 |  |
Epithelial basement membrane dystrophy (EBMD) may be more common than we think. Literature suggests that it affects 2% to 3% of the global population.1,2 This is probably an underestimate, as EBMD is sometimes overlooked because of how subtle its clinical appearance can be. Here’s how to spot and manage it.
Clinical Presentation
EBMD happens when the basement membrane (BM) extends into the corneal epithelium. Basal corneal epithelial cells produce abnormal BM cells, leading to the region’s irregularity.2-4 As this occurs, the epithelium becomes uneven over the irregularly heaped areas of membrane, creating the elevations clinically seen as areas of negative staining and patterns of mapping, dots and fingerprints. Elevated epithelium due to BM irregularities is thinner than corresponding non-elevated epithelial tissue. This can be easily seen with AS-OCT (Figure 1).
As EBMD progresses, it can cause a progressive reduction in BCVA. Unfortunately, often this leads to variability in vision because of poor tear film qualities over the corneal irregularities and variability in the irregular patterns observed on the cornea. These patients’ refractive errors can vary with manifest refractions over separate visits. Usually this is seen as changes in the axis and amount of astigmatism measured.
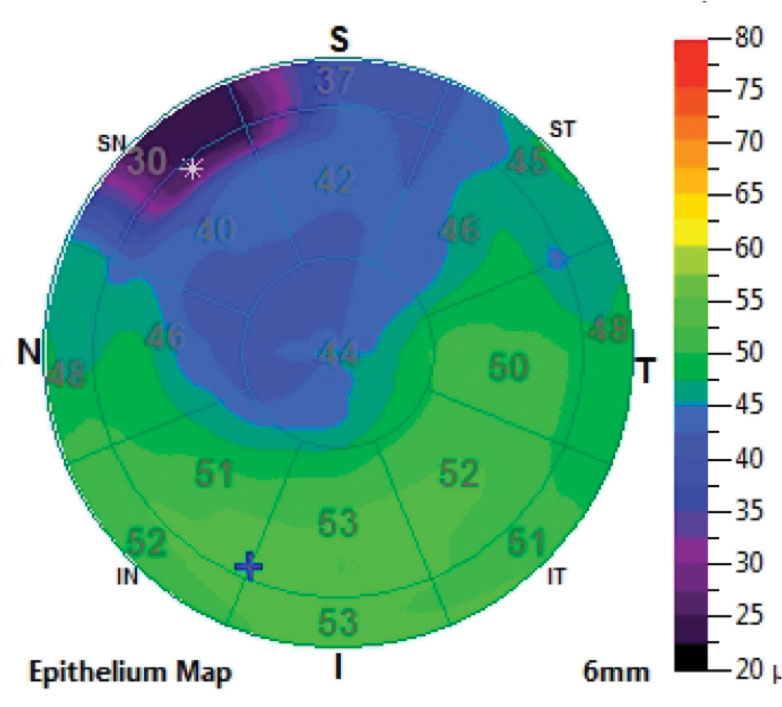 |
| Fig. 1. Epithelial thickness map shows thinning where the map pattern is located. Click image to enlarge. |
Vision Optimization
EBMD management strategies focus on promoting the health of the tear film and ocular surface. If any abnormalities exist, it is critical to treat them appropriately. In the presence of a normal tear film and ocular surface, lubrication via artificial tears, punctal plugs, Lacriserts or a combination of the three may be used.
A major concern for patients with EBMD is recurrent corneal erosion. Preventative measures include lubrication in the evening with bland and hyperosmotic saline ointments. More aggressive strategies to reduce the risk of recurrent events include epithelial debridement and phototherapeutic keratectomy.5-7
In the event of a recurrent erosion, the goal is to rehabilitate the cornea. In mild cases, a bandage contact lens can help the cornea heal. If the erosive event is more severe, consider an amniotic membrane.8
For patients who have a difficult time seeing well and experience fluctuating vision, there are several contact lens options that can improve the visual experience by renormalizing surface irregularities to create a smooth, regular optic surface.
