid direct sources of ventilation and educate them on the use of a humidifier. These simple environmental adjustments to their everyday routine can help retain moisture on the ocular surface. For example, a post-op LASIK patient came in to the office complaining of consistent dry eye, which was hindering his healing process. After determining that a nightly ceiling fan was contributing to the problem and discontinuing use, his corneas healed nicely and he responded well to the treatment.
One recommended treatment is the use of nutritional supplements—such as omega-3 and omega-6 fatty acids—to help stabilize the tear film.7,8 Also, consider prescribing a specific artificial tear for your dry eye patients. The supplements, along with dedicated use of the prescribed drops, are one of the most commonly recommended treatment, for dry eye.
For blepharitis or meibomian gland dysfunction (MGD) patients, I recommend the use of warm compresses and a more stringent eyelid hygiene regimen. Occasionally, an antibiotic eye drop such as AzaSite (azithromycin 1%, Insight Pharmaceuticals) or an antibiotic/steroid combination such as Tobradex ST (tobramycin/0.05% dexamethasone 0.3%, Alcon) may help alleviate acute and/or chronic eyelid disease.
Consider stronger therapies aimed at decreasing the inflammation, including t.i.d. or q.i.d. doses of Lotemax (loteprednol 0.5%, Bausch + Lomb) for short-term therapy.9 For long-term inflammatory modulators, consider the application of Restasis (cyclosporine 0.05%, Allergan) b.i.d. Finally, punctal occlusion or ophthalmic inserts like Lacrisert (hydroxypropyl cellulose, Aton Pharma) are other options to consider.
• Stress the importance of compliance. Our contact lens industry continues to develop new innovations in contact lens materials and is eager to introduce them to the market. In clinical practice, success depends not only on the science of the material, but also how well the lenses fit, whether patients are wearing them and how well they are adapting to them.

Address fluoroscein staining due to dry eyes prior to a contact lens fit.
Repeatedly, we have seen that if practitioners fail to reinforce proper lens care regimens, patients can be turned off from lens wear. For example, we can all agree that it is vitally important to wash your hands prior to inserting contact lenses. Yet, a recent survey reported that 35% of patients do not wash their hands before handling their lenses.10 These findings reinforce the need for practitioners to advocate compliant lens care; a few words can go a long way to increase comfort for those non-compliant wearers.
As the percentage of silicone hydrogel fits increases, rubbing and rinsing techniques are becoming the ritual. Silicone hydrogel lenses deposit lipids more readily than their hydrogel predecessors, making it important to rub. These lipids can potentially be uncomfortable. However, the simple act of rubbing and rinsing will minimize lipid deposition and increase comfort for the lens wearer.
In a recent study on contact lens wearer compliance, 20% of participants were unsure of the type of contact lenses they were wearing. In addition, 52% of those wearing two-week disposable contact lenses were non-compliant, while 28% of those wearing one-month replacement lenses and 12% of those wearing daily disposable lenses did not replace their contacts on a timely basis.11 You can increase compliance by discussing patient preferences prior to performing a lens fit and reinforcing proper wearing schedule at every visit.12
• Make patient education a priority. There are two things that are critical to long-term comfort with contact lens wear: cleanliness and moisture. First, clean, disinfected contact lens will reduce the microbial load on the patient’s eye. Second, a lens that stays wet will not dry out or build up a filmy surface. Added moisture prevents lenses from dehydrating throughout the day, which ultimately provides a comfortable—and more enjoyable—lens wearing experience.
When patients return for their post-trial contact lens evaluation, ask them to remove their lenses and check the cornea. If you see something wrong—adhesion, staining or infiltrates—you know there is a problem. Potential causes could be the specific contact lens, the solution being used or even the wearing schedule. The key to comfortable long-term lens wear is to identify these roadblocks before they become bigger problems.
Prescribing the Best Care System
How you recommend a care system can go a long way to solidifying patient loyalty and reducing lens dropouts. Instead of making a soft recommendation—such as handing your patients a starter kit as they leave your office—take the time to make a verbal recommendation or better yet, provide them with a written prescription.
Just like you’d prescribe artificial tears, you may want to recommend a specific contact lens solution to each patient. When something is written down—like your contact lens agreement form—compliance can be greatly improved. Another suggestion is to have your patients bring in their contact lens solutions and care systems to their appointment. With the products in hand, the eye care professional can better understand the lens wearing experience and patients can better describe any discomfort they may be experiencing. Finally, in addition to providing a written copy of the prescription after their fit, you may want to write the replacement schedule, the recommended contact lens solution and any specific patient notes at the bottom of the form.
Ultimately, these suggestions all lead to the need for increased patient education. Our patients only see us once a year. Clarity and emphasis are critical skills to perfect because they make the greatest impact and when our patients are not in our office, they are out in the real world receiving mixed messages from friends and commercial advertisements. One trip to the local drug store and I can easily see why our patients are confused. Our patients are bombarded with a variety of options, each at competing prices and with visually attractive packaging. When we take the time to educate our patients about which product we are prescribing and why, they are more likely to comply with our recommendation.
Understanding the Lenses
Silicone hydrogel contact lenses play a significant role in many practices. The generally high oxygen permeability (Dk/t) of these lenses allows for the minimization of the hypoxic stress to the cornea, which often results in less conjunctival hyperemia. Many practitioners have embraced silicone hydrogels as their material of choice for many of their contact lens wearers. This is because silicone hydrogels have continued to evolve; second- and third-generation silicone hydrogels have a lower modulus and a higher water content than the earlier generations. These lenses—Acuvue Oasys (Vistakon), Biofinity (CooperVision)—may improve the subjective comfort symptoms.13

Active blepharitis is treated aggressively with improved lid hygiene.
The daily disposable market share has exhibited perhaps the largest growth—76% of practitioners are using daily disposable lenses at a greater rate, which is the highest of all modalities surveyed.14 The newest designs—Proclear 1-Day (CooperVision), 1-Day Acuvue Moist (Vistakon), Dailies Aquacomfort Plus (CIBA Vision) and Acuvue TruEye (Vistakon)—attempt to maximize comfort by enhancing lens moisture.
Applying the Information Clinically
Understand that small changes to a contact lens regimen can make significant improvements to patients’ wearing experience. Identifying and treating any underlying causes continues to be a big concern, and reinforcing compliance at every patient encounter is a critical step. Knowing and understanding what care systems a patient is using and how they are cleaning their lenses also helps maximize comfort. Appreciate that newer generation contacts will continue to focus on bringing patients exceptional comfort. Those who embrace these newer technologies will likely see increased patient satisfaction, improved patient loyalty and a decreased dropout rate.
Mile Brujic, O.D., is a partner of Premier Vision Group, a four-location optometric practice in northwest Ohio.
Jason R. Miller, O.D., M.B.A., is a partner at EyeCare Professionals of Powell, Ohio, and serves as an adjunct faculty member for The Ohio State University College of Optometry.
1. Ritson M. Which Patients are More Profitable? CL Spectrum. 2006 Mar;21(3):38-40,42.
2. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Conact Lens Clin. 1999 Nov;26(6):157-62.
3. Rumpakis J. New Data on Contact Lens Dropouts: An International Perspective. Rev Optom. 2010 Jan;147(1):37-42.
4. Contact Lens Council. New survey finds more education on contact lenses and lens care will help consumers see 20/20. PR Newswire. 2007 Aug.
5. Abetz L, Venkataraman K, Mertzanis P, et al. The Development, Reliability and Validity of a Questionnaire to Assess the Impact of Dry Eyes on Everyday Life (IDEEL). Invest Ophthalmol Vis Sci. 2003;44(4):e-abstract 2477.
6. TearLab. Available at:
www.tearlab.com. (Accessed January 2011).
7. Rashid S, Jin Y, Ecoiffier T, et al. Topical omega-3 and Omega-6 fatty acids for treatment of dry eye. Arch Ophthalmol. 2008 Feb;126(2):219-25.
8. Kokke KH, Morris JA, Lawrenson JG. Oral Omega-6 essential fatty acid treatment in contact lens associated dry eye. Cont Lens Anterior Eye. 2008 Jun;31(3):141-6.
9. Pavesio CE, Decory HH. Treatment of ocular inflammatory conditions with loteprednol etabonate. Br J Ophthalmol. 2008 Apr;92(4):455-9.
10. Stone R. The importance of compliance: focusing on the key steps. Poster presented at 2007 Annual British Contact Lens Association meeting. May 2007; Manchester, United Kingdom.
11. Dumbleton K, Woods C, Jones L, Fonn D. How Compliant are Today’s Lens Wearers?. CL Spectrum. 2010 June. Available at:
www.clspectrum.com/article.aspx?article=104344.(Accessed January 2011).
12. Nixon GJ. A Review of Contact Lens Modalities. 2006 Mar. Available at:
www.clspectrum.com/article.aspx?article=&loc=archive\2006\march\0306032.htm. (Accessed August 2010).
13. Fonn D, Situ P, Simpson T. Hydrogel lens dehydration and subjective comfort and dryness ratings in symptomatic and asymptomatic contact lens wearers. Optom Vis Sci. 1999 Oct;76(10):700-4.
14. Nichols, JJ. Contact Lenses 2010. CL Spectrum. 2011 Jan. Available at:
www.clspectrum.com/article.aspx?article=105083. (Accessed January 2011).