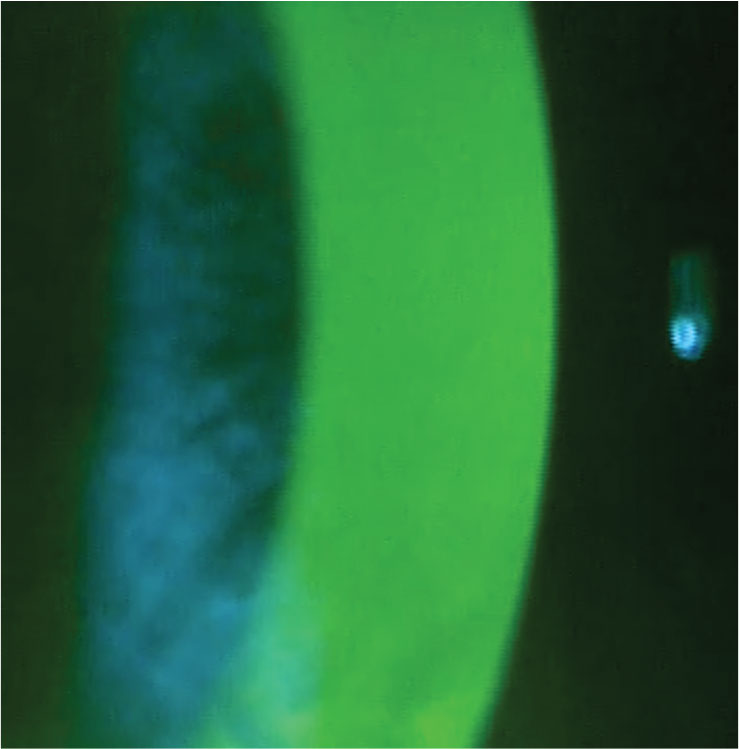 |
| Fig. 2. Normal fluorescein pattern over the cornea. Click image to enlarge. |
EBMD patients can minimize their need for glasses with the appropriate lens prescription. In mild cases, a soft contact lens can accomplish this. Although no clear guidelines exist for soft lens selection, higher modulus lenses, such as silicone hydrogel options, work well for these patients. With ever-advancing technologies, we now have a handful of daily disposable lens options that are silicone hydrogel. For more moderate or severe corneal irregularities secondary to EBMD, oftentimes a rigid surface is required to renormalize the optics entering the eye. Small-diameter gas permeable lenses work well for EBMD patients. If a patient has a difficult time wearing this lens, a hybrid may be an appropriate alternative. Scleral lenses are also an option and correct corneal irregularities through the post-lens solution reservoir and lens surface.
Case Study
A 45-year-old male presented with a chief complaint of blurred vision. He noted that everything “seemed blurry” and driving at night was becoming much more difficult for him. He reported that his glasses were re-made three times but the prescription was never correct. His manifest refraction was different than what was in his glasses. His VA was 20/25 OU.
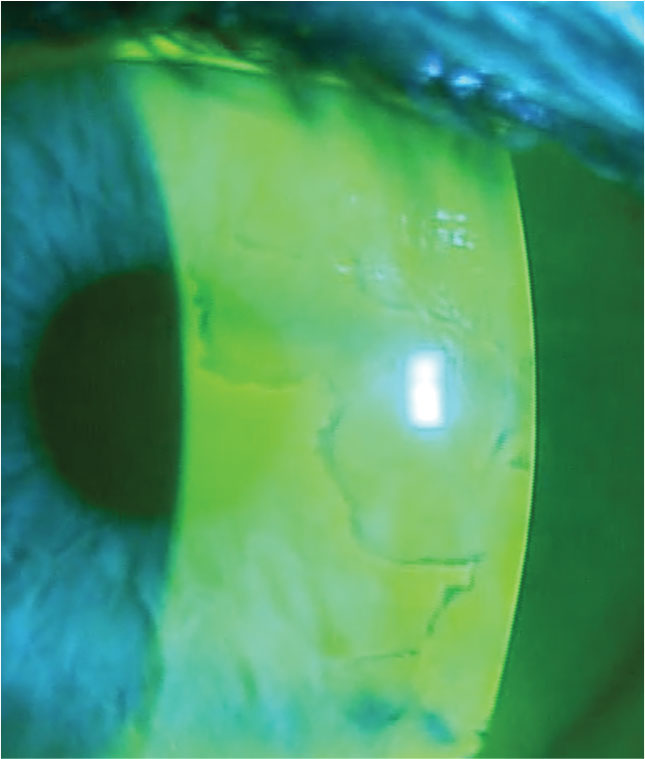
The posterior segment examination was unremarkable. The patient’s corneas were remarkable for significant mapping patterns that were visible when viewed with a cobalt blue light and a written #12 filter after fluorescein was placed on the surface of the eyes (Figure 2). EBMD patients have elevated regions on the corneal surface that appear darker or black when compared with the surrounding cornea because they are not adequately covered by the tear film (Figure 3).
The patient was educated on the reason for his reduced and variable vision. We discussed treatment options, and he wanted to proceed with lenses to improve his vision. He was fit with scleral lenses of the following parameters: -2.00/16.5mm diameter/4200 sagittal depth/toric scleral landing zone OU.
After the lenses were worn for 30 minutes, the central corneal clearances measured with a horizontal scan were 220μm OD and 240μm OS. There was adequate limbal clearance, and the landing zone was slightly flat in the steep meridian. The steep meridian was oriented vertically on the eye with a marking indicating it was located at the 6 o’clock position. The over-refraction was -0.50 SPH 20/15 OD and -0.25 SPH 20/15 OS.
 |
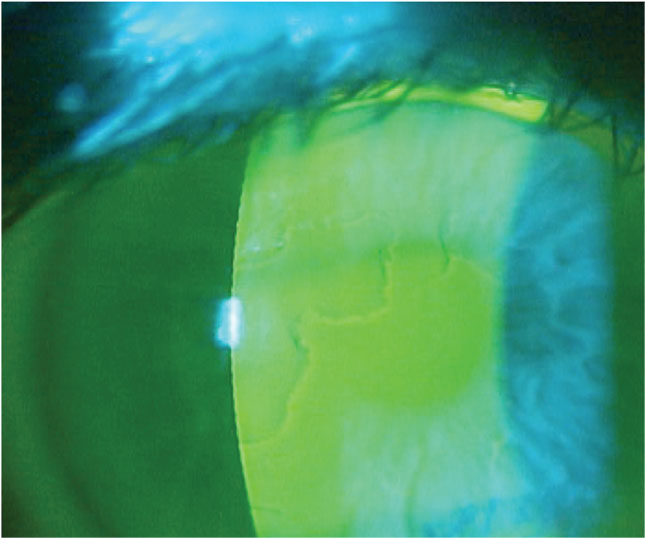 |
| Fig. 3. Negative staining associated with EBMD. Click images to enlarge. |
With the diagnostic lenses, the patient reported that his vision was better than it had been in years. He commented on how sharp everything looked. We ordered lenses with the appropriate powers and Hydra-PEG (Tangible Science) coating to optimize the hydrophilic properties of the lens surface and steepened the landing zone in the steep meridian by two steps.
With the lenses, the patient’s VA was 20/20 OU. In addition to improved vision and visual quality, the patient commented on how comfortable the lenses felt. He was taught appropriate wear and care practices before the lenses were dispensed.
The patient noted good comfort and vision at his one-week follow-up. His vision was 20/15 OU with no notable over-refraction. He continues to find success with scleral lens wear and experience clearer vision.
A specialty contact lens improved the quality of this patient’s vision and could be the solution for others like him. Practicing appropriate treatment methods, including advanced contact lens fittings and surgical remedies, presents an important opportunity to intervene in an EBMD patient’s life and help optimize their vision for the best outcomes. You just need to know where to start and how to proceed.
1. Hillenaar T, van Cleynenbreugel H, Remeijer L. How normal is the transparent cornea? Effects of aging on corneal morphology. Ophthalmology. 2012;119(2):241-8. 2. Waring GO 3rd, Rodrigues MM, Laibson PR. Corneal dystrophies. I. Dystrophies of the epithelium, Bowman’s layer and stroma. Surv Ophthalmol. 1978;23(2):71-122. 3. Labbé A, Nicola RD, Dupas B, et al. Epithelial basement membrane dystrophy: evaluation with the HRT II Rostock Cornea Module. Ophthalmology. 2006;113(8):1301-8. 4. Karpecki PM, Shechtman DL. Put an end to EBMD. Rev Optom. 2008;145(3). 5. Reidy JJ, Paulus MP, Gona S. Recurrent erosions of the cornea: epidemiology and treatment. Cornea. 2000;19(6):767-71. 6. Vo RC, Chen JL, Sanchez PJ, et al. Long-term outcomes of epithelial debridement and diamond burr polishing for corneal epithelial irregularity and recurrent corneal erosion. Cornea. 2015;34(10):1259-65. 7. Lee WS, Lam CK, Manche EE. Phototherapeutic keratectomy for epithelial basement membrane dystrophy. Clin Ophthalmol. 2016;11:15-22. 8. Miller DD, Hasan SA, Simmons NL, et al. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-35. |


